Introduction
Lithium ion batteries are highly powered and efficient sources of energy used to power many devices from mobile phones, power tools and vehicles.1 Lithium is the third lightest element with the lowest reduction potential of any element: this allows high gravimetric, volumetric capacity and power density providing a higher charger capacity per ion.2 Lithium batteries are composed of four main components: an anode, cathode, separator and electrolyte. The electrolyte in a lithium-ion battery is intrinsically flammable resulting in an exothermic chemical reaction.3 Commercially, there are variations in lithium ion batteries based on cell design, chemistry and size. Short circuiting is a common concern among many batteries that can lead to dramatic changes in the electrochemical structure of the battery resulting in local heat generation and transfer.4 This ‘thermal runaway’ phenomenon is an exothermic event that leads to elevated temperatures up to 80 °C which cracks the electrode material and surrounding structures impeding detection of temperature differences and leading to risk of fire and explosion.5,6 There are safety measures in place for some devices such as pressure burst discs, shutdown separators, and one-shot fuses.7
In recent years lithium batteries have gained attention for their potential in harvesting energy in grid systems but also for the risk of serious burn injuries in children and adults from portable electronic devices and e-cigarettes. The popularity of e-cigarettes has risen since 2007 with changes to tobacco regulation, attitudes and market factors across countries.8–10 There have been worldwide reports about the occurrences of explosions related to these devices leading to fires and explosions in phones, electronic scooters, vehicles and airplanes.11–14 Anecdotally, we noted a surprising number of burn cases in both children and adults related to lithium battery explosions that prompted an audit of these specific types.
The aim of this study was to describe the epidemiology, mechanism of injury and clinical outcomes of lithium battery related burns across three major tertiary centres in New South Wales (NSW), Australia. The secondary objective was to analyse and explore the preventative measures and policies.
Methods
The NSW Statewide Burn Injury Service (SBIS) has three major units that treat burns including two adult services—Concord Repatriation General Hospital (CRGH) and Royal North Shore Hospital (RNSH)—and one paediatric service, the Children’s Hospital at Westmead (CHW). Each year, over 2000 patients combined are treated in these units for burn related injuries. A 15-year retrospective review of the NSW SBIS database was conducted from January 2005–December 2019 including patients of all ages with burns caused related to lithium battery devices such as phone batteries, chargeable devices or e-cigarettes. This study was approved by the ethics committees of CHW, RNSH and CRGH [2020/PID00179].
Data were collected from the SBIS database including information on: sex, time and location of injury, total burn surface area (TBSA), operative intervention, length of stay and surgical complications. A statistical analysis using IBM SPSS Statistics version 26.0 (SSP Inc, 233 S Waker Drive, 11th floor, Chicago, Illinois 60606-6307, USA) was computed for continuous variables assessing the relationship between linear data and correlation based on a level of significance (p = 0.05). The continuous variables were expressed as mean, standard deviation (SD), percentages and range. The differences between proportions were analysed using Pearson’s chi-squared test for the device of injury and type of burn from categorical data.
Analysis
Patient profile
Twenty-four patients presented with burns related to lithium batteries with a 7:1 male predominance. Patients age was normally distributed ranging from 1 to 58 years with a mean age of 29.0 (± SD 16.6) years. The mean TBSA burnt was 2.5 per cent (± SD 0.9; range 0.1–21%). Nearly all patients sustained minor burns (less than 10.0% TBSA), however, TBSA was positively skewed with an outlier of 21.0 per cent sustained from a battery charging device explosion that caused a house fire. The majority of cases were flame burns (n = 15), followed by chemical burns (n = 4), contact burns (n = 3) and electrical burns (n = 2). There were six (25%) paediatric patients and the remaining 18 cases were adults. Three quarters of the cases (n = 18) occurred in the home setting. The majority of cases occurred after the year 2014.
