The new Australasian Journal of Plastic Surgery will serve to document current and future generation’s ideas, innovations and achievements in plastic surgery. In the spirit of empiricism, a control is needed to compare and hence judge these future advances. This control or benchmark is our history to date; what we have achieved and who were those responsible.
What follows may not be proven truth, rather anecdotal slant and circuitous, non-malicious licence in the telling … ‘I’ve heard it said, at least I think that’s what they said, by whom I’ve forgotten…’ spices meals and makes history more digestible. Like much of plastic surgery itself, which is more art than science, comparisons with this ‘control’ are not evidence-based but a product of truths, myths and legends. Reconstructive surgery’s illustrious and dubious past is outlined and Australasian contributions are showcased in the context of international surgical evolution.
Tell all the Truth but tell it slant Success
in Circuit lies.—Emily Dickinson
Plastic surgery, aiming primarily to repair or disguise deformity, not surprisingly focused first on the face, particularly the nose. To disguise the amputated nose of the publicly branded adulterer in India, Sushruta (Figure 1), an Ayurvedic physician in 600 BC, divined the ‘Indian forehead flap rhinoplasty’ as well as alternative cheek flaps and free grafts. These and other reconstructive procedures are described in the text Sushruta samhita. In the 1500s following Columbus’ return from the Americas, the nose again branded the apparently new stigma of syphilis, which called for reconstructive camouflage.
The Indian flap was as yet unknown in Europe although the Sushruta samhita had been translated from Sanskrit to Old English in the 10th century1 and into Arabic in 1400. Gasparo Tagliacozzi (1545–1599), professor of surgery and anatomy at the University of Bologna, published De curtorum chirurgia per insitionem (‘On the surgery of mutilation by grafting’) in 15972 the first systematic treatise on reconstructive surgery, describing the tube flap method of nose repair from the inner arm which now bears his name. His description includes a delay procedure. Probably the first of many ‘stolen flaps’, it had been invented by the Branca brothers in Sicily more than one hundred years before. For several generations they guarded their secret method handing it down from father to son in a patent type proto-Mafioso fashion to be eventually succeeded by the family Bojani. Tagliacozzi had a few followers who repeated successful cases but despite the fame of the procedure today, over the course of time it fell into disuse. It was thought to be either impossible or fabulous and his success was eventually declared apocryphal.3
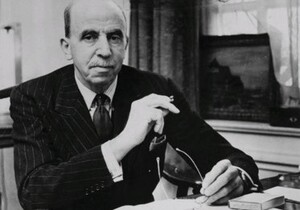
In the early twentieth century Jacques Joseph (Figure 2) published the modern closed rhinoplasty technique. A nasal hump was considered an ethnic stigma and rhinoplasty was sought by many of Berlin’s Jewish community. In 1916 the same year that Harold Gillies was commissioned to start his maxillofacial unit, Joseph became head of the newly established Department of Facial Plastic Surgery at the Charité, Berlin. Three years later he was named professor of surgery and anatomy at the Charité, that powerhouse chair of German Reconstructive surgery formerly occupied by Karl Ferdinand von Graefe, Johann Friedrich Dieffenbach and Bernhard von Langenbeck.
It had been offered to him earlier by Kaiser Willhelm on the condition that he converted to christianity but he refused. In 1931 he published his milestone book on plastic surgery—Nasenplastik und sonstige gesichtsplastik, nebst einem anhang über mammaplastik.4 Joseph gave the first description of the deltopectoral island flap for breast surgery and neck resurfacing5 which includes a copy of a picture from Carl Manchot’s 1889 atlas on cutaneous arterial anatomy,6 specifying the arterial basis for the flap. Manchot, while still a medical student, was tasked by his neurology professor to chart the course of the cutaneous arteries assuming that they followed the nerves, his primary focus of intent.
The nerves did not reliably follow arteries and the work, which proved to be a veritable treasure map for subsequent flap design, was shelved and thought to be lost to humanity by those who could only read English until its ‘rediscovery’ in the 1970s.
