Introduction
The GOSLON yardstick was developed in 19871 as a clinical tool to rate the dental arch relationships of patients with repaired complete unilateral cleft lip and palate (UCLP) in the mixed dentition. An assumption was made that the GOSLON score would predict the degree of difficulty to correct a malocclusion in a patient with a UCLP.1,2 The GOSLON yardstick uses a set of reference models to rate the degree of horizontal, transverse and the vertical inter-arch occlusal features present in standard dental models into one of five ordinal categories. The degree of horizontal discrepancy is measured by the overjet and is regarded as the most important feature in the assessment.3 The score is considered to be a reflection of the degree of maxillary growth disturbance resulting from the primary cleft repair4 thereby influencing a patient’s dental arch relationship.5
Because of its high intra- and inter-rater reliability1,6,7 and ease of use the GOSLON yardstick has become an accepted method for measuring cleft dental arch relationships in internal audits,8,9 as a method of comparing the treatment outcome between different cleft centres10–15 and as a proposed tool to measure the alteration of the dental arch relationship following changes in cleft treatment protocols.6
Despite its widespread use the accuracy of the GOSLON as a predictor of the need for growth completion orthognathic surgery is disputed. Suzuki found no correlation between GOSLON scores at age then and maxillofacial growth between five and age 15.16 The aim of this paper was to assess how accurately a GOSLON score at age nine predicted the need for growth completion orthognathic surgery as assessed by our unit’s clinical criteria for a patient with a UCLP. Patients considered for orthognathic surgery are referred to the unit’s multidisciplinary combined orthognathic clinic involving plastic and craniofacial, oral and maxillofacial, ear nose and throat surgeons, dental specialists (orthodontists, periodontists, prosthodontist and paediatric dentists), speech therapists, cleft specialist nursing and craniofacial scientists. The decision to recommend surgery is made after balancing potential risks and potential benefits for each individual patient.
Methods
A review of a retrospective cohort of consecutively treated patients born with complete UCLP between 1982 and 1995, managed from birth to maturity by CLP unit at the PMH. This was undertaken as part of extensive cleft audit undertaken by the PMH cleft unit (Approvals PMH Quality Activity 5806).
All patients included in the study had study models taken at nine years (± 3 months) and were subject to clinical review within the unit during adolescence and at growth completion. Patients with a diagnosed syndrome or incomplete records from age nine were excluded from the study. Patients who had undergone orthodontic appliance therapy or alveolar bone grafting prior to having dental models at age nine were also excluded as such interventions may positively influence the GOSLON yardstick score.17 Sixty six patients fulfilled these criteria. From this cohort 38 patients who had had a lateral head X-ray at age 18 that was suitable for analysis were subject to objective cephalometric appraisal for candidature for orthognathic surgery as proposed by Daskalogiannakis.
All UCLP patients born between 1982 and 1995 were identified from the database of the CLP unit, PMH. The year 1995 was chosen as the endpoint for data collection as these patients have now attained skeletal maturity. Examination of the clinical records, birth photographs and neonatal palatal impressions was performed to confirm all patients were born with non-syndromic complete UCLPs.
Data collected included age at the time of lip and palate repair and the type of lip and palate repair. Patients were referred for consideration of orthognathic surgery when a patient had a malocclusion where achieving a positive overjet and overbite was beyond the scope of routine orthodontic correction or if the concave facial profile was of aesthetic concern to the patient. The final decision on a patient’s need for orthognathic surgery was made in a combined clinic setting where all involved clinicians provided input. Lateral cephalometric radiographs, clinical photographs, 3D surface scans (3DMD), dental study models, speech assessments and sleep studies were routinely reviewed as a part of the decision making process. Cephalometrics were reviewed as part of this assessment but the need for surgery was not based on a set of cephalometric criteria as reported by Daskalogiannakis.
Two ‘raters’ experienced in the use of the GOSLON yardstick rated the dental study models taken at age nine. Raters were blinded to patient details and did not collaborate when scoring. The process was repeated two weeks later with the dental models reallocated in a randomised order.
