Introduction
Split-thickness skin grafts (SSGs) are a fundamental reconstructive technique for wounds of the lower limb. Exploring the most effective dressing for SSGs of the lower limb to maximise the rate of graft take will also minimise patient discomfort, improve postoperative QOL and decrease hospital expenses.
Traditionally, lower limb SSGs are dressed with a non-adherent dressing and a foam or gauze bolster that is secured by sutures, an elastic bandage or both.1 The bolster dressing immobilises the graft, preventing shearing between the graft and the wound. Dressing choice for skin grafts has been broadened with the introduction of negative-pressure wound therapy (NPWT). With NPWT, a non-adhesive perforated layer is applied over the skin graft followed by foam or gauze and a polyurethane film dressing. A suction device is then attached which maintains a constant negative pressure of between -125 and -80 mmHg.
The application of NPWT may reduce the incidence of graft loss due to shear forces, reduce the incidence of tissue oedema and improve management of exudates and haematoma compared with traditional dressings.2 The benefits are particularly useful on contoured skin graft beds such as lower limbs where bolster dressings may not be sufficient to maintain continuous contact of the graft with the graft bed.2 In 1998, Blackburn and colleagues used NPWT after skin grafting with promising results.3 Several later studies have shown NPWT to have the same or improved graft take compared with bolster dressings alone.4–9 Despite this, NPWT has not been universally adopted due to a variety of limitations, notably that dressings are large and cumbersome, limiting patient mobility and requiring home nursing. A recent survey of Australian surgeons found a link between NPWT use and an increased tendency towards early mobilisation for lower leg skin grafts.10
Adequate pressure is required to absorb exudate and conform the graft to the wound bed. Evangelista and colleagues showed no significant difference in graft take with grafts maintained at 50, -75, -100 or -125 mmHg pressure.11 Thus, a pressure of -75 mmHg appears adequate for graft take while resulting in less pain for the patient, reduced surrounding skin reaction and a lower risk of venous occlusion.
PICO (Smith and Nephew® 85 Waterloo Road, North Ryde, NSW 2113, Australia) is a dressing that provides NPWT in a smaller, more manageable format and it has recently become available in Australia. A PICO unit is about the size of a pack of playing cards and the dressing is waterproof, providing a portable and user-friendly format. Similar fluid handling, maintenance of negative pressure, wound contracture and blood flow have been found comparing standard NPWT and PICO.12
Traditional dressings for skin grafts have been shown to have success rates of 87–89 per cent.8,13 PICO dressings may be the answer to cumbersome NPWT dressings and improve graft take compared with standard dressings using the same principles of removing wound exudate and haematoma. We hypothesised that PICO dressings were non-inferior to standard dressings with regard to graft take of lower limb SSGs in adults.
Method
A prospective, randomised, controlled, open, single-site trial was performed to assess whether PICO dressings provide improved graft take success, easier dressing changes, lower complication rates and earlier ambulation in comparison with standard dressings for lower limb SSGs. Ethical approval for the trial was granted by the Human Research Ethics Committee at Peninsula Health [HREC/14/PH/25].
Recruitment for the trial ran from February 2015 to September 2017. Potential participants were recruited from the Frankston Hospital plastic surgery outpatient clinic, referring clinicians, emergency department presentations or the investigators’ private clinic.
This study included all patients requiring SSG to the lower limb for any aetiology with the following exceptions:
a. patients under the age of 18
b. those who had infected wounds
c. previously confirmed and untreated osteomyelitis
d. malignancy in the bed or margins of the wound
e. necrotic tissue with eschar present
f. exposed arteries, veins, nerves, bones or tendon
g. a wound that was greater than 15 × 20 cm or more than 2 cm deep and
h. those who had cognitive impairment or concomitant conditions preventing mobilisation.
Informed consent was obtained from each patient prior to patient screening and data collection. Participants were randomised into each group once in theatre. A sealed envelope was sent to theatre, determining whether the participant was in the standard dressing group or the PICO group. Randomisation was revealed at the induction of anaesthesia for each patient. If the patient had multiple wounds receiving SSG, each wound was randomised separately to a treatment group.
All wounds were prepared for skin grafting including debridement or regular dressings, if required. In the operating theatre a preoperative dose of intravenous cefazolin or equivalent, as required by the patient’s allergies, was given on induction of anaesthesia. Ongoing intravenous antibiotics were given if clinically indicated, such as a previously infected wound that was critically colonised with bacteria. All anticoagulants apart from aspirin were ceased preoperatively. Clexane was given perioperatively if required with oral anticoagulation recommenced within 24 hours.
A SSG 0.25–0.3 cms in thickness was obtained from the patient’s thigh using an electric dermatome machine meshed at a ratio of 1.5:1 and stapled, glued or sutured to the margins of the recipient bed. The standard bolster dressing was a non-stick contact layer followed by gauze or foam, then Velband®, (BSN Medical Australia, 211 Wellington Road, Mulgrave Victoria 3170, Australia) crepe bandage and Tubigrip (Mölnlycke, Gamlestadsvägen 3C 415 02 Gothenburg, Sweden).
