Introduction
Trigger finger is an uncommon entity in children. Synovial chondromatosis is a rare cause of trigger finger in all patient groups. Synovial chondromatosis is a proliferative condition in which cartilaginous nodules develop in the synovial membranes of joints, tendon sheaths and bursae.1 This has not been described to date in the paediatric population.
Case
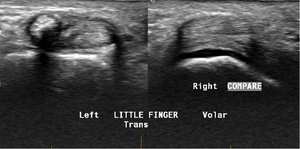
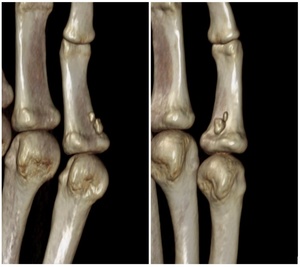
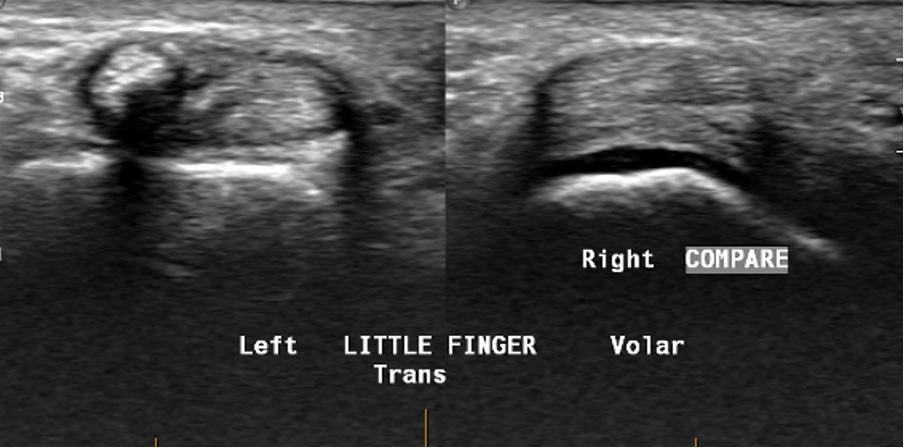
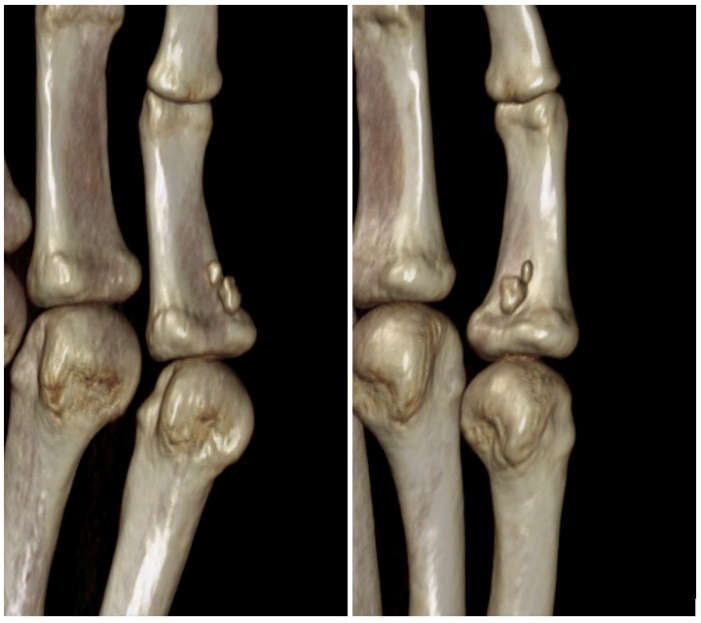
A 16-year-old boy presented with intermittent locking associated with pain of the left small finger. Examination revealed tenderness at the A1 pulley without crepitus, swelling or reproducible triggering. High-resolution ultrasound revealed multiple echogenic ossified bodies within the distal flexor sheath at the level of the A1 pulley (Figure 1). This finding was confirmed on CT (Figure 2) and MRI scans. Explorative surgery revealed that these ossified bodies, at the level of Camper’s chiasm (Figure 3), herniated through the flexor sheath with passive flexion. These lesions were removed and the flexor sheath repaired with 6-0 Prolene sutures (Ethicon, New Jersey, USA). The patient was commenced on an immediate active and passive exercise program and recovered with no complications. Histopathology from the intraoperative samples collected showed a well-circumscribed osteochondroid lesion, consistent with a diagnosis of synovial osteochondromatosis.