The linear weighted Kappa statistic was calculated using Microsoft Excel (Version 14.5.5) for the GOSLON scores to determine the intra-rater agreement and inter-rater reliability (Table 1). The strength of agreement was determined using the scale in Table 2, which was adapted from Landis and Koch.18
Available digital lateral cephalometric radiographs taken at age 18 (n = 38) were imported into Dolphin Imaging (Version 11.9, Release Build 24) where a comprehensive list of commonly applied landmarks were indicated by one operator (MW). From these indicated landmarks the software calculated inter-landmark Euclidean distances, angles and ratios of cephalometric variables consistent with those reported by Daskalogiannakis as ‘objective’ measures of the need for orthognathic surgery. These were based on the satisfaction of all three of the following criteria, a:
-
ANB angle of -3 degrees or lower
-
Harvold unit difference (CoGn-CoSn) of 34 mm or larger and
-
Wits appraisal result of 25 mm or lower (B-point ahead of A-point).19
Results
Sixty-six unilateral cleft lip and palate patients, 38 male and 28 female, fulfilled the inclusion criteria for this study. The cleft side ratio was L:43 and R:23.
Our protocol for UCLP patients includes presurgical orthopedics to narrow the alveolar cleft and improve symmetry of the alar bases. A passive plate and external strapping were used. Lip and primary palate repair was performed at a mean age of 3.4 months (SD 1.0). The lip repair was Tennison-Randall repair in 61 patients (92.4%), Millard repair in five patients (7.6%). Palate repair was performed at a mean age of 8.9 months (SD 3.2). Hard palate closure utilised Veau, Wardill-Kilner or von Langenbeck flaps. Alveolar bone grafts were subsequently performed in 62 patients (94%) at a mean age of 10.4 years (SD 1.0).
The GOSLON yardstick scoring showed good intra-rater agreement and inter-rater reliability (tables 1 and 2).
PMH GOSLON yardstick scores and referral status
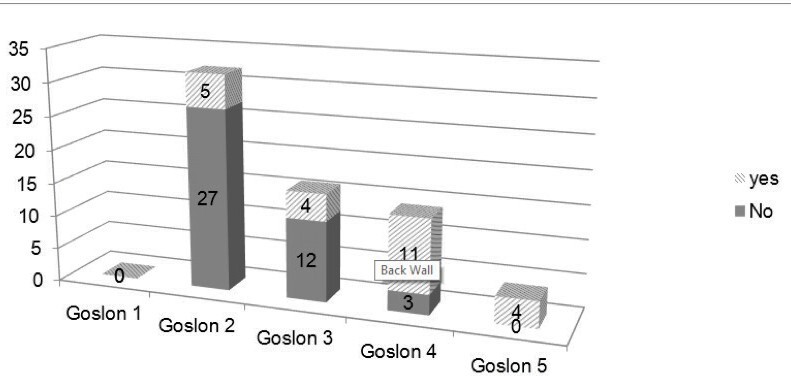
The distribution of GOSLON yardstick scores for the 66 patients is presented in Figure 1. We have previously published a review of our treatment protocol and GOSLON scores.8 Twenty four patients (36.6%) were referred for orthognathic surgery at growth completion.
Five of 32 patients (15.6%) with a GOSLON score of two were referred for orthognathic surgery. This increased to four of 16 patients (25%) with a GOSLON score of three, 11 of 14 patients (79%) with a GOSLON score of four and all four patients (100%) with a GOSLON score of five were referred for orthognathic surgery at growth completion (Figure 1). One patient under-went orthodontics and osseointegrated implant supported face-mask therapy at age 12 achieving a positive overjet but a persisting class III tendency at growth completion.
All remaining patients underwent conventional orthodontic treatment for correction of their malocclusion.
Cephalometric outcomes at age 18
A total of 38 of the original cohort of 66 patients had a suitable cephalometric radiograph at age 18 available for the study. Seventeen of this group (44.7%) were referred for orthognathic surgery based on results of our combined orthognathic clinic. Only eight of these patients (21%) fulfilled the cephalometric criteria of Daskalogiannakis and Mehta.19 None of the patients that were not referred for orthognathic surgery based on our combined clinic review (n = 21) fulfilled the objective cephalometric criteria for orthognathic surgery. Statistically significant differences (two tailed t-test assuming unequal variances, perormed in Excel 2010, Microsoft Coorporation) in ANB angle (p < 0.05) and Wits appraisal (p < 0.05) but not Harvold unit difference (CoGn-CoSn) (p = 0.29) were recorded for the clinically assesed orthognathic surgery candidates compared to those who were not referred (see Table 3 for details).
