Introduction
Dupuytren’s disease is a common, benign fibrotic disease resulting in finger flexion contractures.1 This can lead to significant functional hand impairment through decreased range of motion,2 with patients thus seeking treatment.3 As no cure currently exists for Dupuytren’s disease, treatment primarily focuses on four characteristics identified by Tubiana in 1975 ‘to correct deformity, avoid complications, shorten post-operative recovery, and prophylactically prevent recurrences’.4
Surgical correction of Dupuytren’s disease via fasciotomy, fasciectomy and dermofasciectomy has been the mainstay of therapy over recent decades.5,6 Percutaneous needle fasciotomy is advantageous due to rapid recovery times and the ability for outpatient management, thus reducing costs.7 However, as the cord is not excised during fasciotomy, recurrence rates are higher compared with fasciectomy or dermofasciectomy.8 These two more radical treatment options are associated with a lengthier recovery time but a lower recurrence rate. Furthermore, adverse effects such as pain, infection and nerve injury have a higher likelihood.6
In 2013, collagenase clostridium histolyticum (CCH) was licensed by the Therapeutic Goods Administration in Australia for the treatment of Dupuytren’s disease. CCH is delivered as an injection into the palpable cord, containing a fixed-ratio solvent of two enzymes, clostridial type I and II collagenase. These enzymes combine to hydrolyse the pathological type I and III collagen.9 More than 24 hours post injection, the finger is manually manipulated by a hand surgeon. This straightens the affected digit by disrupting the cord responsible for causing contracture.10
Other non-surgical options explored for treatment of Dupuytren’s disease include pharmacological therapy (steroid injections, vitamin A or E application, 5-fluorouracil treatment), physical therapy and radiotherapy.11 Radiotherapy is hypothesised to inhibit the early proliferative phase of Dupuytren’s disease, but the evidence and its use are currently limited.12 Steroid injections are thought to reduce fibroblast proliferation and increase apoptosis during the development of Dupuytren’s disease, although the clinical use is still minimal.13
This review seeks to examine the current evidence regarding the increased use of CCH in the management of Dupuytren’s disease. We particularly explore:
-
The effectiveness of CCH for patients with Dupuytren’s disease
-
The safety of CCH for the treatment of Dupuytren’s disease
-
The likelihood of recurrence for patients with Dupuytren’s disease who have been treated by CCH and surgery.
Methods
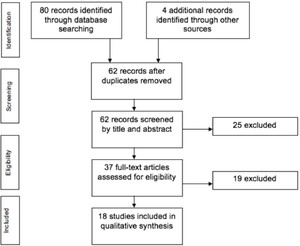
A literature review was undertaken, with study inclusions comprising English language, peer-reviewed journals and available full text. We included randomised controlled trials, observational studies and case series published after the year 2000. Additional studies were sourced via bibliographic linkage. Search terms included ‘Dupuytren disease/contracture’ and ‘CCH/Xiaflex’ mapped against effectiveness, recurrence and safety (see appendix). Papers included analysis of effectiveness, safety and/or recurrence for adults with Dupuytren’s disease receiving CCH. Editorials, case reports and non-English studies were excluded.
Data were collated and synthesised using the Cochrane Collaboration data collection tool.14 A qualitative analysis of the data was undertaken.
Results
Eighteen studies were eligible for full review after deletion of duplicates and application of exclusion criteria (Figure 1).15 Of these 18 studies, four were randomised controlled trials, three were open-label, nine were observational and the remainder were case series. Consequently, four studies were level therapeutic I, one was therapeutic II, three were therapeutic III and the remaining 10 were therapeutic IV (OCEBM 2011 levels of evidence chart).16 One of the deficits of existing literature is the variability and heterogeneity of outcome measures for assessment of Dupuytren’s disease. Such limitations include effectiveness, recurrence and adverse effects.
