The history of plastic surgery and military surgery are inextricably entwined. The exigencies of war have led to tissue reconstructive techniques to meet the demand of very challenging tissue defects. Advances in plastic and reconstructive surgery date from the World War I and World War II through to the Arab-Israeli war and into the modern-day conflicts in Iraq and Afghanistan where the use of improvised explosive devices has led to uncontrolled, widespread tissue damage. The use of negative pressure vacuum-assisted therapy and the use of microsurgical reconstructive techniques have enabled these injuries to be treated effectively and the patient returned to a significant degree of normalcy.
The history of the speciality is summarised in the words of Gaspare Tagliacozzi (1545–1599), who in 1597 penned the words:
We restore, rebuild, and make whole those parts which nature hath given, but which fortune has taken away. Not so much that it may delight the eye, but that it might buoy up the spirit, and help the mind of the afflicted.1
The word ‘plastic’ is derived from the Greek word ‘plastikos’ and the Latin word ‘plasticera’, which both mean ‘fit for moulding’ or ‘to mould and shape’.
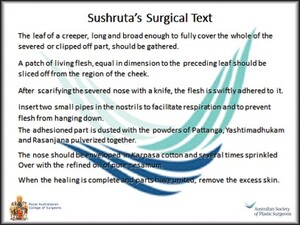
Recorded history of plastic surgery dates to 600 BC where Sushruta, a Hindu, is regarded as the ancient father of reconstructive surgery. In his writing Sushruta samhita he described the basic principles of the pedicle flap, sliding graft and particularly nasal and ear reconstruction. While it is commonly considered that nasal reconstruction using a forehead flap was the first recorded plastic surgery, it is clear from Sushruta’s surgical text (Figure 1) that his initial procedure, meticulously described, was of a nasolabial transposition flap.
Precious little seems to be recorded from those ancient Hindu writings to the first century when Celsus, a Roman, described the rotation flap and the advancement flap. He also described the four cardinal signs of inflammation—rubor, tumor, calor and dolor.
In the fourth century, the royal Byzantine physician, Oribasius, whose contributions to plastic surgery are found in his comprehensive medical encyclopaedia entitled Synagogue medicae, followed Celsus. He described in detail the use of bipedicle advancement flaps for skin defects around the area of the eyebrow, ala, cheek, nasal dorsum and tip, columella and ear.
In the era of the barber surgeons, Leonardo Fioravanti, a physician trained at the University of Bologna, played a crucial role in disseminating knowledge. Posing as a squeamish and uninformed observer, Fioravanti observed several nasal reconstructions performed by the Vianeos Family and later published these accounts for all to read in Il Tesoro della vita humana.
In the Renaissance Period, Tagliacozzi described detailed nasal reconstruction using a flap of tissue from the upper arm (Figure 2).
In 1818, the German surgeon, Karl Ferdinand von Graefe, considered by many at that time to be the finest surgeon in Europe, published his major work entitled Rhinoplastik.2 While the use of the term ‘plastic’ to describe reconstructive surgery was popularised 20 years later by Eduard Zeis in his book Handbuch der plastischen chirurgie, von Graefe was the first to reference it in print in 1818. In 1874, Karl Thiersch (1822–1895) was the first to widely popularise thin split thickness skin grafts. He used a long flat-bladed knife to harvest his grafts which were 1 cm in diameter. In 1875, John Reissberg Wolfe (1823–1904), a Hungarian ophthalmologist, reported the use of full thickness skin grafts in repairing defects of the lower eyelid. These were 2.54 cm wide and 5.08 cm long taken from the upper arm. Interestingly, Wolfe chose to practice in Melbourne for some time around the turn of the twentieth century.
World War I is considered as the true beginning of the modern speciality of plastic surgery. In particular, there was a great increase in the number of facial wounds due to trench warfare. Harold Gillies (1882–1960), a New Zealand otolaryngologist, established his own unit at the Aldershot Military Hospital in England to treat such wounds. Gillies’ tube pedicle techniques involved ‘waltzing’ the tissue from one part of the body to another, often using an intermediate carrier such as the wrist. Gillies summarised the activities at Queen Mary Hospital in Plastic surgery of the face, which was published in 1920.3
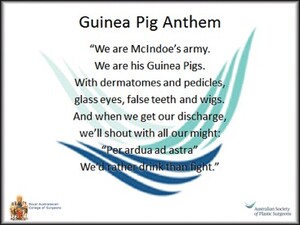
During World War II, Archibald McIndoe (1900–1960), who was Gillies’ cousin, came to prominence. He promoted early skin grafting of burns and introduced saline baths, and mechanical cleansing and dusting of the burn wounds with sulphonamides. He established a self-help support group called the ‘Guinea Pig Club’. The club was formed mostly by McIndoe’s patients at the Queen Victoria Hospital in Sussex during World War II. Initially, it was formed as a drinking club to help with patient rehabilitation and to create a relaxed environment. Their common theme was the guinea pig anthem (Figure 3). It was particularly relevant that this anthem alluded to the origins of most of the patients as RAF aviators.
The greatest advance in plastic surgery in the twentieth century was microsurgery. It was made feasible through the development of micro instruments, fine suture material, and the introduction of the binocular microscope by the Carl Zeiss Company in the mid-1950s. In 1965, Vahram Bakamjian described the deltopectoral flap and reintroduced arterial flaps based on the initial efforts of Johannes Esser. In 1970, SH Milton demonstrated that flap survival was based not on length to width ratio as had previously been taught, but rather on the blood supply that was incorporated into the flap.
The first free skin flap in an animal model was described by Goldwyn and colleagues in 1963.4 This was a groin flap in a dog. In 1973, the first successful free flap transfer in a human was performed by G Ian Taylor and Roland Daniel in Melbourne. In 1977, JB McCraw described myocutaneous flaps, followed in 1981 by Bengt Pontén, who described a fasciocutaneous flap. The first formal classification of muscle flaps was published in 1981 by SJ Mathes and F Nahai.5
Australia continues to remain at the forefront of both microvascular reconstruction and tissue regeneration. Taylor and Daniel, as previously mentioned, successfully transferred the first free groin flap in 1973. Bernard O’Brien and Wayne Morrison transferred a toe to form a wraparound flap for thumb reconstruction in 1980. Identification and publication of angiosome territories by Taylor in the 1980s was a sentinel advancement in plastic surgery. Since the early 2000s, tissue regeneration in vitro by Morrison continues to highlight Australia’s place at the forefront of advances in plastic surgery.
During the twenty-first century, advances in microsurgical free tissue transfer have matured to include the concept of flap pre-lamination, where implantation of tissue or other devices into a vascular territory is performed prior to its free tissue transfer. With the advent of reliable drugs to prevent tissue rejection, the performance of facial transplants has been made possible. The first of these transplants was in November 2005 in Amiens, France where a partial facial transplant was successfully completed. Full facial transplants have followed, enabling once horrendous defects to be reconstructed and return the patient to a normal lifestyle. Even penile transplantations have now been successfully performed and the procedure has been approved for United States war veterans.
The history of successful military surgery is embedded firmly within the history of the specialty of plastic and reconstructive surgery. Knowledge of this history is, I believe, the cornerstone to beginning a career within the specialty of plastic and reconstructive surgery.
Acknowledgements
All the text is the original work of the author, extracted from the Rupert Downes Memorial Lecture, which was his invited presentation at the RACS Annual Scientific Congress, Singapore, May 2014, during his tenure as Surgeon General Australian Defence Force Reserves.