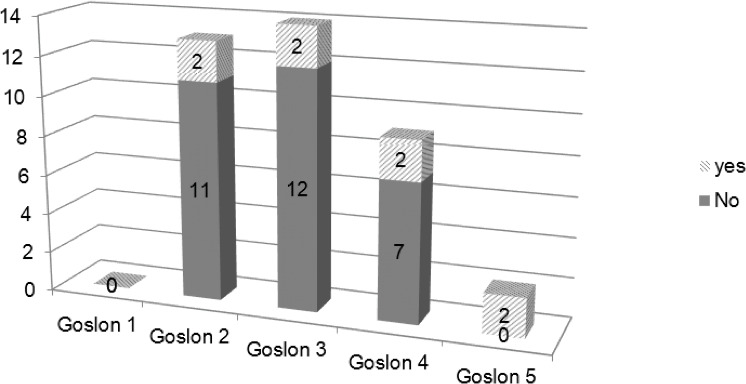
The ratio of objective cephalometric based surgical referrals to GOSLON categories (Figure 2) differed to those observed in the clinical referral cohort (Figure 1) for GOSLON three and four categories where patients with a cephalometric indication for orthognathic surgery were substantially under-represented at 14.3 per cent and 22 per cent respectively.
Discussion
The GOSLON yardstick was developed to provide standardised assessement of the dental arch relationship in patients with a UCLP in order to be a research tool to compare the longitudinal outcomes of surgical technique, surgeons and institutions.6,17,20 Though the assessment of a dental study model is not based on precise measurements it has proven to be a robust tool for the assessment of cleft outcomes. This was demonstrated by the good intra- and inter-rater agreement achieved by the raters in this and many other studies (Table 1).1,6,7,15,21,22
It was inferred that a GOSLON yardstick score would predict the future treatment required to correct the cleft malocclusion.1,23 Predicting the treatment requirements within a cleft unit is not only of value for audit purposes but also as an aid to calculating the resources necessary to provide ongoing treatment. The higher a GOSLON score the more complex and difficult the treatment anticipated to correct a UCLP related malocclusion. This was reflected in this study with a progressively increasing requirement for orthognathic surgery as a patient’s nine-year-old GOSLON yardstick score increased (Figure 1).
Five patients with a GOSLON score of two, which is an indication of a normal overjet and overbite, at age nine were however referred for orthognathic surgery in combination with orthodontic treatment to correct their malocclusion. Examination of the clinical records indicated that for one patient orthognathic surgery was required to correct a unilateral crossbite caused by collapse of the minor segment, another for occlusal cant the remaining three experienced a progressive development of maxillary retrusion. This outcome is a reflection of the higher weighting given to the overjet observed as compared to the presence of a posterior crossbite or open bite tendency when examining dental models of a UCLP patient to assess the GOSLON score.24
The referral of eleven of the 14 patients (78.6%) with a GOSLON score of four and all patients (100%) with a GOSLON score of five for orthognathic surgery illustrates that the presence of a large reverse overjet at age nine is an accurate indication of the requirement for future orthognathic surgery. Two individuals with a GOSLON score of four who required orthognathic surgery to correct their malocclusion were not offered treatment due to poor compliance. One patient with a GOSLON score of four did not need orthognathic surgery for correction of his malocclusion at growth completion as he had undergone protraction of the maxillary complex by osseointegrated implant supported face mask therapy at age 12 in conjunction with orthodontics.25 Had this patient not undergone this treatment he would probably have required orthognathic surgery at growth completion. Two other patients that had also undergone osseointegrated implant supported maxillary protraction did not achieve sufficient advancement to avoid orthognathic surgery at growth completion. No other patients in this cohort underwent this treatment.