Injury profile
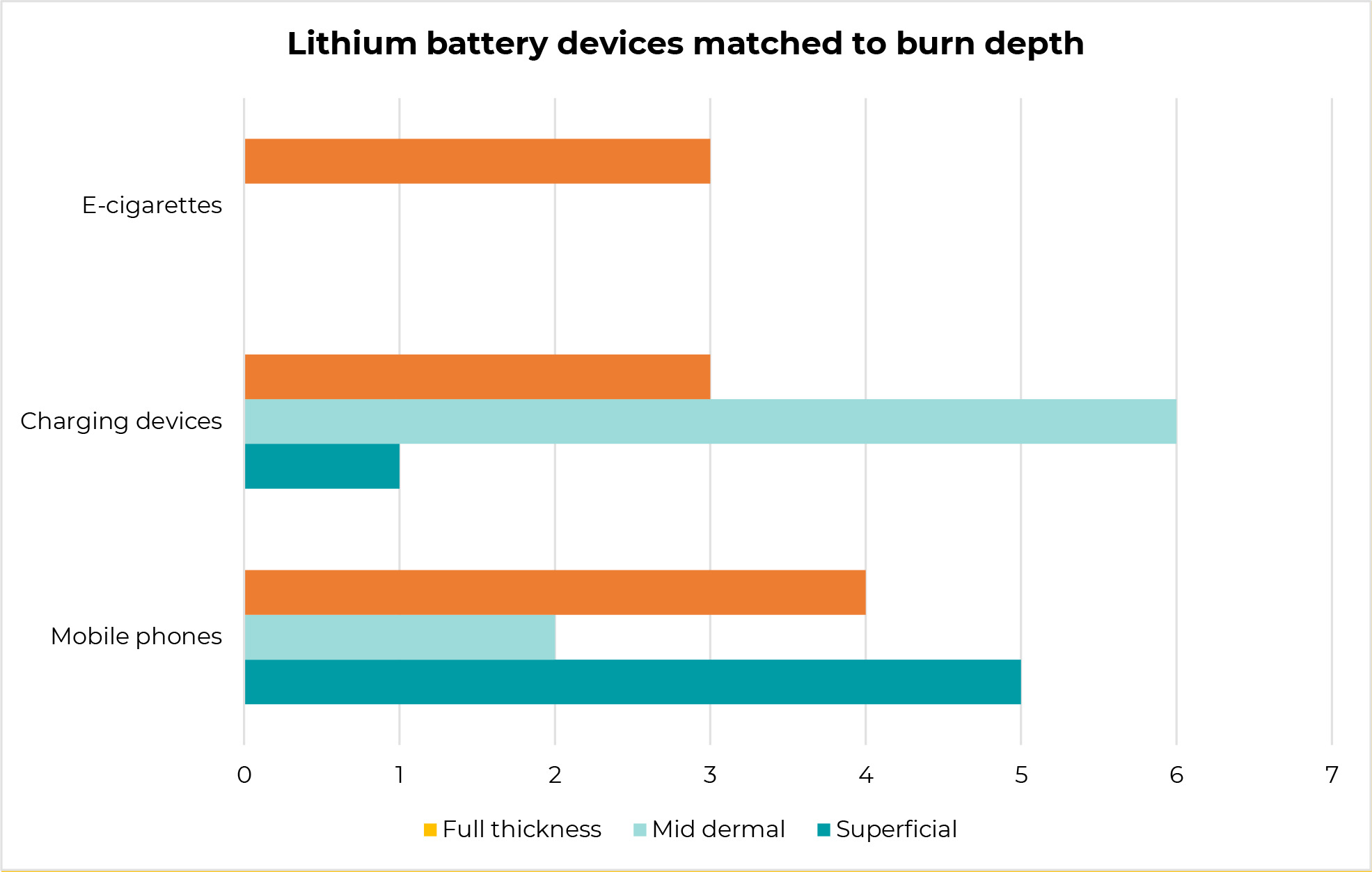
The most common source of injury originated from phone batteries (n = 11), portable charging batteries (n = 10) and e-cigarette devices (n = 3). The administration of cool running water for a minimum of 20 minutes as first aid was identified in 14 cases (58%). The most common site affected was the lower limb (n = 9) notably the thigh (Figure 1), followed by the upper limbs and multiple regions respectively (n = 6). The majority of injuries occurred in summer (n = 11). Most patients presented to an outpatient clinic (n = 21). Ten patients sustained full thickness injuries, followed by mid dermal injuries (n = 8) and the remaining superficial injuries (n = 6) (Table 1). Phone battery devices and charging devices resulted in a spectrum of superficial, mid dermal and full thickness injuries (Figure 2). E-cigarette devices all resulted in full thickness injuries. There was a statistically significant association between the device of injury and degree of burn (p = 0.04).
