Introduction
Calvarial exposure is a recognised complication following both surgery and radiotherapy to treat scalp skin cancers and it can lead to life-threatening complications.1 Exposure of the bone leads to necrosis, infection, osteomyelitis and sequestrum that can cause significant morbidity or mortality.2,3 These frequently develop into chronic wounds that can reduce quality of life, and are resource-consuming and expensive to treat.4 Reconstructive techniques in this context may be challenging owing to the effects of radiation, including microvascular occlusion and fibrosis on local tissue.1 Despite the significance of this issue, there is minimal discussion of the incidence and management of calvarial exposure in the literature.
Surgical excision is the most common treatment modality for scalp skin cancers and it is considered the treatment of choice for most tumours.5 Radiotherapy is often indicated for patients where the functional and/or cosmetic results would be better than surgery, for example, surgery may be unsafe because of the location and size of the tumour, or because the patient has comorbidities or is elderly.6,7 Scalps may undergo both surgery and radiotherapy over a patient’s lifetime as part of dual therapy for a single lesion or in the treatment of field recurrence, new lesions or reconstruction of radiation-induced changes.8 While calvarial exposure is a known risk for either modality,9,10 there currently exists no comparative study exploring the difference in incidence of calvarial exposure for patients receiving surgery alone compared to radiotherapy alone or dual therapy. Therefore, the purpose of this study is to investigate the phenomenon of exposed calvarium in patients undergoing treatment of scalp malignancies and address a clear gap in the scientific literature.
Aim
Primary aim: To report the incidence of calvarial exposure in the treatment of T2 and T3 scalp malignancies.
Secondary aim: To investigate risk factors for calvarial exposure in patients undergoing surgery and/or radiotherapy for the treatment of T2 and T3 scalp skin cancers.
Methods
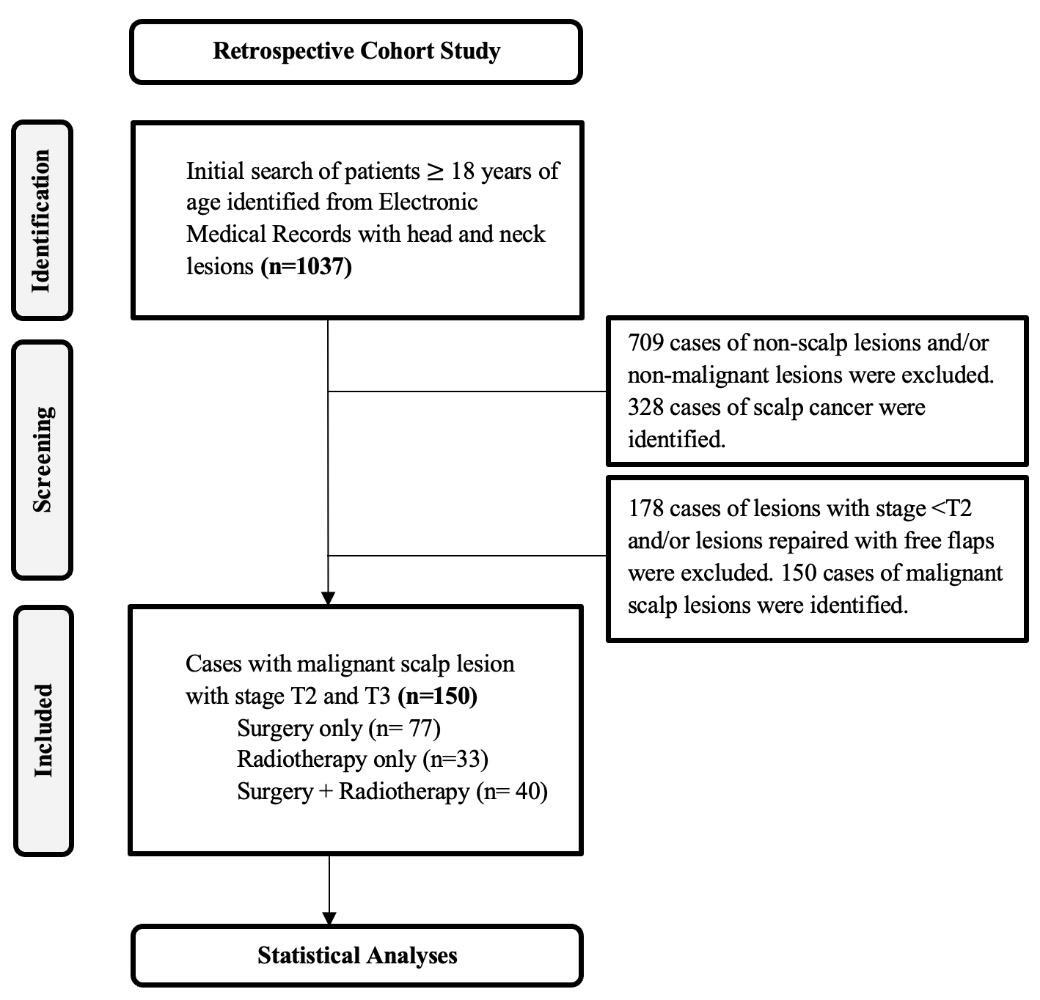
This was a retrospective review of patients presenting to Liverpool Cancer Therapy Centre with T2 or T3 scalp malignancy between 2016 and 2022 (Figure 1). Patients were identified from electronic medical records. Electronic medical records were also used to evaluate the operation reports, radiotherapy reports and histopathology of all patients. Patients aged over 18 at presentation with at least one tumour staged T2 or T3 on the hair-bearing parts of their head were included in this study. Simultaneous skin cancers on one patient were counted as separate cases if they were excised from different pieces of skin or irradiated separately, otherwise they were counted as a single case. Recurrence of skin cancer was included as the same case as the initially presenting lesion. A total of 150 lesions and 145 patients were identified from the database. Patients undergoing free flap reconstructions were excluded.