One hundred and sixty years later, Felix Behan, in Melbourne, showed that arteries did broadly follow the dermatome pattern and described his angiotome concept of skin blood supply7 on which much of his keystone designs are based. Behan quotes that at the conclusion of his presentation at the International Plastic Surgery Congress in Madrid, 1973, the Chair, Bill Manchester, said ‘I have no idea what you are talking about, but keep going.’ Joseph was blackballed by the establishment because of his cosmetic focus. In 1922 he established a large private clinic where he charged visitors to observe but no questions were entertained nor technical details explained.8 Joseph, himself Jewish, refused to leave Germany despite the looming Nazi oppression and died of a heart attack on his way to the operating room in 1934. The nose, again, wears the hallmark of society’s latest epidemic, cocaine. Ischaemic necrosis and perforation of the septum and hard palate are stigmata, albeit largely hidden, of cocaine addiction which are seen mostly in the very private clinics which serve celebrities, the rich and the famous.
Despite the work of Sushruta and Tagliocozzi, the history of surgery up until the latter half of the nineteenth century, with few exceptions, was essentially the management of traumatic wounds, fractures and amputations. It had been accepted since Galen’s edicts that such wounds must heal with septic discharge and that primary repair was impossible. Ambroise Paré (1510–1590) made fundamental observations on wound healing which he described in his book The apologie and treatise of ambroise paré in 1537. He described one of the earliest controlled experiments in surgery. In his first military campaign, having almost exhausted his supply of oil to cauterize wounds, he was forced to manage his patients in two different ways. One group was treated traditionally with oil and cautery, the other with a compromise digestive mixture of egg yolk, rose oil and turpentine without cautery. Returning in the early hours after a sleepless night fearing that his second group would be dead from infection, he reports:
[T]here, beyond my hope, I found those on whom I had used the digestive medication feeling little pain in their wounds without inflammation and swelling, having rested well throughout the night. The others on whom I had used the oil I found feverish, with great pain, swelling and inflammation around their wounds. Then I resolved never again to cruelly burn the poor wounded by gunshot.9
Paré also reports in his treatise that he did not persist with the balm recipe given to him by the surgeon to the King made from boiling puppies but instead advocated onions. His most famous phrase at the end of his treatise on wounds is ‘I dressed the wound and God healed him’. In the mercenary world of today this is more commonly stated as ‘God heals and the doctor sends the bill’.
From earliest times successful grafts of amputated tissue have been reported. The miraculous thumb replantation by St Julius is celebrated in a painting dedicated to the saint on the Isola San Giulio.10 Tom Gibson, in his excellent vignette on the history of grafting11 describes the most credible documented survival of a replant by William Balfour in 1814. Having previously reattached three of his own son’s fingers, he was presented with a finger amputation at the middle phalanx level. He took the precaution of obtaining signed affidavits from witnesses who saw the finger before and after his reattachment so as not to be marred by claims of charlatan, a common problem of that era. Balfour next saw his patient one month later and noted that the nail had fallen off and the skin had desquamated but the finger was ‘the handsometh the man has and had recovered both heat and sensation’. Gibson accredits Gottlieb Hoffacker, doctor to the dualists of Heidelberg, with the most critical and credible observations, and hence the most valuable, in predicting success of free grafting amputated parts. Quoting from Gibson:
He analysed reported cases, including 16 of his own amputated nose tips and lips sustained from duelling incidents. He observed that contrary to common understanding, completely severed parts were not yet dead and the most predictable parameters for rescue were washing away blood, oblique amputation, and delay. The latter allowed bleeding to stop, the severed part to relax from its contracted state to its original dimension and for its blood vessels to reopen allowing lymph fluid exuding from the cut wound to re-enter the now open ends. Replantation of the part facilitated accurate and maximum primary adhesion over the largest recipient area and favoured first, rather than second, intention healing. These parameters appear obvious today as those which would most favor graft take, but it is of note that at this period, nearly 40 years before Revedin reported his skin grafting in 1870, it was generally accepted that wounds could only heal by secondary intention.11
Jacques-Louis Reverdin, a young Genevan intern in the department of Guyon in Paris, was aware of Theodor Billroth’s observations that some wounds appeared to heal from expanding islands of presumed surviving epithelial remnants. He therefore implanted tiny pieces of skin from the arm to a thumb defect and obtained complete wound healing. In 1869 he presented his case to the Societe Imperiale de Chirurgie. It was the first demonstration that skin could survive for a period detached from the body, that it could regain a circulation and that once grafted it could expand. Reverdin returned to Geneva where with his cousin described myxedema and its association with thyroidectomy. Emil Theodor Kocher was the sole recipient of a nobel prize for almost parallel work on the thyroid, a prize that many believed should have been shared with the Reverdins. Jacques retired and dedicated himself to the study of butterflies. Louis Ollier and Karl Tiersch soon showed that larger grafts were also possible.