Management
The majority of these cases (n=17) were managed conservatively with manual debridement and dressings. The remaining seven cases required operative intervention involving either split thickness skin graft (n=5) or xenograft dressings (n=2). There was one outlier case (case 23) with 21.0% TBSA who required multiple operations and suffered burn wound infection. Most cases (n=21) were managed in the outpatient clinic setting, however, the three full thickness injuries that were operated on had a length of stay ranging from seven to 21 days. The three full thickness injuries included spontaneous explosive flame burns from an e-cigarette device, phone battery and chargeable device respectively. Table 2 provides a summary of the patient characteristics and type of devices associated with the burn injury.
Discussion
This first Australian case series of burn injuries related to lithium batteries highlights the variation in presentation with a strong male predominance and complexity of managing burns from a health professional and public health advocacy perspective. The trends in incidents relating to lithium batteries are growing at a significant rate globally with variations in the presentation of burn types related to device use and popularity at the time.15 The types of explosive injuries have the potential for a mixture of flame, chemical, electrical and contact burns resulting in different types of injuries to soft and/or hard tissues.
Paediatric
The paediatric age group had a total of six cases including flame, chemical and electrical burns with an equal number related to a phone or battery device exploding. These presentations highlight the importance of history and examination in guiding optimal management. Jones and colleagues 2019 case series on e-cigarette burns recommended initial management with mineral oil as water is contraindicated for lithium due to a risk of exothermic injury to tissues.16 For the initial assessment of a burn in an emergency department or clinic this seems valid, however, all of the paediatric injuries occurred at home where running water, as adequate first aid in the immediate setting, has priority. Detailed history from parents reported spontaneous explosions with no awareness that a device was heating up prior to an event. The danger is even greater if an actual blast explosion occurs as airways can be compromised with the release of toxic substances such as carbon monoxide, carbon dioxide and hydrogen fluoride which pose serious health threats in confined environments.17
Adult
E-cigarettes
Commonly known as vaping, e-cigarettes use lithium batteries to convert liquid nicotine into perfumed vapour. A literature review on adolescences smoking e-cigarettes found that they are more likely to be male, of older age, have a higher amount of pocket money, smoke regularly and heavily and have peers who smoke.18,19 Our adult age group had a total of 18 cases with a mix of burn types including flame, chemical, electrical and contact burns with more males affected than females. Interestingly, our series did not reflect the many reported global cases of explosion injuries from e-cigarettes resulting in serious soft and hard tissue injuries of the face, limbs and neck.20–25 Our experience noted an increase in findings of e-cigarette related burns from 2016 onwards reflective of the growing popularity of these devices and consistent with an increase of e-cigarette use reported from 2016 to 2019 in Australia.26 Data from the Burns Registry of Australia and New Zealand (BRANZ) in New Zealand reflects similar trends to our experience with notable incidences of malfunctioning phone devices, portable charging devices and e-cigarettes relating to fires reported from 2014 onwards.27
Ramirez and colleagues’ 2017 series of 30 patients who had injuries from e-cigarettes reported a male predominance of mean age 30 years with thighs, hands and genitalia commonly affected (mean TBSA of 4.0%) and nine patients requiring surgery.28 Our three e-cigarette explosions involved spontaneous combustion in the pocket that resulted in full thickness injuries to the lower and upper limbs (TBSA 0.6 – 9.0%), where two of three patients required debridement and split thickness skin grafting. These spontaneous explosions raise questions about manufacturing standards and the safety of devices. None of the patients in our series were carrying metallic objects in the same pocket as the e-cigarette when the explosion occurred, as has been reported elsewhere.29,30
Seitz and colleagues’ 2018 systematic review of 164 cases showed that most patients were male (9:1) between the age of 20–29 years with the majority (65%) of e-cigarettes exploding in pockets leading to thigh and genital burns, compared to exploding in the face or hand. The burns were typically deep partial burns (35%) or a combination of deep partial or full thickness burns (20%) with 48 patients (29%) required skin grafting with a median hospital stay of five days.31 To ensure prevention of ‘thermal runway’ and safe designs, Brown and Cheng recommend that manufacturers use circuits that protect against overcharging, integrate cut-offs for thermal power, and use internal overpressure relief mechanisms.32
Phone devices and chargeable devices
Case reports have documented spontaneous explosions of phone devices with and without the use of charging stations and without warning about overheating.33–35 In the media, there have been safety reports from mobile phone manufacturers leading to recalls of devices due to short-circuiting.36 These devices, similar to e-cigarettes, have potential to cause a combination of chemical, flame and contact burns with potential to cause significant disability and the need for ongoing rehabilitation. Their proximity to thighs and hands while in use risks serious morbidity owing to the potential for soft and hard tissue damage caused by these types of explosions.