Effectiveness
Effectiveness infers that a treatment or intervention (already proven to be efficacious) offers a similar therapeutic benefit when delivered in a real-world setting, by standard clinicians and with a broad population base.17
The effectiveness of CCH for the treatment of Dupuytren’s disease has consistently been measured via improvement in total passive extension deficit (TPED) or Tubiana grading. The landmark phase III randomised controlled trial published in 2009 (by Hurst and colleagues) stated outcomes for measures of clinical effectiveness, which have been replicated in the literature and have formed a baseline for the comparative data of this review.2 Dupuytren’s disease results in significant functional impairment and, although subjective, patient-reported outcome measures (PROMs) ultimately provide insight into patient experience and perceived views of effectiveness.11
Clinical success
Clinical success of CCH for the treatment of Dupuytren’s disease is defined as a reduction in primary joint contracture to 0–5 degrees of full extension 30 days after the last CCH injection. Clinical success is reported as the percentage of study participants who achieved the 0–5 degree endpoint.2 Of the 13 studies included for measuring effectiveness, 11 measured clinical success.2,10,18–26 The lowest rate of clinical success (all joint average) was 41 percent by Skov and colleagues, who had a small sample size of 28 for the randomised controlled trial performed.22 The highest rate of clinical success was 72.5 percent by Alberton, who undertook a case series of 40 participants.21 Hurst and colleagues, who first documented clinical success in the landmark study, collagenase option for the reduction of Dupuytren’s disease (CORD I), achieved a clinical success of 64 percent for CCH compared with 6.8 percent for the placebo.2
In all studies, a greater proportion of participants achieved clinical success for the metacarpophalangeal (MCP) joint compared with the proximal interphalangeal (PIP) joint (Figure 2).2,10,18,22,24–26 This is consistent with the surgical literature for treatment of Dupuytren’s disease, whereby earlier intervention is the most effective.27
The collagenase option for reduction of Dupuytren long-term evaluation of safety study (CORDLESS), by Peimer and colleagues,28 examined the long-term effectiveness of CCH by collecting five-year data as a continuation of CORD I and CORD II. The study authors found that 53 percent of joints which achieved clinical success in CORD I and CORD II maintained that response over the following five years. In addition, treated joints did not return to their pre-existing contracture severity.29
Clinical improvement
Clinical improvement was defined by Hurst and colleagues as more than 50 percent reduction from baseline contracture 30 days after the last injection.2 Five studies measured clinical improvement as shown in Figure 3.2,10,18,26,30 The lowest level of improvement was documented by Witthaut and colleagues where 76 percent of 587 participants achieved the outcome.26 The highest level of clinical improvement was 90.1 percent of 110 study participants of Verstreken’s observational study.18 All studies recorded greater or equal clinical improvement for the MCP joint compared with the PIP joint.2,20,24,26,30
Patient-reported outcome measures
Validated patient-reported outcome measures (PROMs) include the unité rhumatologique des affections de la main (URAM) scale and the Southampton Dupuytren’s scoring scheme (Southampton).31,32 Other PROMs questionnaires used in the literature include disabilities of the arm, shoulder and hand (DASH), QuickDASH and the Michigan hand questionnaire (MHQ).33,34
Only three studies recorded PROMs, but none used the same measures and two did not include post-treatment scores. Of these, Verstreken used URAM, Zhou used MHQ and Skov used DASH.18,20,22 The lower the URAM score, the lower the degree of impairment or concern noted by the patient.31 The single study using both pre and post PROM showed patient perceived improvement post CCH injection.18
Patient satisfaction
Three studies assessed patient satisfaction at 30 days following CCH injection. Of these, patient satisfaction was recorded as 92 percent, 92.3 percent and 93 percent respectively.18,24,26 Clinical success was documented in two of these studies as 64.9 percent (92 percent patient satisfaction) and 57 percent (93 percent patient satisfaction).18,26 This suggests that patient opinions of treatment effectiveness vary from the objective outcomes measured.
Safety
Adverse events can have serious consequences on morbidity.18,35 The safety of collagenase is commonly reported within the literature by using the outcomes: treatment-related adverse effects and serious adverse effects.36 This is important, as many patients with Dupuytren’s disease are elderly with comorbidities and existing limitations upon their daily activities.
