Introduction
With one in eight women in Australia projected to be diagnosed with breast cancer in their lifetime and a growing number of women opting for autologous reconstruction, management of the donor site has become crucial.1 Since the introduction of the deep inferior epigastric artery perforator (DIEP) flap, plastic and reconstructive surgeons have improved its reliability and reduced functional morbidity to the donor site.2 Despite being frequently explained to patients as having a similar impact on the abdominal wall as cosmetic abdominoplasty, less effort has been directed at improving the aesthetic impact of the DIEP donor site. We present our senior author’s unique modified corset rectus plication technique to optimise the aesthetic outcome of the DIEP donor site and review its application in 10 consecutive patients.
Operative technique
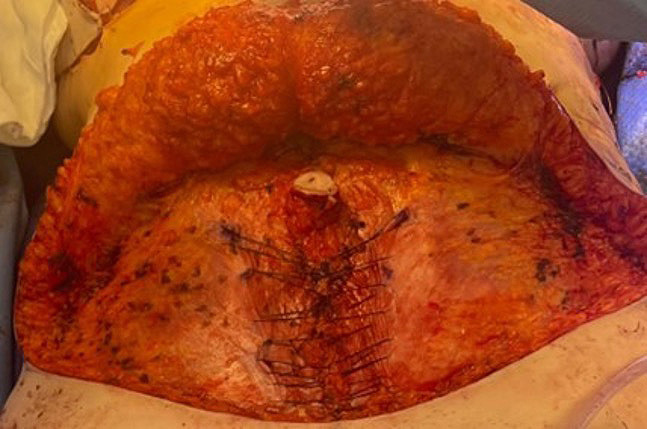
We retrospectively reviewed 10 consecutive patients undergoing this technique using bilateral DIEP flaps. All patients have given consent for clinical photography and publication. The DIEP flaps are raised and the abdominal wall is undermined to the xiphisternum in a standard manner. The rectus sheath is also closed in standard double-layer with interrupted 2.0 PDS suture (Ethicon, Raritan, New Jersey, USA) for the initial approximation, followed by a continuous 0 Stratafix suture (Ethicon, Raritan, New Jersey, USA). Rectus plication cranial to the umbilicus is performed in the same double-layer technique. Rectus plication caudal to the umbilicus is performed using the modified corset technique where 0 nylon suture is run continuously from mons to umbilicus and back to mons, grasping the external oblique aponeuroses bilaterally and preferentially grasping the aponeuroses wider at the level of umbilicus in order to advance the fascial edge and tighten the waist (Figure 1). Tension is initially applied by the operator and maintained by the assistant as the operator takes the next bite. Careful selection of a robust section of fascia and taking bites of adequate length ensured that we did not experience any suture pull-through. This nylon suture creates a construct similar to a nylon mesh and hence reduces the risk of abdominal bulge/hernia.
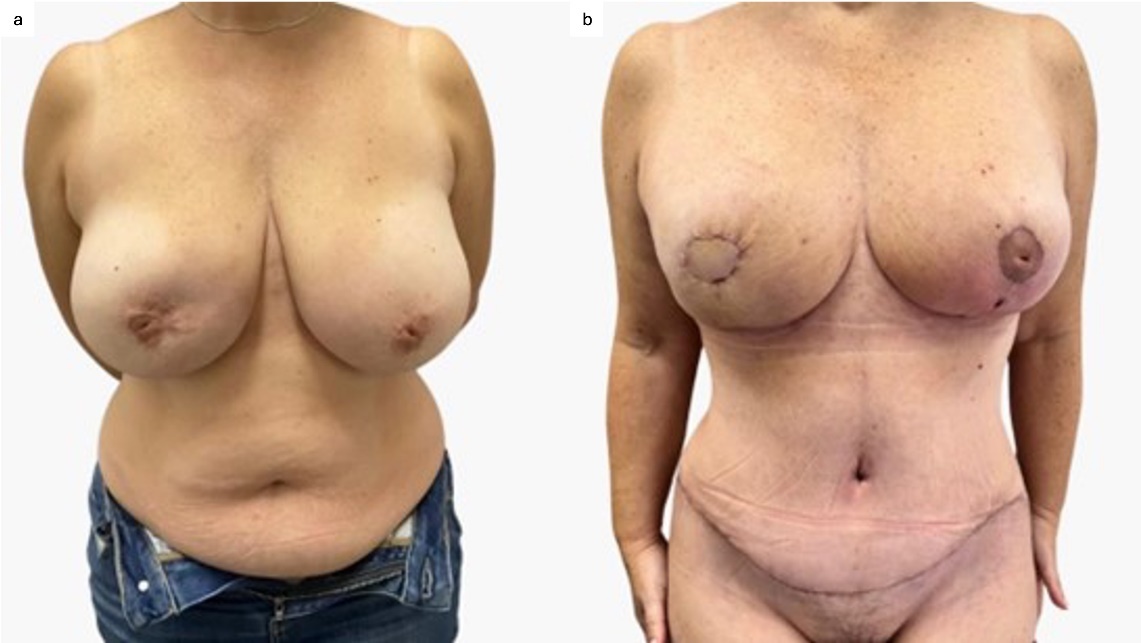
The average age of patients was 56 years old (range 42–69 years). All 10 patients had virgin abdominal wall history. All patients had similar courses of recovery in the immediate postoperative period. Notably, the introduction of the modified corset technique did not increase analgesia requirement or affect bowel function. At three-month follow-up, no patient reported abdominal hernia/bulge and all patients demonstrated a more aesthetically-pleasing, tapered waistline (Figure 2).
Discussion