There appears to be more literature on e-cigarette devices exploding than phone devices, however, our series showed a wide variety of injuries from phone devices in children and adults prior to 2014 when e-cigarette popularity increased significantly. Manufacturers have created internal devices to detect and monitor electrochemical changes that may lead to explosions including: thermal stability separators that detect variations in temperature, solid electrolytes which are less combustible and flame retardants such as polymer binders in the device framework to reduce fires in solid state materials.37
Recommendations
We recommend stronger transparency for public education and access regarding safe use including clearly labelled lithium batteries with key standards for safe operation such as maximum charging rate, cell voltage and correct charging with safe disposal.38,39
Globally, the standards for battery operating equipment and testing fall under different jurisdictions with no international consensus on industry design and performance-based test methodologies.40 There are gaps between the industry, research, fire departments, consumers, stakeholders and burns units where collaboration and sharing of information about these incidents could help to facilitate improvements, integration and harmony across sectors. As a result of these potential dangers, The International Civil Aviation Organization has prohibited airplane passengers and crew from carrying e-cigarettes and other battery-powered portable electronic smoking devices in checked baggage, and from recharging the devices in aircraft cabins.41 Health professionals must therefore advocate for consumers for safety warnings of potential explosions and inform the Australian Competition and Consumer Commission (ACCC) when injuries occur.42
Limitations
The limitations of this study reflect the retrospective nature of the data collection process. Since the rise of e-cigarettes in 2007, and particularly after 2014, we have noted more cases presenting to burns units but this may not have been captured in the data at the time. The small sample size, collected over a period of 15 years, reflects the limited research that has been undertaken in Australia and New Zealand on the number and impact of lithium battery related burns. With a small sample size, descriptive statistics highlight interesting points and statistical association between depth burn and devices. This research is one of the largest series specifically on lithium battery devices that will add value to the growing literature and incidents reported on related fires and how to better educate consumers and health professionals.
A further limitation with the collection of data was the lack of objective measurement tools for burn depth assessment such as laser Doppler imaging and therefore may be subject to inter-observer bias. Burn depth is most often assessed clinically and there are some variations in treatment across units.
This statewide case series highlights the impact these injuries have on both paediatric and adult patients with potential for soft and hard tissue injury. Health professionals should be informed about trends associated with the use of lithium-ion powered battery devices.
Conclusion
Lithium battery related burn injuries pose a modern challenge for burns professionals and health practitioners and a serious risk to children and adults of soft and hard tissue injuries from a combination of flame, chemical, electrical and contact burns. The nature of the injury and the severity of depth related to these everyday devices beckons regulation on the manufacturing and improved dissemination of safety information.
Acknowledgements
We would like to extend our acknowledgement to the burns team members at all three units who provided ongoing support for this research. We wish to thank Anne Darton and the SBIS Data Registry of the NSW Agency for Clinical Innovation for their assistance with data acquisition.
Patient consent
Patients/guardians have given informed consent to the publication of images and/or data.
Disclosure
The authors have no conflicts of interest to disclose.
Financial declaration
The authors received no financial support for the research, authorship, and/or publication of this article.
Revised: 2020 November 2; 2020 December 27; 2021 January 12