General information was collected for each patient through the hospital’s medical record systems and included patient demographics (age, gender), skin lesions (number, pre-treatment stage, tumour grade), concurrent medical conditions, smoking status, treatment type (surgery, radiotherapy or both), calvarial exposure, wound infection, central nervous system infection, and death (duration from last treatment, cause of death).
Specific information collected for each of the treatment groups and the patients with calvarial exposure included radiotherapy (site, duration, dosage), surgery (area of excision, type of reconstruction, date of surgery), dual therapy (days between surgery and radiotherapy) and calvarial exposure (size of calvarial exposure, time from last intervention to diagnosis, treatment for exposure, follow up duration, presence of healing, time to healing).
Tumour size was based on the documented size of the lesion in histopathology reports and radiotherapy planning documentation. The excision area was determined using operative and histological reports. The Charlson Comorbidity Index (CCI), which predicts 10-year survival in patients with multiple comorbidities,11 was calculated for each patient using their concurrent medical conditions and age as an indicator of comorbidity. The assigned weights for each condition can be seen in Table 1. The shape and area of calvarial exposure was often not recorded in patient medical records; as such, calvarial exposure size was determined by the average of the documented dimensions.
Data was analysed with descriptive statistics. Categorical variables were summarised with frequencies and percentages. Continuous data were summarised using means and standard deviations. Data was stratified by treatment modality.
Ethics approval was given by the South Western Sydney Local Health District Ethics Committee (approval number 2021/ETH00298).
Results
A total of 150 lesions were identified in 145 patients. Of the lesions identified, there were 111 (74.0%) squamous cell carcinomas, 20 (13.3%) basal cell carcinomas, 5 (3.33%) melanomas, 7 (4.67%) pleomorphic dermal sarcomas, 1 (0.67%) angiosarcoma, 1 (0.67%) myxofibrosarcoma, 1 (0.67%) fibrous histiocytoma, 1 (0.67%) sarcoma and 1 (0.67%) atypical fibroxanthoma. Two (1.33%) lesions did not have histopathology available. The average age of patients was 77.5 years old; 126 (86.9%) were males and 19 (13.1%) were females. 93.33% of the patients were current non-smokers. To treat the 150 lesions, 33 (22.0%) underwent radiotherapy only, 77 (51.3%) underwent surgery only, the remaining 40 (22.7%) underwent dual therapy. Overall, 8 (5.3%) patients experienced calvarial exposure. The number and percentage of each treatment group that experienced calvarial exposure is provided in Table 2.