For many patients skin grafting from elsewhere on their body was anathema and unpopular because of the fears of pain and infection. The newly introduced general anaesthesia was too dangerous for such minor procedures and local anaesthetic would not arrive for another 20 years. So it was that a curious chapter in the history of plastic surgery, zoografting, came into being and is again described in a fascinating article by Gibson.12 This involved grafting of living tissue from one species to another, the recipient being human.
Frog skin was most popular because it was cheap and could be carried in the surgeon’s pocket13 although dog puppies, rabbits and birds were also tried. Although many of the writers wrote with extravagant and misplaced enthusiasm, remarkably some of those who performed the grafts, including Reverdin, believed that the grafts did survive and were responsible for their wounds eventually healing. Reverdin felt that, although surviving, they did not grow but stimulated the surrounding granulations to metamorphose into epithelium which then covered the wound.14 Allen quoted Stricker’s view of the existence of sexes in the tissues:
The colonies of epithelial corpuscles at the edges remain quiescent through lack of one sexual element, which the grafts no sooner supply than reproduction rapidly sets in, fertilisation being brought about through the medium of the fluid which bathes the surface of the granulations. If the sexual theory accounts for the process, the skin that grows after the application of the frog grafts must be of a new breed, a cross between human and frog epidermal elements.13
What we have now learned from immunology means that these were clearly false interpretations of apparently correct observations. Even before skin grafting, emboldened by the experimental parabiosis publications of Paul Bert (1863)15 who joined a rat to the back of a cat and demonstrated successful circulatory connections by instilling atropine into the rectum of the cat and observing dilatation of the rat’s pupils. Charles-Emmanuel Sédillot,16 French military physician and surgeon, in 1868, bound a human with an ulcerated hand to the freshly peeled abdominal region of a dog but the procedure failed because of excessive movement of the animal. He then advocated the spinal section of the animal for any subsequent trials but none were attempted. Dr E Lee in Chicago reported in the Boston Medical and Surgical Journal of 1880 (now The New England Journal of Medicine), that he had joined the burned back of a 10-year-old girl to flaps raised on the belly of a sheep. Both the sheep and girl were harnessed in a purpose-built cage. A correspondent of the journal wrote: ‘What now adds to the interest of the operation, and makes those who have watched the progress with anxiety hold their breath, is that the experiment bids fair to be a success.’ The correspondent gave a sequel to this piece of news in his next dispatch: ‘The experiment of Dr Lee at the county hospital of transplanting the flaps of skin of the sheep to a little girl failed by the death of the patient before the flaps were completely cut loose from the body of the sheep’. Finney in 1910 presented a case of a human pedicled flap joined to another human, which failed but ‘there is no reason why it should not succeed.’