Autologous breast reconstruction with DIEP flap has become the gold standard in patients with breast cancer.3 In comparison to transverse rectus abdominis myocutaneous (TRAM) flaps, DIEP flaps have lower abdominal donor site morbidity but a higher fat necrosis rate.4 With the introduction of preoperative computed tomography angiography and enhanced selection of appropriate dominant perforator(s), the reliability of DIEP flaps has significantly improved.5 At some high-volume units, operative steps are optimised with input from anaesthetic and nursing staff, and those units are able to perform a bilateral as well as a unilateral DIEP flap in a single day.6 As a result, we are able to routinely achieve aesthetic breast reconstruction from DIEP flaps. In contrast, aesthetic abdominal wall reconstruction is not often prioritised.
Abdominal wall contour and waist definition are key to an aesthetic abdomen. Successful abdominoplasty addresses the skin and soft tissue, as well as the myofascial apparatus.7 The latter, when appropriately tensioned, can significantly enhance the abdominal aesthetic. Numerous techniques have been described for improving myofascial apparatus in cosmetic abdominoplasty.8 Goncalves and colleagues described a corset abdominoplasty technique where they plicate the rectus fascia in the midline as well as along the linea semilunaris from xiphisternum to the pubic tubercle, preferentially more at the level of umbilicus.9 In our experience, simple rectus plication technique would suffice above the level of umbilicus. However, below the level of umbilicus, a superior technique was indicated due to fascial division and pre-morbidly weaker fascia.
The DIEP flap donor site poses unique challenges due to fascial breach and potential loss, muscle weakness from dissection, and an incision pattern that may have to be higher than in cosmetic operations due to patient-specific perforator location. Our running nylon suture creates a mesh-like structure for both functional and aesthetic effects. The modification in our technique is that it is only performed below the umbilicus, and sutures are tapered widely cranially and with grasping switch.
Conclusion
Robust fascial repair is crucial in order to prevent functional morbidity from DIEP flap reconstruction. We present a retrospective analysis of 10 consecutive bilateral DIEP flaps where we have performed a modified corset repair that both enhances the aesthetic outcome of the DIEP flap donor site and acts like a nylon mesh to improve the strength and integrity of the abdominal wall.
Patient consent
Patients/guardians have given informed consent to the publication of images and/or data.
Conflict of interest
The authors have no conflicts of interest to disclose.
Funding declaration
The authors received no financial support for the research, authorship, and/or publication of this article.
Revised: October 20, 2025 AEST