Introduction
Carpal tunnel syndrome (CTS) is a common median nerve compressive neuropathy. Any process that increases pressure within the carpal tunnel can compress the median nerve leading to sensory and motor dysfunction. Carpal tunnel syndrome is generally a chronic condition and can be associated with diabetes mellitus and rheumatoid arthritis. Acute CTS is a rare event occurring more commonly following trauma and often requires surgery to avoid serious sequelae.1 Amyloidosis is known to be associated with chronic CTS but rarely manifests in acute cases of CTS.2 This case report describes an unusual presentation of acute CTS secondary to amyloidosis requiring urgent surgical decompression.
Case report
A 91-year-old right-hand dominant woman presented with acute onset of idiopathic left-hand pain and paraesthesia to the fingertips. Physical examination revealed positive Tinel and Phalen signs. The patient also had decreased sensation over the volar aspect of the thumb, index, middle and radial half of the ring fingers in keeping with median nerve territory innervation.
A radiograph of the hand and wrist demonstrated multiple joint degenerative changes and no acute fracture or dislocation. A clinical diagnosis of acute CTS was made. The patient underwent urgent surgical decompression of the carpal tunnel through an extended volar approach under general anaesthesia. Once the transverse carpal tunnel ligament was released, florid synovitis, turbid fluid and hyperaemia were seen during exploration. The median nerve was flattened. Specimens were sent for histology and culture.
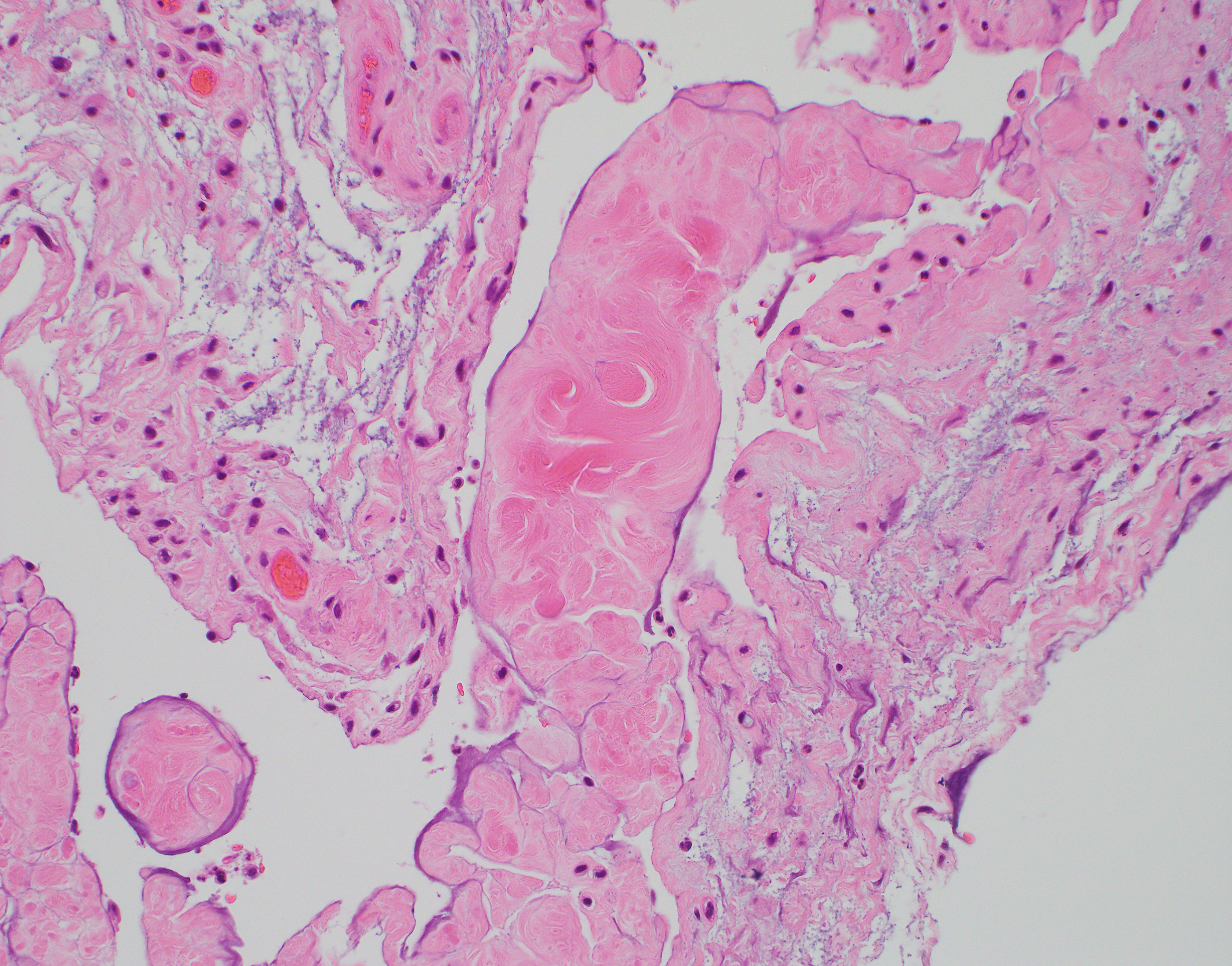
Intraoperative cultures were negative for growth of micro-organisms after five days of incubation and synovial fluid was negative for crystals. Tissue biopsy samples, including median nerve sheath and synovial tissue, sent during surgery, were analysed by immunohistology and Phenol Congo (Congo) red staining. Haematoxylin and eosin (H&E) staining showed a deposit of acellular, eosinophilic, extracellular material characteristic of amyloid (Figure 1). A positive Congo red stain showing red-orange to salmon-pink material highlighted the presence of amyloid as the foci of eosinophilic hyalinisation (Figure 2). When observed under polarised light, the positive Congo red stain demonstrated the ‘apple-green’ birefringence of amyloid (Figure 3).