Treatment-related adverse effects
Of the nine studies analysing safety, three reported at least one treatment-related adverse effect in all participants receiving CCH.10,37,38 The lowest level of adverse effects was documented by Alberton, recording 57.5 percent of participants.21 Eight of the nine studies reported more than 75 percent of participants developing at least one treatment-related adverse effect (Figure 4).2,10,18,24,26,29,37,38 The two clinical trials that used a placebo (Hurst and Gilpin) reported treatment-related adverse effects in 96.6 percent and 100 percent of interventional participants respectively, compared with 21.1 percent and 38.1 percent for the placebo cohort.2,10
Common treatment-related adverse effects were recorded but they were variable across the studies. Common adverse effects were only included if 50 percent or more of the studies reported the variable as a common outcome. The most common adverse effect was peripheral oedema with seven studies assessing the variable. This occurred in over 60 percent of patients across each cohort.2,10,24,26,29,37,38
All common treatment-related adverse effects were local and included contusion, injection site haemorrhage, swelling and pain, ecchymosis, pruritus, skin laceration and lymphadenopathy. Adverse effects were reported as mild or moderate, however, only three studies assessed outcomes of mild and moderate separately.18,24,37 No studies provided classification or definition for mild and moderate adverse effects.
Serious adverse effects
Three studies reported nil serious adverse effects.18,21,29 The highest proportion of patients developing a serious adverse effect was five percent (3/60, pulley rupture, tendon rupture and pain management issue) recorded by Coleman and colleagues.37 The four serious adverse effects deemed to be treatment-related were allergic reaction to CCH, tendon rupture, ligament rupture and complex regional pain syndrome.2,21,24
Recurrence
Like all current therapeutic options, CCH does not provide curative treatment for Dupuytren’s disease.39 Recurrence data provide insight into the long-term effectiveness of CCH but also enable understanding of the need for repeat injections.28
The definition of recurrence of Dupuytren’s disease is discrepant among the literature, emphasised through the variations among different therapeutic options (surgery, radiotherapy).40 However, attempts have been made by Peimer and colleagues to accurately define recurrence.28,41 Recurrence is defined for CCH treatment of Dupuytren’s disease as ‘an increase of 20 degrees or more (relative to day 30 after the last injection) with a palpable cord or any medical/surgical intervention to correct new or worsening contracture in that joint’.28,42
Studies examining recurrence were follow-up studies of published data evaluating the effectiveness and safety of CCH. Two studies included the same cohort, published as three-year data and five-year data in separate papers.28,42 Only Peimer and colleagues28,42 reported the overall recurrence rate of all joints. At three years, 35 percent of successfully treated joints had recurred, and at five years 47 percent of all joints had recurred. This emphasised that 75 percent of all recurrences developed within the first three years post CCH injection.28,42 The rate of recurrence was higher among all PIP joints compared with MCP joints (Figure 5).
Discussion
This review focuses upon the effectiveness and safety of CCH and the recurrence of Dupuytren’s disease following CCH treatment. The use of CCH is increasing in Australia, with 25 publicly-funded clinics currently practising CCH treatment. With the translation into real-world settings, we must ensure that CCH is optimally and safely delivered.
Effectiveness
Many studies have reported on the efficacy and effectiveness of CCH, yet the lack of consistent terminology has limited the assessment across all studies. The effectiveness of CCH for treating Dupuytren’s disease using the two terms ‘clinical success’ and ‘clinical improvement’ was variable across the literature, ranging from 41 percent to 72.5 percent of study cohorts. MCP joints consistently showed greater clinical success and clinical improvement compared with PIP joints.
Collagenase clostridium histolyticum injection protocol was different across the studies. Hurst and colleagues first described the commonly used injection method of using 0.58 mg of CCH per injection, reconstituted in a sterile diluent of either 0.39 mL (MCP joint) or 0.31 mL (PIP joint). The CCH was to be injected once directly into the affected cord.2 All studies documented using 0.58 mg per injection but two studies did not record their diluent volume.18,24 Furthermore, three studies injected over three locations in the fibrous cord.19,21,30
The measurement protocol for assessing contracture degree was scarce within the literature. Only five studies recorded their goniometer and goniometer user method. Again, Hurst and colleagues described the commonly used measurement protocol for measuring fixed-flexion angles by passively extending the finger until a firm end-point is achieved.2 Only two other studies reported their goniometry methods aligning with Hurst.10,28 The remaining studies did not document their goniometer protocol sufficiently.18–26,30 Furthermore, only one study reported using the same clinician for baseline and post-treatment measurements.19 Consequently, the remaining studies may have been exposed to inter- and intra-reporter variability, leading to discrepancies within their results.43 The variation among measuring contracture degree may have affected the assessment of CCH effectiveness and limited the standardised interpretation across the literature.
