Introduction
The outcome after a burn injury can be judged against objective measures such as mortality. However, in practice, burn outcome is measured against morbidity factors with the long-term outcome relating to the ongoing issues that patients take with them for the rest of their lives. The major form of morbidity, both physical and psychological, relates to the severity and extent of scarring that remains once the scar maturation process is complete.
The long-term severity of scarring is related to several factors: the severity of the initial injury, the effectiveness of first aid and the acute management of the burn and secondary reconstructive options. It is therefore the quality of the scarring that determines a patients’ long-term outcome. Our research confirms that the quality of scarring can be predicted by the healing time and that the outcome of scarring can be improved by better acute burn management.
Healing time
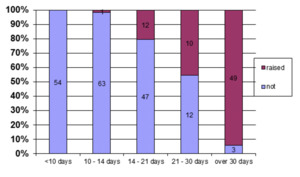
In 2006 we provided data from a large cohort of children with a scald injury, mapping their healing time to scar outcomes.1 Although it was a retrospective study, it demonstrated a clear link between hypertrophic scarring and prolonged healing times (Figure 1). We demonstrated this link in both patients treated conservatively and those who underwent split skin grafting.
Patients who had split skin grafts and healed early fared better than those who had late grafting. However, patients who underwent a skin graft, even if performed earlier, had more scarring than those who healed quickly without a graft.
What determines the healing time?
Factors such as the depth of injury are primarily determined by the severity of the injury itself but there is good evidence that timely and effective first aid can stop the ‘cooking’ effect and potentially save some of the tissue in the zone of injury.
The depth of the dermal injury determines the number of adnexal elements that remain viable—these include hair follicles and glands and are important because they provide epidermal cells that can migrate onto the surface and heal the wound. The more superficial the injury, the more adnexal elements remain, the more quickly the wound heals and the better the outcome. If the dermis is damaged at a deeper level, then the outcome is worse due to slow re-epithelisation and issues such as contraction can also become a problem. The best outcomes for deeper injuries arise from early re-epithelisation using split skin grafts or other autologous cell techniques onto viable deep dermis or from the use of dermal regeneration templates, such as INTEGRATM (Integra LifeSciences, 311 Enterprise Drive, Plainsboro New Jersey, USA) covered with autologous epidermal graft. The traditional techniques of full thickness excision and split skin grafting are very effective at closing the wound quickly but often produce less favourable scarring outcomes in the long-term.
Other factors such as medical comorbidities, nutrition and smoking may also prolong healing and these too can be managed to reduce overall healing time.
As surgeons we either strive to preserve viable dermis and provide the best wound environment possible to facilitate re-epithelialisation or decide early to excise and replace the epidermis and dermis if required.
Strategic planning
The strategic plan that we have developed aims to reflect our understanding of the scarring process, to keep healing times as short as possible and to actively treat those at high risk of aggressive scarring. It incorporates the following elements:
-
promoting effective first aid
-
accurately judging depth
-
removing dead tissue while conserving dermis
-
grafting early when indicated
-
optimising dressing changes
-
preventing infection
-
anticipating scars and pre-treat with aggressive scar therapy and pressure garments.
Assessing the intermediate depth of a burn injury
The most difficult group of patients to manage are those with intermediate depth injuries. They comprise a diverse group who have suffered scald and flash/flame burns and such patients can challenge the most experienced of surgeons. The key decision in managing their care is whether to graft or not. The changing perfusion in the zone of injury in the first 24 hours makes accurate determination of viability difficult, either by the eye of the experienced burn surgeon or by instruments such as the laser Doppler imaging (LDI). If there is doubt, then the wound should be reassessed 48 hours after the injury and an objective method used to assess dermal blood flow. Dermal blood flow, be it assessed by clinical capillary refill or the flux reading of the LDI, can then be related to the healing potential of the burn and therefore direct management according to either a conservative or surgical approach. Any surgery should be carried out as soon as practical to preserve as much viable dermis as possible.
Dermal preservation surgery
Techniques to remove necrotic tissue while preserving viable deeper dermis can be achieved surgically by using traditional graft knives such as the Watson knife or finer instruments such as the Goulian knife. More recently, surgical instruments such as the Versajet hydrosurgery system2 have been developed to allow even finer debridement while chemical debriding agents such as NexoBridTM (MediWound Ltd, 42 Hayarkon Street, Industrial Zone, Yavne, 8122745, Israel) are able to selectively remove necrotic tissue while preserving the three-dimensional heterogeneity of the viable wound surface. This can then be dressed with a biological dressing while awaiting re-epithelisation or resurfaced with split skin autograft if the deeper dermis is exposed.