Of the 40 patients in the dual therapy group, 32 patients (80.0%) received surgery followed by radiotherapy and 8 patients (20.0%) received radiotherapy followed by surgery (Table 3). The number and percentage of each dual therapy group that experienced calvarial exposure is provided in Table 3.
The mean size of calvarial exposure was 2.6 cm (range 1–5 cm). Mean CCI score was higher in patients who underwent radiotherapy than surgery (RTx 6.94 ± 1.87; Sx 5.96 ± 2.22; p < 0.05). There was also a trend for a higher CCI score in patients who experienced calvarial exposure (7.25 ± 1.83) than the non-exposure population (6.29 ± 1.99) (p = 0.18). In the surgical cohort, the average area of excision was higher in patients who experienced calvarial exposure (502.31 cm2 ± 518.46) than those who did not (263.36 cm2 ± 392.47) (p = 0.13). The smallest area of excision resulting in calvarial exposure was 7.65 cm2.
Initial reconstruction during scalp cancer surgery for the six surgery patients who experienced calvarial exposure included one full thickness skin graft, one split thickness skin graft and four transposition flaps with split thickness skin graft to the secondary defect. All four patients with transposition flaps experienced breakdown at the site of their split thickness skin graft. Out of all patients who had a transposition flap with a split thickness skin graft, 13.8 per cent experienced calvarial exposure.
In the radiotherapy cohort, calvarial exposure patients received an average dose of radiotherapy 23.03 Gy higher than non-exposure patients (exposure 73.50 Gy; non-exposure 50.47 Gy; p = 0.0011).
Three of the calvarial exposure patients (37.5%) underwent surgical reconstruction of their exposure and all three achieved healing. The remaining five calvarial exposure patients were treated conservatively with dressings; at the time of analysis, none of these patients had achieved healing. At the time of analysis three of the non-healed exposure patients had died; however none of their deaths were attributed to exposed calvarium. The mean duration of follow-up in the non-healed exposure patients was 176.6 days (range 0–441 days). No patients experienced osteomyelitis, meningitis or bone erosion.
Discussion
Calvarial exposure following surgical or radiotherapeutic treatment of scalp malignancies is a known but under-described phenomenon.9,10 Quality of life post-cancer is becoming increasingly important as people live longer lives, thus a consideration of patient morbidity is more important than ever. Yet in head and neck cancers there exists a paucity of knowledge about skin and wound care. In the context of modern multidisciplinary care, a thorough understanding of the incidence and risk factors of calvarial exposure would help clinicians with pre-treatment counselling, consideration of appropriate treatment and effective resource allocation. The rate of calvarial exposure in this study was 5.3 per cent, with the exposure rate of the single modality treatment group at 4.6 per cent compared with the dual modality treatment group at 7.5 per cent. The rate of exposure in dual therapy patients was higher than single modality treatment irrespective of therapy sequence. This figure is an important reference point for clinicians when obtaining informed consent, planning treatments and improving quality of care. In this study, factors that significantly contributed to calvarial exposure included the size of the resection, reconstructive method, radiotherapy dose and comorbidities of the patient.
To date, there has been no comparative study exploring the difference in incidence of calvarial exposure for patients receiving surgery alone compared to radiotherapy alone or a combination of the two interventions. Thus, this is one of the largest reports of calvarial exposure in the current literature. Existing studies lacked comparative elements, focused on single treatment modalities and suffered from low sample size and selection bias or were single study case reports and case series.4 Bone and soft tissue radionecrosis is widely reported in the mandible,12,13 but less commonly in the calvarium. Factors leading to mandibular osteoradionecrosis (ORN) include dose, proximity of tumour to bone, trauma (eg, perioperative dental work) and poor oral hygiene.14 It is reasonable to infer the same factors would contribute to calvarial ORN. Intriguingly, the factors leading to ORN, such as trauma and poor oral hygiene, may be precipitated by surgical intervention and actinic skin respectively. Hence future prospective research should look to capture data regarding general skin quality, including actinic changes and alopecia.