The manipulation method varied between studies. Hurst and colleagues and others described performing manipulation 24 hours after injection without local anaesthesia and allowing three extension attempts at manipulation.2,10,26,28 Six studies reported using local anaesthesia,19–22,25,30 which may have enabled physicians to more forcefully manipulate the affected digit and consequently improve effectiveness results.44 All studies performed manipulation after 24 hours but two studies undertook manipulation between 24 and 72 hours dependent upon patient and physician availability.20,24 One study compared day one with day seven manipulation, but found no statistically significant effectiveness results.30 This study highlighted how further research is required into CCH methods to ensure that effectiveness can be maintained while providing flexibility in clinical practice.44,45
Several studies employed hand therapy as a potential means of sustaining effectiveness. This was not undertaken, or recommended, by Hurst and colleagues.2 Four studies stated that participants were provided with hand exercises to perform at home.20,22,23,30 Ten studies provided nightly splints for patients.2,10,18,20–23,25,26,30 However, the time frame of splint use varied between the studies.2,10,18,20–23,25,26,30 The current evidence suggests that splints offer no therapeutic benefit following surgery, yet extended use in the literature emphasises the need for further assessment.46,47
PROMs were not well recorded across the literature. This can be attributed to two factors: the lack of validity and consistency of using PROMs and the length of time these questionnaires take to complete.48 The URAM score was validated in 2011 and is quicker to complete than both the MHQ and the DASH but its relevance to English-speaking populations has been questioned due to translation concerns.49 The MHQ is reliable yet lengthier to complete (average 10 minutes) and far more complicated to calculate, which limits its use.34 The DASH and the QuickDASH have been found to have inadequate validity for Dupuytren’s disease and have a lengthy completion time. Finally, the Southampton has been declared more reliable, consistent and specific compared with the QuickDASH but due to its recent introduction there are limited data available.33
There has been inconsistent use and reporting of PROMs. Furthermore, when patient satisfaction has been measured against clinical success, results were higher for patient satisfaction.18,26
Overall, variability in how effectiveness is measured and reported across the literature highlights that minimal consensus currently exists, supporting the recommendation that consistent outcome measuring and reporting should be developed for Dupuytren’s disease.
Safety
The safety of CCH was well reported. Most studies recorded their cohort reporting at least one treatment-related adverse effect. However, terminology for types of adverse effects was inconsistent. Three studies reported that investigators ‘used their own terminology to describe adverse effects’,2,10,29 five studies did not report how they determined the classification of adverse effects18,21,26,37,38 and one study stated that adverse effects were classified according to the Medical Dictionary of Regulatory Events.24 This lack of consensus towards classification may skew data towards commonly known adverse effects.
The most comprehensive data comes from the CORD studies which, because of their nature as sponsored phase three trials, have included all events (bruising, swelling and pain) as adverse events rather than clinical expectations.
Recurrence
Recurrence was poorly reported in the literature. The lengthy follow-up required to observe recurrence appeared to hinder investigation. Our review of recurrence only discussed joints successfully treated, due to the limited literature describing joints that either failed CCH treatment or were partially responsive. Only Peimer and colleagues acknowledged this.28 Long-term follow-up of partially and non-successfully treated joints needs further research to accurately assess recurrence.
Follow-up
The follow-up period ranged from 30 days to eighty years and may have affected all outcomes of effectiveness, safety and recurrence. Recurrence follow-up varied between three and eight years however, as stated by Peimer and colleagues, 75 percent of recurrences that were recorded at five years had already developed at three years.28 This suggests that most recurrences develop early, following clinical success.