A degree of maxillary growth impairment is a feature of most UCLP patients. Review of long-term growth outcomes provides evidence to elucidate treatment protocols and techniques that effectively reduce the severity. Many collaborative inter-centre studies have demonstrated differences in respect to mid-facial growth outcomes.26,27 The need for orthognathic surgery to correct cleft related growth deficiencies is also an issue for all cleft units. The rates of orthognathic surgery range from approximately one in eight to one in two patients.19,28–33 Differences in inclusion criteria, thresholds of acceptability, availability of services, incidence of skeletal malocclusions in the unit’s population group and funding support for orthognathic surgery make comparisons of orthognathic surgery rates between cleft units of little value as indicators of long-term growth outcomes. Standardised ‘objective’ criteria for orthognathic surgery facilitates inter-centre comparison but may underestimate the number of patients requiring such surgery.
The GOSLON yardstick has been extensively used as a tool for inter-centre cleft outcome comparisons by stratifying the severity of the dental alveolar discrepancy in the mixed dentition. This index has been used to assess efficacy of cleft management protocols in minimising growth disturbance and combined orthodontic surgical requirements1 The relationship between GOSLON scores and growth completion outcomes has been inferred but not extensively explored.
In 2014 Suzuki and colleagues found that a GOSLON yardstick at age 10 may not predict maxillofacial morphology in adulthood.16 They found that growth of the maxilla was similar in all five GOSLON groups between age five and 15. Mandibular growth however did differ with more anterior growth of the mandible with higher GOSLON scores. Their study reported on cephalometric outcomes rather than differences in orthognathic surgery rates for patients with differing GOSLON scores.
The authors investigated the relationship between GOSLON scores at age nine and the percentage of patients referred for orthognathic surgery to correct a dentofacial anomaly. We found an increased incidence of referrals for patients with higher GOSLON scores (Figure 1). This pattern differed when utilising an objective cephalometric appraisal that considers variables that best describe jaw relationships19 at age 18, where we found a relative reduction in surgical candidature in GOLON three and four categories (Figure 2). This outcome may indicate that the clinical assessment adopted by the unit’s multidisciplinary clinic has a lower referral threshold than one utilising only an objective cephalometric appraisal. The distributions of cephalometric variables used in the objective appraisal proposed by Daskalogiannakis, ANB angle, Harvold unit difference and Witts appraisal all had mean values below the threshold for the clinical referral group. The means of the distributions for the non-referral group were outside thresholds except for the Harvold unit difference (Table 3). These outcomes are suggestive that the clinical assessment for surgical candidature has a relationship with cephalometric variables used in an appraisal when dealing with population data, however on an individual basis lacks discriminatory power.
The frequency of complete UCLP patients requiring orthognathic surgery for this cohort of patients was 36.6 per cent. This being comparable to those reported from other centres.19,31,33,34 In Australia patients requiring combined orthodontic and orthognathic treatment to resolve their cleft related dentofacial deformity have their treatment cost fully covered by our Medicare system. This enables more patients to undergo treatment compared to some other countries where patients are required to cover some, or all, of the treatment costs.
The ability of GOSLON to predict probability of the need for orthognathic surgery, based on a clinical team assessment, is particularly evident for patients with scores of four and five (Figure 1). This was confirmed by cephalometric appraisal for category five only (Figure 2). This outcome in part validates the GOSLON yardstick9 as a measure of cleft outcome when scored at age nine.
The identification of patients in the early mixed dentition who are likely to require future orthognathic surgery may result in the avoidance of early orthodontic treatment that may need to be repeated at growth completion to prepare the patient for surgery. The caveat to this is that mid-facial growth in adolescence can be difficult to predict. We had patients with GOSLON scores in the mixed dentition that could be considered as a low risk for requiring orthognathic surgery become candidates as well as some patients recovering from a poor prognosis at age nine. Considerable effort is required to more fully understand these growth disturbances and which treatment protocols result in best growth outcomes.
Conclusion
In conclusion, the results of this study suggest that a GOSLON score at age nine is a good predictor of the future need for orthognathic surgery based on clinical criteria for patients with UCLPs. It may be a useful tool to predict the future treatment requirements, and therefore resources required, to manage UCLP patients within a CLP unit. Patients with GOSLON scores of four or five are most likely (79% and 100%) to require growth completion orthognathic surgery and can be identified in the early mixed dentition preventing unrealistic orthodontic treatment interventions. This could also assist with the education of both patients and their parents as to likely treatment requirements.
Disclosure
The authors have no conflicts of interest to disclose.
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
Revised: January 16, 2018 AEST