In our cohort, we have calculated a 1 in 20 rate of long-term calvarial exposure following treatment for scalp skin cancer. In our study, calvarial exposure only occurred in areas of excision greater than 7.65 cm2. We selected T2 lesions (≥4 cm2–<16 cm2) and T3 lesions (>16 cm2) for inclusion in this study. The rationale for adopting this choice was grounded in the low occurrence of bone exposure in T2 and T3 lesions—selecting higher-risk groups enhances the likelihood of identifying distinctions between the two treatment methods. The finding that exposures occurred in excisions ≥7.65 cm2 vindicates our choice of T2 and T3 lesions. We excluded T4 lesions, as they have cortical or marrow involvement that would have provided a source of confounding. There was a trend towards calvarial exposure in patients with larger skin surface area resections but this did not reach statistical significance (p = 0.13). Possible suggestions for this association include first that these were higher-grade tumours requiring wider margins and excision of pericranium; and second that these areas were too large for simple local flaps and were therefore grafted.
In our study, skin-grafted reconstructions tended to be significantly less robust than local flaps at preventing exposure. This confirms notions held by prior studies that flaps provide a more predictably vascularised wound bed, whereas grafts are generally avoided in the repair of defects with exposed bone given the high likelihood of ischaemic failure.10,15,16 None of the calvarial exposures healed with conservative treatments, while all calvarial exposures that had surgical closure attempted achieved healing. This suggests that surgical intervention should be considered early in treating calvarial exposure following scalp skin cancer.
Moreover, the mean time to bone exposure was 46 days with the earliest time at six days and the latest time at 209 days. This suggests an ‘at-risk’ window of bone exposure being in the first seven months or 209 days post treatment, with a standard deviation of 70.02.
Radiotherapy dose was on average 23.03 Gy higher in calvarial exposure patients when compared to non-exposure patients (p < 0.05). The CCI score for the radiotherapeutic patient groups was higher than the surgery only group (p < 0.05). It is important to note that this could be attributed to the fact that patients with greater comorbidities tended to receive radiotherapy alone or as an adjunct to surgery rather than surgery alone.
This study is limited by the typical drawbacks of retrospective research as well as the low overall incidence of calvarial exposure. Prospectively collected data would allow: capture and analysis of variables such as skin quality and alopecia, patient reported outcome scores, patient characteristics and comorbidities; standardised follow up; and relevant documentation of specific treatment detail. It would also establish a clear temporal sequence between exposure and outcome, reduce recall and selection bias, and allow for more rigorous data collection control. Additionally, analysis of the radiotherapy area would have ideally been explored, which was not possible due to the varied therapy modalities used on different patients. As such, there exists room for future prospective studies to be conducted as well as studies conducted over longer time horizons with larger sample sizes. Notably, using 5 per cent as the risk of calvarial exposure approximated from our data, future studies would need to have a sample size of around 928 to give adequate power.
Conclusion
This retrospective study has demonstrated a trend towards a higher incidence of calvarial exposure in dual therapy patients than those who received surgery only or radiotherapy only. This study identifies larger skin surface area resections, larger radiotherapy doses and a higher CCI score as risk factors for the development of calvarial exposure. Incidence of calvarial exposure following treatment of scalp skin cancer is low but outcomes are poor. This study has additionally identified the need for a large-scale prospective study to be conducted and the necessary variables to include.
Patient consent
Patients/guardians have given informed consent to the publication of images and/or data.
Conflict of interest
The authors have no conflicts of interest to disclose.
Funding declaration
The authors received no financial support for the research, authorship, and/or publication of this article.
Revised: November 1, 2024 AEST; November 16, 2024 AEST