It is now difficult to appreciate, but before Joseph Lister very few surgeons were prepared to inflict incisions through intact skin because of the extreme risk of wound infection, often fatal. Even the simplest procedure, like removal of a sebaceous cyst, might be followed by lethal erysipelas. At the Royal Melbourne Hospital in 1890 the death rate from opening the abdomen was almost 90 per cent.17 Although orthopaedic wounds and traumatic tissue loss were fair game for surgeons, the abdomen was not entered electively until 1879 when Robert Lawson Tait in Birmingham removed the gallbladder for infected stones. A year later he performed the first appendicectomy and in 1881 he was first to ligate the fallopian tube for ectopic pregnancy.18 In 1882 Billroth in Vienna successfully removed the stomach for a cancerous obstruction. This ‘master of men’ was the first surgeon to meticulously document his results including operative mortality, complications and five year reviews. A bizarre anecdote alleges that Billroth, despite his famed surgical technique accidentally poked his assistant’s eye out using the scalpel handle as a dissector with the blade uppermost. The assistant retired from surgery and became a green-grocer.19 In the light of the risks and technical challenges it was therefore extraordinary that Dieffenbach,20 influenced by von Graefe,21 in 1830, years before the resolution of the three scourges of surgery, pain, sepsis and bleeding, had the courage and deftness of hand to perform an array of innovative procedures for facial reconstruction. These included his square flap for the lip, V-Y flaps, modifications of the Indian rhinoplasty that had been recently reported by Carpue,22 the Italian method and new procedures for cleft palate and urethral fistula. He championed myotomy and tenotomy and somewhat overzealously proposed tongue myotomy as a solution for stuttering. Dieffenbach is the undisputed father of plastic surgery in Europe almost a century before Gillies and the foundation upon whom later surgeons stood.
Lister was a young spectator present in the theatre of Robert Liston, University College Hospital in London in December 1846 when a butler’s leg was to be amputated for osteomyelitis. Ether anaesthetic was planned, the first to be performed in Britain and only two months following William TG Morton’s initial demonstration in the Etherdome in Boston. Liston, awesome in frame and countenance and famed for his speed and showmanship, called upon the students ‘now gentlemen, time me’—28 seconds later the limb falls to the floor. Ironically the era of speed as the hallmark of surgical prowess ended with his stroke. Surgery could now be leisured and executed with care but sepsis was ever present and amputations carried a 50 per cent mortality. Lister, who never opened an abdomen in his career, experimented with carbolic acid for the treatment of compound wounds and reported in The Lancet in 1867 a reduction in mortality from 46 to 15 per cent. So convinced was he of the efficacy of his antiseptic precautions and carbolic spray that he risked malpractice when in 1870 he electively performed an open osteotomy of a malunited ulna. The wound, effectively converted into a compound fracture, healed by something rarely seen before Lister—it healed by first intention (primary healing).23
The surgeons of marvellous Melbourne in the boom period of the latter half of the nineteenth century were equally larger than life, fabulously rich, daring-do characters, whose homes and private hospitals still characterise the opulence of the Paris end of Collins Street. Surgery was a dangerous game and not for the faint hearted. Failure often resulted in the patient’s death and a murder charge could follow. The prize of success however was high and reputed fees for appendicectomy of one thousand pounds were probably true. Of greatest interest to plastic Surgeons is William ‘Jerry’ Moore whose life and times are told in Benjamin Rank’s fascinating book, Jerry Moore and some of his contemporaries.24 He was surgeon to St Vincent’s Hospital and then the Melbourne Hospital, and in 1899 wrote a textbook titled Plastic surgery, probably the first with such a title in the English language. Included in its chapters were examples of Thiersch grafting, Indian rhinoplasty flaps, and Wolfe’s full thickness grafts. JR Wolfe had come to Melbourne for a period in the 1890s and practiced in Moore’s rooms. The illustrative photographs show an astonishing mastery of the art, ‘a level far superior to the early years of Gillies at Sidcup where plastic surgery in Britain was being reinvented’.25
Moore was dogmatic, entirely humourless and unpopular but by power of persistence, introduced Listerian principles to Melbourne almost 30 years after its acceptance in Europe, ending the era of the ‘frock-coated’ surgeons and in doing so he reduced the death rate of abdominal surgery at the Melbourne Hospital from greater than 90 to less than 10 per cent. He was also responsible for ending scandalous public elections for appointment of surgeons to the hospitals. Hospitals were funded by public subscription and only subscribers could appoint the surgeons. This required an election akin to council elections of today and inevitably led to the public spectacle of fierce and brazen advertising, lampooned by cartoons in The Bulletin of the day. The notorious ‘Diamond Jim’ Beaney of the Melbourne Hospital allegedly hired an elephant which he proudly rode down Bourke Street parading his wares after being acquitted of a murder charge. One tactic was to offer the Chinese community a deal, sixpence to become a subscriber, and sixpence for their vote. In this way the electoral roll is said to have read like a Chinese telephone book. Because of Moore’s persistence medical appointments are now through the electoral college. With the emergence of abdominal surgery as a safer and potentially life-saving discipline, Moore’s focus on plastic surgery diminished and it was not until post-World War II that it would reemerge as a subspecialty.