Discussion
Paediatric trigger finger is uncommon and considered to be a separate pathology to the more common paediatric trigger thumb. Overall, 54 per cent of paediatric trigger fingers present in a single digit and 29 per cent of patients with trigger finger have been reported to have a genetic abnormality.2 Potential causes includes anatomic variations and metabolic (eg, mucopolysaccharidosis), inflammatory, and developmental neurological disorders.3 Although described in adults, tenosynovial chondromatosis has not previously been described in a child. Tenosynovial chondromatosis is an uncommon condition that can involve the joints (articular) and/or the tendon sheath (tenosynovial), and the nodules commonly undergo secondary calcification and ossification. The aetiology is unclear, although tenosynovial chondromatosis may be associated with previous trauma.4 Milgram described the three distinct phases of synovial chondromatosis as:
-
active intrasynovial disease with no free loose bodies
-
transitional lesions with osteochondral nodules in the synovial membrane and osteochondral bodies lying free
-
multiple free osteochondral bodies with quiescent intrasynovial disease.5
Tenosynovial chondromatosis most frequently affects the hand and feet.6 Including this case, just 40 cases involving fingers have been described in the literature.6–16 These include 17 females and 21 males, ranging from 20 to 80 years of age with a mean age of 48 years. The right hand was more frequently affected than the left hand.8,12 There was one case of bilateral involvement and eight not specified. There have been 10 cases described in the thumb, four cases in the index finger, eight cases in the middle finger, nine cases in the ring finger and nine cases in the little finger. Patients usually present with no history of trauma. The most common symptoms are a painless swelling that develops over months to years and mild tenderness, however, triggering, carpal tunnel syndrome and stiffness have also been described.13
Plain radiography of tenosynovial chondromatosis may show extra-articular swellings, small or large calcifications, or ossifications. A CT scan may delineate the calcified or ossified bodies and cortical erosion. High resolution ultrasound is a useful investigation because it offers a dynamic assessment of the flexor tendons, revealing tendon nodules, thickening of the pulleys or abnormalities in the flexor sheath, such as in this case. An MRI scan is excellent for identifying soft tissue abnormalities; however, sedation may be required in younger patients limiting access to this mode of investigation. Triggering in multiple fingers in the paediatric patient is an indication for metabolic screening and genetic testing.
Spontaneous resolution of paediatric trigger finger with conservative management is difficult to predict. This is largely because previous papers assessing the outcomes of splinting grouped paediatric trigger finger with paediatric trigger thumb. Surgical exploration of the flexor sheath and tendons is indicated in cases of failed conservative management. Typically, surgery involves an A1 pulley release, ranging of the flexor tendons intraoperatively and inspection distally for the cause of triggering, including tendon nodules, abnormal flexor digitorum superficialis (FDS) slips, aberrant lumbrical insertions and adhesions. In this case, the cause of triggering was able to be localised to between the A1 and A2 pulleys, and an extensive surgical dissection was not required. For tenosynovial chondromatosis, complete excision of the loose bodies is the most common treatment, commonly resulting in resolution of pain and stiffness.
Macroscopic examination of the excised tumour often shows multiple white, lobular cartilage nodules that are easily separated from the synovial tendon sheath. These can number from single nodules to hundreds. Histopathologic examination generally reveals hyaline cartilage nodules surrounded by synovial membrane, mild chondrocyte atypia and, occasionally, mucinous changes, calcification and ossification.14 Malignant degeneration of tenosynovial chondromatosis to chondrosarcoma has been described in the hip and elbow (2.5%), but not the hand.17
Recurrence rates for articular chondromatosis range from 3 per cent to 23 per cent.14,18 Recurrence rates for tenosynovial chondromatosis based on the cases described in the literature are higher, with 14 cases having recurrence (36%) and seven cases having multiple recurrences (18%).
Conclusion
This case report describes a rare condition in the paediatric population. There are multiple possible causes of paediatric trigger finger and while tenosynovial chondromatosis is not the most common differential diagnosis, this case demonstrates the importance of a thorough clinical assessment and judicious use of imaging prior to proceeding to surgery. This approach to an atypical case improved the surgical planning and contributed to a positive functional outcome as described for the young patient.
Patient consent
Patients/guardians have given informed consent to the publication of images and/or data.
Conflict of interest
The authors have no conflicts of interest to disclose.
Financial disclosures
The authors received no financial support for the research, authorship and/or publication of this article.
Revised: January 27, 2024 AEST