The packaging was sterile and the dressings were stored at room temperature. PICO dressing has a silicone contact layer and absorbent pad with a 200 mL fluid-handling capacity. PICO dressing size was determined for each patient to allow the inner gel pad to fully cover the grafted area with the port placed away from the wound. All dressings in both treatment groups were changed at five to seven days postoperatively. Thereafter the PICO dressings were converted to standard dressings and both groups had dressing changes every 24–48 hours depending on wound condition until complete wound healing. Patients were mobilised as per the surgeon’s normal postoperative protocol.
Data were recorded at specific time points—preoperatively, first follow-up with dressing change at postoperative days five to seven (follow-up 1), days 10–14 (follow-up 2) and days 21–28 (follow-up 3). Wound tracings were drawn on acetate sheets placed over the graft—these included outlines of graft regions that had not taken or had questionable graft take. Graft surface area was measured using these tracings with a Visitrak® (Smith and Nephew, 85 Waterloo Road, North Ryde, NSW 2113, Australia) wound measurement device.
The primary outcome measure was skin graft take rate. This objective clinical assessment was calculated by expressing the healed graft surface area as a percentage of the total wound area measured at the same follow-up visit. A clinically successful graft take was defined as at least 80 per cent graft take of the total wound area.
The secondary outcome measure was health-related quality of life (QOL), which is a subjective clinical assessment based on the validated QOL questionnaire, WoundQoL. This questionnaire has been validated for assessment of health-related QOL in chronic wounds.14
Data were entered into an Excel spreadsheet (Microsoft, Level 24-30, 1 Denison Street, North Sydney NSW 2060, Australia) and once complete, imported into the statistical analysis software Stata version 14 (StataCorp LLC, 4905 Lakeway Drive, College Station Texas 77845, USA). The distribution of continuous data was checked with the Shapiro-Wilk test for normality, which showed that none of the continuous variables was normally distributed. Therefore, all continuous data were described using medians and interquartile ranges (IQR) and comparisons of these data from groups treated with the standard versus PICO dressing used the Mann-Whitney-Wilcoxon rank sum test. This comparison for categorical data used Fisher’s exact tests.
In addition, generalised linear mixed models (GLMM) were used to compare multiple measurements made from each group with different time points and to account for some patients who had multiple wounds treated. As there were repeated measures from the same participants at different time points and, as some but not all, participants had multiple wounds treated, data structure was not independent and was not normally distributed as required for tests like analysis of variance (ANOVA). GLMM were used for continuous and categorical data, but separately for each outcome variable, and using the appropriate family (Gaussian or binomial, respectively) and link functions (identity and logic, respectively). In all cases, p < 0.05 was accepted as statistically significant.
Analysis
Study population characteristics
Seventy-two patients with 84 wounds were recruited. Thirteen patients with 13 wounds were excluded from further analysis (see [Figure 1](96711)) leaving 59 patients with 71 wounds available for analysis. Thirty-six wounds were treated with a standard dressing (14 male and 22 female) and 35 wounds with the PICO dressing (12 male and 23 female). The median age in the PICO and standard groups, 78 (25.5) and 79 (24) years respectively, was not statistically significantly different (p = 0.9), nor was the frequency of current smokers at 19 per cent of the standard group and 11 per cent of the PICO group (p = 0.27). In general, the population proportions were matched for recorded comorbidities and whether they were taking anticoagulants ([Table 1](96712)). However, patients were not matched for the type of anticoagulation therapy with more patients in the PICO group taking aspirin and more patients in the standard group taking apixaban, rivaroxaban or warfarin ([Table 1](96712), p = 0.03)
The wounds were matched for aetiology in the standard and PICO groups (p = 0.068) with the most common aetiology being excision of skin lesions (21/36 and 24/35 respectively), followed by trauma (13/36 and 5/35 respectively), infected wounds (1/36 and 4/35 respectively) and Mycobacterium ulcerans ulcer (0/36 and 2/35, respectively). All wounds in both groups were on the lower leg, with no difference found for particular lower leg location (p = 0.342). They were also matched for wound area. The median (interquartile range) wound area was 16 cm2 (25) in the standard group and 16 cm2 (22) in the PICO group, and was not statistically significantly different (p = 0.83)
Differences in treatment
There was no statistically significant difference in the frequency of antibiotics administered (p = 1.00) with 35/36 (97.2%) of patients in the standard group and 34/35 (97.1%) in the PICO group receiving antibiotic treatment. There was also no statistically significant difference in the antibiotic treatment duration between the two groups (p = 0.46), with six patients from each group receiving a single dose only and the longest duration of intravenous antibiotic treatment being five days for both groups.