Basil Kilvington26 was a surgeon at the Royal Melbourne Hospital and researcher at the University of Melbourne. In 1905 he published his work on nerve regeneration and repair in which he described neural sprouting and the concepts of neurotrophism before the writings of Santiago Ramón y Cajal. Cajal is given sole credit in this field which subsequently led to Rita Levi Montalcini receiving a nobel prize for the discovery of nerve growth factor as the trophic agent. Kilvington also performed nerve grafting and transfers and even advocated muscle grafts as nerve substitutes. His obituary reads typical of the period, dismissive of the research-minded who were thought less able than their clinical counterparts.
The Frenchman Alexis Carrel (1873–1944) must be included in the pantheon who powerfully influenced reconstructive surgery. He pioneered vascular surgical techniques, wound sterilization (Carrel/Dakin solution), tissue culture and, with the aviator, Charles Lindbergh, heart bypass. His work was a precursor to microvascular surgery and transplantation.
In 1902 Carrel (Figure 3) accompanied the moribund Marie Bailly to Lourdes and after witnessing her dramatic recovery reported to have changed from skeptic to believer after experiencing healing that he could not explain. He refused to discount a supernatural explanation and steadfastly reiterated his beliefs. The prevailing anti-clericalism of the universities at the time and the loss of reputation among his peers led to his migration to Canada to take up farming. Soon after however he was offered a position in Chicago and then at the Rockefeller Institute where he continued the research he had begun in France. This research with Charles Claude Guthrie led to him being awarded the Nobel Prize in 1912. In 1939 he returned to Vichy France and like many intellectuals of his time robustly took up the cause of eugenics. He argued for ‘an aristocracy springing from individuals of potential’. He was accused of Nazi involvement but died in 1944 before any trial could be held.
Harold Gillies from Dunedin studied medicine at Cambridge and trained in Otolaryngology. His career and contributions are well known especially to Australasian plastic surgeons. At the outbreak of war he was challenged with the daunting new injury of ‘trench jaw’ from flying shrapnel. Posted to Rouen and on leave in Paris, he visited the reclusive Hippolyte Morestin,27 an extraordinarily creative and underestimated figure who was treating the French war wounded and civilians. Gillies was mesmerised by what he saw and attempted a second visit but was summarily evicted. What he had seen however was a seminal influence on his career and after returning to England dedicated his unit to the cause of plastic surgery. Morestin was from Martinique and rumours of mixed blood, and octoroon, limited his prospects among the French elite. He described unique flaps, pioneered cosmetic surgery and was known as the ‘father of the mouths’ for his work on reconstructing the jaw and mouth. Perhaps because of his hermitic and eccentric behaviour, influenced by the loss of his father and 21 of his family in the eruption of Martinique’s Mount Pelée in 1902 which killed 30,000 people, Morestin strangely became lost to history despite having published more than 600 papers in accredited journals.
Another character of the period in Paris was Charles Auguste Valadier, a bon vivant, French/American dentist of disputed credentials who between the wars plied his mobile maxillofacial trade from the back of a converted Phantom Rolls Royce. Gillies had seen him treating the wounded but, unlike Morestin, Valadier was only too willing to share his secrets which allegedly included variants of the tube pedicle. Rumours also persist that Gillies stole the tube from the Russian, Vladimir Filitov, but it is clear from the writings of the American, John Staige Davis28 (Figure 4) that the concepts of transferring distant flaps, happily subsumed by Gillies as original to him, had multiple precedents (see below). Whoever planted its seeds, Gillies is responsible for its successful development, promotion and dominance in the English speaking nations as the method of transferring tissues until superseded by microsurgical free flap transfer.