Postoperatively all movements of the wrist were noted to be improved, with no pain or numbness in the fingers. The patient was followed up in clinic two and four weeks postoperatively and had no complications of note, with normal return of hand function.
Discussion
This case was unusual for two reasons. Firstly, non-traumatic presentations of acute CTS are uncommon. Secondly, the finding of amyloidosis in acute CTS is rare. Amyloidosis is more commonly reported with cases of chronic CTS. There is a paucity in the literature linking amyloidosis with cases of acute CTS—we were able to find only one case report in the English literature demonstrating a case of acute CTS secondary to amyloidosis.2
Chronic CTS is a common neuropathy encountered in clinical practice and symptoms progress over months to years, whereas the features of acute CTS progress over hours and days. Acute CTS is characterised by rapid progression of pain and paraesthesia in the distribution of the median nerve. It usually occurs secondary to a traumatic event such as fracture of the distal radius or carpal bones. Rarer non-traumatic cases may be secondary to infection, haemorrhagic disorders or inflammation.3 The rapid progression of acute CTS and the potential for lasting nerve damage make it a surgical emergency.
In this case, the diagnosis of acute CTS was based on clinical findings. Regardless of cause, no guidelines are available for diagnosing and managing acute CTS. Carpal tunnel release is considered the gold standard for treatment and time-sensitive surgery ensures better clinical outcomes.4 The goals of surgical decompression include resolution of symptoms and preservation of function by surgical release to prevent median nerve damage and maintain capillary blood flow.5 Full recovery of nerve function generally occurs between three to six weeks regardless of aetiology.6 This patient had full recovery from surgery with improved hand function and minimal neuropathy.
Amyloidosis has been linked with cases of CTS in the literature. Carpal tunnel syndrome is reported to be present in a quarter of patients diagnosed with primary systemic amyloidosis.7 Local amyloid deposits in the tenosynovium, transverse carpal tunnel and surrounding tissue reduce the low carpal tunnel volume, causing compression of the median nerve. In reported case series of carpal tunnel release with findings of amyloid deposits there were no cases of acute CTS.7,8 In this case the patient did not have a known diagnosis of amyloidosis or prior history of CTS symptoms in the affected hand. The significance of amyloid deposits in the absence of systemic amyloidosis is less clear. In one case series 82 per cent of patients who had amyloid deposits in the carpal tunnel had no evidence of systemic amyloidosis.9 During a 23.5 year follow up only two patients (2%) with localised amyloidosis went on to develop systemic disease.
There is one report in the literature of acute CTS secondary to localised amyloid deposits in the carpal tunnel.2 Unlike this case, that patient had a recent biopsy from an alternative site demonstrating findings consistent with secondary amyloidosis. The definitive method for diagnosis of amyloidosis is tissue biopsy. In one large series the sensitivity of carpal tunnel biopsies for clinically involved disease was reported as 90 per cent or more.9 Amyloid has a characteristic microscopic appearance where protein fibrils bind Congo red in an organised fashion, leading to apple-green birefringence under polarised light microscopy.10 The histological findings from this case are similar to those reported by Hakyemez and colleagues confirming the presence of amyloid deposits.2 In some cases, immunohistochemistry can be used to identify the protein subtype but this is variable and depends on the subtype.
Conclusion
Amyloidosis causing acute CTS is rare, with most patients likely to present with features consistent with chronic CTS. Urgent surgical decompression is the gold standard for management of acute CTS. As in this case, it should be noted that acute CTS may develop secondary to amyloid deposits in a patient with previously undiagnosed amyloidosis.
Patient consent
Patients/guardians have given informed consent to the publication of images and/or data.
Conflict of interest
The authors have no conflicts of interest to disclose.
Financial declaration
The authors received no financial support for the research, authorship, and/or publication of this article.