Biological dressings
For partial thickness burn injuries there are a wide variety of biological dressings available ranging from cadaveric allograft, which requires specialised storage, to off the shelf products such as pig skin, BiobraneTM (Mylan/UDL, Robert J Coury Global Center, Mylan,1000 Mylan Blvd, Canonsburg, PA 15317, Pennsylvania, USA) and SUPRATHEL® (Polymedics Innovations GmbH, Heerweg 15D, 73770 Denkendorf, Germany). These provide a good physiological environment by adhering to the wound, reducing fluid loss and pain and requiring no removal during the healing process. They can reduce healing times but they are expensive and require thorough debridement prior to application—so will usually be applied under anaesthesia. In our paediatric patients we apply BiobraneTM if a child has a greater than 4% total body surface area (TBSA) confluent superficial partial thickness burn injury as this is considered a large enough area of burn to justify the risk of general anaesthetic. We use prophylactic antibiotics in the early stages as infection can potentially occur between the dressing and the skin.
Non-biological dressings
Conventional dressings are used for smaller or more superficial burns and a variety of products are available. Our current first line product for paediatric patients is AQUACEL® Ag Extra™ (ConvaTec Global, 3 Forbury Place, Forbury Estate, 23 Forbury Road Reading, Berkshire, RG1 3JH, UK) which is a silver hydrofibre dressing. It adheres to the surface of a superficial partial thickness burn injury, providing a degree of antimicrobial effect when the exudate is wicked into the dressing without releasing a high concentration of silver onto the wound surface that would otherwise delay re-epithelialisation.
Post-healing protocol
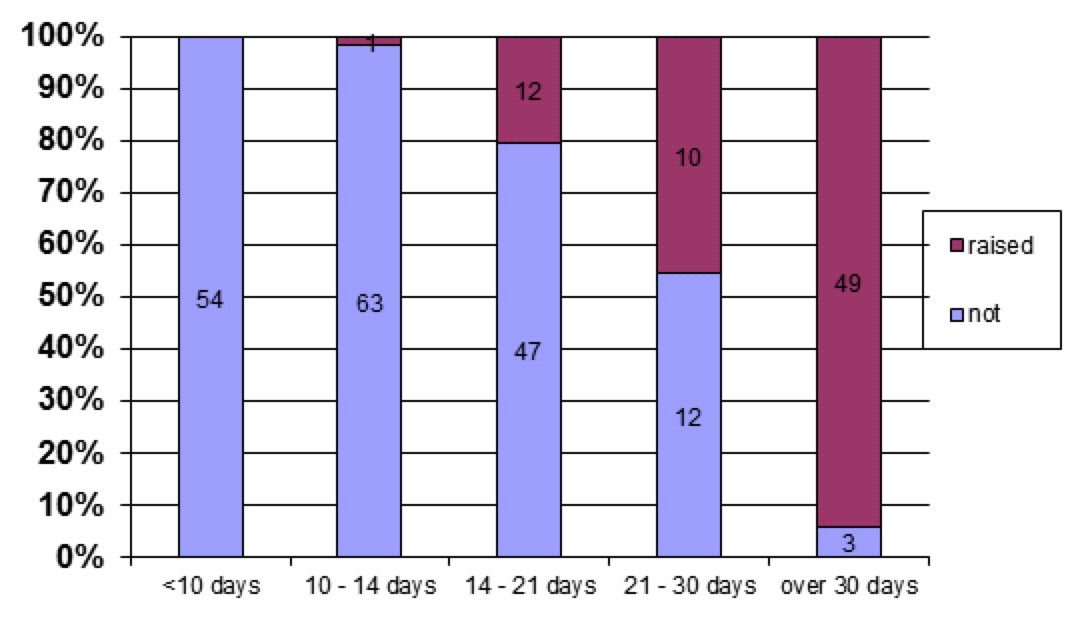
After the patient has healed they are placed into one of three groups: if fully healed by 14 days, the patient is discharged from the dressing clinic with an advice sheet; if healed between 14 and 21 days, the patient is discharged with information and advice to return if any scarring appears (there is no routine follow-up but easy access to the clinic if required); if it takes more than 21 days to heal, or grafting was needed, patients are pre-treated with active scar therapy including prophylactic pressure garments in most cases. They are then actively followed up in outpatient clinics.
Does it work?
After revising our approach since the 2006 study,1 we reviewed a further group of children.3 Lower overall rate of hypertrophic scarring was seen and, for corresponding healing times after injury, hypertrophic scarring rates were halved in comparison to the 2006 cohort. We have demonstrated that the use of a structured approach for paediatric burns (Figure 2) has improved outcomes with regards to healing times and hypertrophic scarring rate. This approach allows maximisation of healing potential and uses aggressive prophylactic measures.
Conclusion
Early decision-making and good strategic management of acute burns can improve the long-term outcome. Although our study groups comprised less complex paediatric cases, we apply the same principles in managing adult patients. Elderly patients do not produce hypertrophic scars with delayed healing so accordingly there is no indication to prioritise excisions for this group.