To emphasise the truism that the victor writes the history, Gillies makes no reference to influential Europeans, nor does he acknowledge Johannes Esser, despite his island flap publications in English of 191729 and later being aware of his remarkable book, Biological or artery flaps of the face,30 which offers a myriad of one stage arterial based alternatives to the tube method. He dismisses its significance with the rather pompous comment that ‘[t]he ‘ideal biological’ outlook has overshadowed the meticulous refinement that is demanded of the plastic surgeon in the United States or British Empire the truth about these procedures as practiced by the English-speaking races is that the ideas are eminently sound when suitably modified’. Sadly the English speaking races to which he referred, including Australians, could also only read English. They remained blinded to the brilliant innovations and craftsmanship of Esser and other Europeans.
Esser was Dutch and was denied entry into the British army, so by default became the Gillies equivalent to the German/Austrian military of WWI. In photos of the period where Gillies boasted tubes hanging from patients’ faces and limbs in varying states of survival or decay, Esser had no tubes, only one stage islanded arterial flaps reconstructing the same defects. Gillies by his failure to recognise the significance of Esser’s arterialised flaps and Esser himself progressively becoming delusional and ignored, at one stage negotiating with Mussolini to develop a Mediterranean island into a centre for world plastic surgery, condemned plastic surgery to a 60 year stagnation employing semi-barbaric procedures, some of them extant in the Middle Ages. Enlightenment would not come until the era of microsurgery.
Our American colleagues may have a different slant on the plastic surgery hegemony presented above. John Staige Davis, their pioneer plastic surgeon and contemporary of Gillies in WWI, wrote a textbook Plastic surgery: its principles and practice one year before Gillies’ classic Facial plastic surgery of 1920. Their books and achievements are compared by Felix Freshwater31 who although American himself squarely accredits Gillies with the honours of clearer writing and far superior results (of note his article is published in the former British JPRAS and not PRS, perhaps not up to the expected standards of the latter). Davis, in an enlightening presentation to the American Surgical Association in June 1918, ‘The use of the pedunculated flap in reconstructive surgery’,32 describes its historical beginnings from Egypt and India to the Brancas, Vainio and Tagliacozzi, its demise and re-emergence (Indian flap by Carpue, 1814, London and the Italian flap, von Graefe, 1815, Berlin). He then describes the first description of the successive migration of a pedicled flap from the thigh to the cheek by Philibert Joseph Roux33 in Paris, in 1851. Davis accredits Maas particularly with perfecting the migration of pedicled flaps.34 William Stewart Halsted in 1897 gives the first description of ‘waltzing’ a pedunculated flap so that none of the original attachments remain.35 Davis’ presentation gives detailed technical insights including distinguishing arterialised flaps (temporal, angular forehead and abdominal) from those without a vessel and the method of intermediate transfer to the wrist. He makes no mention of Gillies. Did he believe that Gillies was simply an intermediary in the progression of plastic surgical advances?
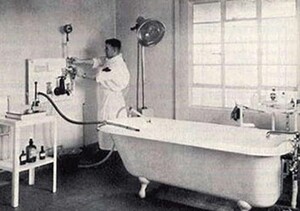
Archibald McIndoe from Dunedin via the Mayo Clinic arrived in England in 1930 with his wife and newly born child on the personal promise of an appointment with the prestigious Lord Moynihan. The good Lord said that he had never heard of him, and McIndoe, seeking urgent options, called on the graces of his cousin, Harold Gillies. Thus began his eminent career in plastic surgery. His fame spread due to his care of the burned airmen of WWII, not only because of his masterly reconstructions but for his focus on their social rehabilitation into the community. His patients proudly wore the membership badge of the ‘guinea pig club’. He introduced saline baths for burns (Figure 5) based on his observation that those who were shot down in the sea fared better than those over land. McIndoe also repopularized surgical correction of Dupuytrens by advocating wide exposure with Z-plasty closure to reduce the risk of nerve injury, a fate so common in earlier times that the operation had all but been abandoned. Ironically it is rumoured that when he favoured his other New Zealand colleague, Arthur Rainsford Mowlem to operate on his Dupuytrens, Mowlem promptly cut his digital nerves and forthwith retired to an olive grove in Spain. McIndoe’s clientele included the rich and famous including Ava Gardner and his mysterious death aged 59 and precipitous cremation without autopsy has led to several speculations, including the eleventh hour betrayal of his promised appointment to the presidency of the college of surgeons.