Bias
Of the four randomised controlled trials reviewing effectiveness, two used intention-to-treat analysis2,10 and the other two failed to account for loss to follow-ups and thus it was assumed a per-protocol analysis was used, potentially resulting in attrition bias.22,30 Two employed a double blinding method, whereas the other randomised controlled trials were open label.2,10 All randomised controlled trials employed a random sequence generator and random allocation process to minimise selection bias.2,10,22,30
Of the observational and comparative studies, loss to follow-up was not addressed in the studies where participant drop-out occurred.18,19,21,23–25,28,29,37,38,41,42,50 Among these observational studies, patients knew that they had received CCH and were being studied for adverse effects. This may have led to the Hawthorne effect (the alteration of study participants behaviour when they know they are been studied). No studies acknowledged this when reporting adverse effects.
Furthermore, as all three studies assessing recurrence followed up previous randomised controlled trials, one-third of patients failed to enrol from the original randomised controlled trial with Peimer and colleagues and Watt and colleagues recording two-thirds of eligible patients failing to enrol.28,41,42 The lack of follow-up may have resulted in selection bias, due to the select proportion of joints included in the follow-up.
It should be highlighted that 13 of the 18 studies included in this review received some form of funding or research support from Auxilium Inc., the US manufacturer of CCH.2,10,18,20,22,25,26,28,29,37,38,41,42 This funding effect may show a tendency for researchers to support the Auxilium Inc. product (CCH) and potentially lead to publication bias.51
Future implications
Ultimately, treatment of Dupuytren’s disease is becoming multimodal and heterogeneous, individual to each patient’s needs and wants. Of the limited data that currently exist comparing CCH with surgical treatment, Zhou and colleagues found that clinical improvement of MCP joints was 87 percent for limited fasciectomy, compared with 77 percent for CCH patients with a non-significant p value of 0.3239. For PIP joints, 72 percent of fasciectomy patients experienced clinical improvement, compared with 43 percent of CCH patients. It should be noted that the CCH cohort had worse initial MCP contractures, milder PIP contractures and the distribution of involved fingers was different across cohorts.20 Furthermore, Scherman and colleagues compared CCH with needle fasciotomy for Dupuytren’s disease with nil statistical differences found between the cohorts at three and 12 months for total passive extension deficit, pain, function and recovery.52 These two small studies highlight the similar effectiveness currently documented for CCH and surgical techniques.53 To standardise the assessment of recurrence across therapeutics, an increase in > 30 degrees in contracture or medical and or surgical intervention was used, whereby Van Rijssen and colleagues concluded a 24 percent recurrence rate at 3.7 years for limited fasciectomy and an 85 percent recurrence rate for needle aponeurotomy at 2.3 years.54 This is compared to a post-hoc 32 percent recurrence rate for CCH at five years.28 This highlights the increasing need to develop an appropriate paradigm for management of Dupuytren’s disease.
Conclusion
Collagenase clostridium histolyticum for the treatment of Dupuytren’s disease is a non-surgical therapeutic option that has the potential to satisfy Tubiana’s treatment goals to correct contracture, avoid complications and shorten recovery time.4
Further investigation is required to accurately assess CCH’s effectiveness, particularly adverse effects and recurrence rates. However, its potential as a non-surgical therapeutic option improves the treatment of Dupuytren’s disease: the potential to minimise treatment time and cost could substantially improve the public healthcare sector, and the recovery and safety profile could encourage people with Dupuytren’s disease to access treatment earlier.
Disclosures
Associate Professor David J Hunter-Smith is a consultant for Actelion (distributor of Xiaflex® in Australia). The authors have no other conflicts of interest to declare.
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
_joint_vs_proximal_interphalangeal_(pip)_joint_com.jpeg)
_joint_vs_proximal_interphalangeal_(pip)_joint.jpeg)

_joint_vs_proximal_interphalangeal_(pip)_joint_co.png)

_joint_vs_proximal_interphalangeal_(pip)_joint_com.jpeg)
_joint_vs_proximal_interphalangeal_(pip)_joint.jpeg)

_joint_vs_proximal_interphalangeal_(pip)_joint_co.png)