Introduction
Component reduction of the upper lateral cartilages (ULCs) and the bony dorsal hump can damage the attachment between nasal bones and the ULCs,1 resulting in an inverted-V deformity. After nasal bone reduction, in-fractures and osteotomies are commonly performed to close the resulting open book deformity, narrow a wide nasal base or correct deviated nasal bones.2 Incorrectly placed osteotomies and soft tissue manipulation may result in an irregular dorsal contour, airway problems or middle vault collapse.3 Maintaining the position of the nasal bones and their relationship with the ULCs in the immediate postoperative period is a key determinant in the patient’s final aesthetic result. This has traditionally been achieved through a variety of different techniques using plates, wires, halos or external splinting. Our technique gives the surgeon increased intraoperative and postoperative control of the position of the nasal bones.
Operative technique
Through a transcolumellar incision, we sharply dissect the skin and subcutaneous tissue from the cartilaginous and nasal framework. The ULCs and lower lateral cartilages (LLCs) are skeletonised. The ULCs are separated from the dorsal septum preserving the nasal mucosa. The cartilaginous hump is reduced using an 11 blade to the level of the keystone area and just under the inferior portion of the nasal bones. The bony hump is reduced to a desirable profile using a rotating burr. Median osteotomies are performed with the rotating burr.
Prior to the percutaneous nasal bone osteotomies, the percutaneous sutures are placed. A straight Keith needle (Surgiform) is inserted into a Kirschner-wire (K-wire) driver. The needle is passed percutaneously through the nasal bones and septum, in one pass, to the opposite nasal sidewall. The suture captures both the ULCs and the nasal bones. The suture thread of 3/0 polydioxanone suture (PDS II) (Johnson & Johnson MedTech) is inserted into the loop of the Keith needle.
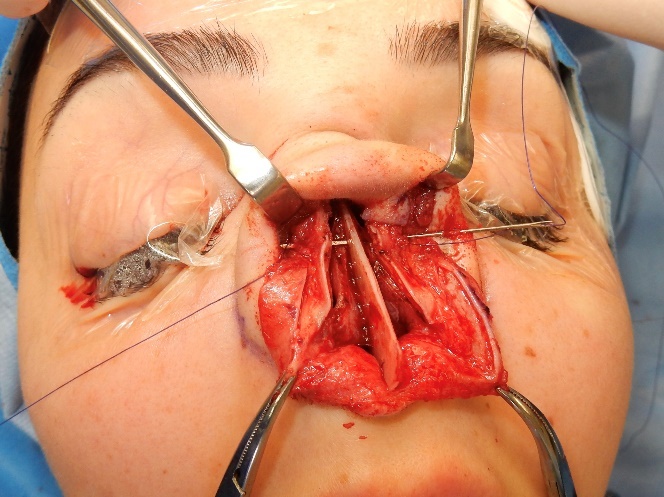
The Keith needle is then manually withdrawn from the nasal vault, to the opposite side, in the direction it was placed using a needle holder (Figure 1).
While the assistant retracts the degloved nasal skin vertically, the surgeon locates both ends of the PDS suture where it enters the deep surface of the skin and soft tissue. The surgeon brings both ends of the suture thread caudally and medially into the surgical wound, internalising the suture thread completely. The process is repeated with a second Keith needle, parallel and caudal to the first suture. This caudal pass is performed with the soft tissue retracted cranially (Figure 2). The suture is tied after the nasal osteotomies and manipulation of the nasal bones.
The rhinoplasty continues with lateral percutaneous osteotomies and medial osteotomies that are performed in a standard fashion, using a 2 mm osteotome in a low-to-low direction to fracture the nasal bones from the pyriform aperture to the nasal process of the frontal bone.4 The in-fractures are performed with digital pressure. With the soft tissue envelope redraped over the skeleton, the symmetry of the nasal bones and the side profile of the nasal dorsum are assessed prior to tying the PDS suture. Avoid overtightening the sutures, as this can lead to pinching of the osseocartilaginous structure.
To finish, we refine the tip and augment the nasal dorsum with ultra-diced cartilage graft from the resected ULC dorsal hump.5
Discussion
After a literature review, we found two published papers with some common principles to our described technique. Kayabasoglu and colleagues describe reconstruction of the nasal dorsum using costal cartilage grafts fixed in position using a K-wire as a guide inside a percutaneous 18G needle through which Prolene sutures (Johnson & Johnson MedTech) are used to achieve nasal dorsum reconstruction.6 Bali and colleagues describe the use of a hammer and needle to create four holes in the nasal bones and septum.7 Our technique has a number of advantages over these techniques. By placing the Keith suture directly in the K-wire driver we improve surgical economy and efficiency. Our technique increases support of the ULCs by suturing them to the septum and bolsters the attachment between the ULC and nasal bones at the keystone area, as the ULCs extend cranially under the nasal bones up to 14 mm cranially.8 This closes the open book deformity, while restoring the anatomical attachment without the need for spreader grafts to prevent middle vault collapse.9
The percutaneous suture through the septum and nasal bones should be done before the percutaneous osteotomies as it is much harder to pass the Keith needle after the nasal bones have been fractured. Further dorsal hump reduction is possible after the PDS sutures have been tied, although this is limited by the depth the sutures were placed at. Our percutaneous technique allows us to place the sutures cranially without being limited by the soft tissue laxity of the overlying skin flap. A PDS suture has a measurable tensile strength of up to 80 days in vivo, which re-enforces the relationship between the ULCs and nasal bones, reducing postoperative complications and maintaining the desired position of the nasal bones.
Conclusion
This technique allows the surgeon to close an open book deformity while controlling both the nasal bones and their ULC attachment. As a result this allows the surgeon to reliably reduce a nasal hump deformity and consolidate long-term aesthetic outcomes for rhinoplasty patients.
Patient consent
Patients/guardians have given informed consent to the publication of images and/or data.
Conflict of interest
The authors have no conflicts of interest to disclose.
Funding declaration
The authors received no financial support for the research, authorship and/or publication of this article.