Introduction
Hand neurilemmomas have a variety of documented unusual anatomical locations, including intraosseous, subungal and within the carpal tunnel.1–3 This case report describes an occurrence of a neurilemmoma in the hand which is unusual not only in its anatomical location but in the way it mimics a more malignant process.
Case presentation
A 53-year-old, left-handed, male manual worker was referred to his local plastic surgery unit with an 18-month history of a painless but enlarging lesion on the radial side of his left ring finger. The lesion was precipitated by a crush injury at work a year earlier that was conservatively managed. The patient reported the lesion rapidly doubling in size and becoming ulcerated within the preceding month. The patient was a non-smoker with hypercholesterolaemia.
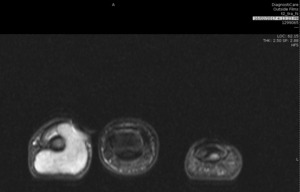
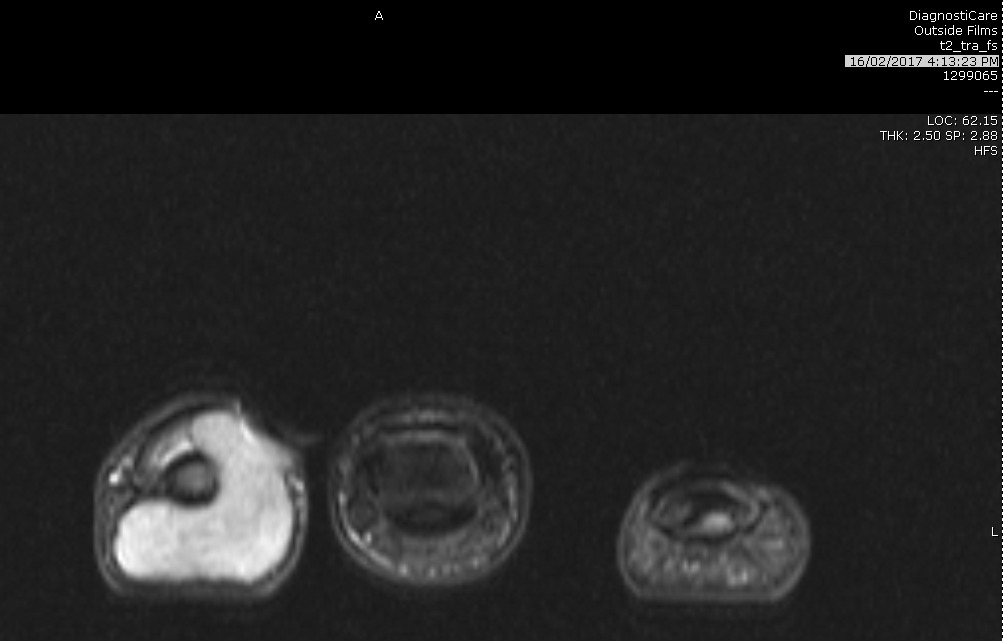
Examination revealed a 20-millimetre, non-tender, ulcerated paronychial mass lifting the nail plate (Figure 1). Distal tip sensation was intact. X-ray showed cortical thinning of distal phalanx consistent with extrinsic compression. MRI noted two separate but communicating lesions, which almost circumferentially enclosed the distal phalanx (Figure 2).
Differential diagnoses included glomus tumour, pyogenic granuloma, periungal fibroma and neurofibrosarcoma. A shave biopsy revealed an ulcerated, haemorrhagic neurilemmoma with S100 positive spindle cells supporting a Schwann cell origin. The lesion continued to rapidly increase in size after biopsy.
Final histology confirmed a >25 mm3 ulcerated neurilemmoma, with clear margins, sparse mitotic figures and S100 positive spindle cells which tested negative when stained with EMA, CD34 and HHV8. No melanocytic features were noted.
Ulnar and radial digital nerves were identified in the digital stump and sent separately for histology to exclude proximal perineural invasion. These samples proved unremarkable. The amputated finger healed well with no pain at three-month follow-up (Figure 3).
Discussion
This tumour was unusual in three respects—neurilemmomas are usually slow growing, volar and rarely occur distal to the proximal interphalangeal joint.4,5 This tumour was both dorsal and fast growing, doubling in size in a month.
There are two reports in the literature of neurilemmomas occurring distal to the proximal interphalangeal joint—one a subungal neurillemoma and another at the eponychial fold.6 Both case reports describe well encapsulated, small neurilemmomas (<10 mm3) that were excised from the surrounding structures. There have been no reported instances of a near circumferential neurilemmoma arising from the paronychial fold. This tumour was not only large and further rapidly enlarging, it had an ulcerated appearance with areas of necrosis.
The goal of surgical resection is to preserve function and continuity of the nerve.7 Two methods are reported in the literature: intraneural enucleation is the process of peeling the tumour off the nerve trunk and is suited to small tumours8; intracapsular enucleation involves incising the capsule and removing the mass, which is safer and suited to larger tumours.9
Despite a reassuring biopsy result, the clinical features of the lesion raised concerns about malignant transformation. Furthermore, its near circumferential pattern of growth meant intraneural or intracapsular enucleation would likely devitalise surrounding soft tissues. After discussion with the patient, the digit was amputated to the level of the middle phalanx.
Conclusion
The benign pathology warranted consideration of excision and length preservation of the digit. However, due to its near circumferential extension around the distal phalanx, the digit required amputation to the level of the middle phalanx.
Consent to publish
Patients signed informed consent regarding publishing their data and photographs.
Disclosure
The authors have no conflicts of interest to disclose.
Funding
The authors received no financial support for the research, authorship, and/or publication of this case report.
Revised: February 15, 2018 AEST; February 28, 2018 AEST; April 2, 2018 AEST