Gillies’ (and McIndoe’s) influence was global and their many trainees and observers, invited and uninvited included John Converse and Ralph Millard from the United States (the latter was told to leave but didn’t), Paul Tessier from France (who tried to leave but became so sick he had to stay), Jack Mustardé (née Mustard) from Scotland (who was told to leave and did) and of course many from the Commonwealth who became pioneers in their own cities. Most influential of these in the Australian scene were Benjamin Rank and John Hueston.
During their medical course both had tasted the spell of hand anatomy and function as dispensed by charismatic Frederick Wood-Jones, Professor of Anatomy at the University of Melbourne and in turn sought further training in the United Kingdom. An apocryphal story is that ‘Benny’ (Figure 6) was posted to Gillies’ unit at St James’ Hospital, Balham by default because the registrar scheduled to take up the position choked on his Christmas pudding. Rank thus came under the influence of the New Zealand triumvirate Gillies (Figure 7), McIndoe and Rainsford Mowlem. After distinguished war service he returned to Melbourne and established the discipline of plastic surgery in Australia including a formalised training program. His book with Wakefield and Hueston, Surgery of repair as applied to hand injuries36 changed hand management advocating primary repair of hand injuries as acute emergencies. His autobiography Heads and hands: an era of plastic surgery, published in 1987, highlights his career and times.37 Hueston won fame for his original observations and treatise on Dupuytrens contracture.38
The modern era of plastic surgery is the story of the coincidence of new technology (microscope and instrumentation) and a reawakening of the nature of the blood supply to skin. Early microvascular technical developments were driven by laboratory researchers to satisfy the need for small animal models of disease. Pre-eminent among them was Sun Lee, a Korean-born US qualified surgeon in Pittsburgh, who in 1958 succeeded in creating portacaval shunts in rats. This was followed by kidney and other organ transplants which were instrumental in the progress of transplantation research.
In 1961, Julius Jacobson,39 a vascular surgeon, realised the potential of the newly developed Zeiss ENT operating microscope to be used for clinical small vessel anastomosis and published reliable patency of 1.5 mm vessels. Harry J Buncke40 in San Francisco famously operated on small animals initially in his garage and soon reported successful rabbit ear and monkey toe to hand transfers. His early sutures were created by dipping nylon thread into molten metal and polishing the tip.
Clinical applications soon followed, replantation, initially by Susumu Tamai in Japan,41 in 1965, and unbeknown to the West, in China, and then a free abdominal dermo-fat graft transfer to the buccal mucosa which sloughed after three weeks (Antia and Buch).42 Buncke’s successful omentum to the scalp followed in 1968.43 Although as far as Buncke was concerned the story of free microvascular transfer was now complete; ‘…it succeeded and the rest is history’44; to others the elegance and mystique of the pure skin free flap remained the grail.
In 1972 in Glasgow, Smith, Foley, McGregor and Jackson described the groin flap45 based on a single vascular pedicle followed by McGregor and Gwynne Morgan’s (from Adelaide) concept of the ‘Axial and random pattern flaps’,46 acknowledging Stuart Milton’s recent work on pig flaps47 as the basis of this ‘new’ anatomical enlightenment. It is ironic that McGregor had previously described the forehead flap based on the superficial temporal vessels for oral reconstruction but seems not to have equated it with the axial pattern concept. In reality they had discovered what Sushruta, Manchot, Esser and Joseph had published long before. This territorial vascularization has since been definitively articulated by G Ian Taylor in his book, The angiosome concept and tissue transfer.48
With the blinkers now lifted it was obvious to many that a purely cutaneous flap based on these single source vessels was ripe for transfer. The race was set for the world’s first free skin flap transfer and the modern era of plastic surgery would begin. Bernard O’Brien at St Vincent’s and G Ian Taylor at the Royal Melbourne, would place Melbourne again at centre stage.