Fixation methods included a mix of staples, glue and sutures with or without quilting. There was no statistically significant difference in the frequency of different fixation methods as 23/36 (63.9%) of patients in the standard group had peripheral fixation compared with 20/35 (57.1%) in the PICO group, while 13/36 (36.1%) and 15/35 (42.9%) respectively had both peripheral and central fixation (p = 0.63). At operation, the standard dressings used included Jelonet (Smith + Nephew, 85 Waterloo Road, North Ryde NSW 2113 Australia) with gauze (11/38), Jelonet with foam (5/38), Adaptic (3M, 3M Center, St Paul, Minnesota 55144-1000, USA) with gauze (6/38), Xeroform (Deroyal Industries, 200 Debusk Lane, Powell, Tennessee 37849, USA) (2/38), Mepitel (Mölnlycke, Gamlestadsvägen 3C 415 02 Gothenburg) with gauze (1/38) and not recorded (13/38).
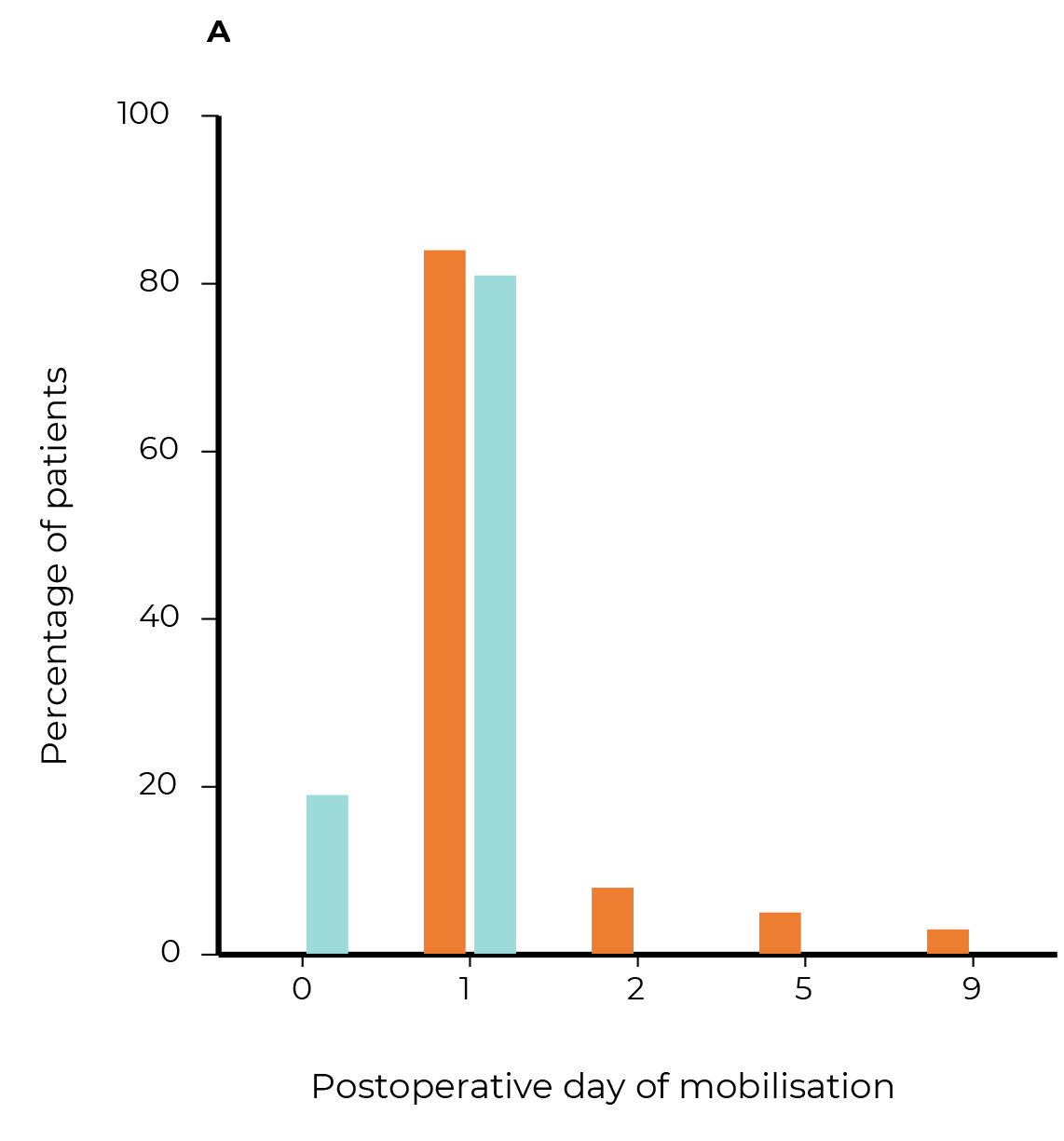
Patients were mobilised significantly earlier in the PICO group ([Figure 2a](96713), p = 0.003) with 100 per cent of patients in this group mobilised by postoperative day one compared with 81 per cent in the standard group.
Differences in patient reported outcomes
At the first follow-up, there was no statistically significant difference in reported pain on dressing removal (p = 0.77) with a median and IQR of two (5) and two (6) out of a maximum possible score of 10 reported by patients in the standard and PICO groups, respectively. At the first follow-up, 65 per cent of PICO users reported the ease of dressing removal as being ‘very easy’ or ‘quite easy’, compared with 55 per cent of those using the standard dressing ([Figure 2b](96714), p = 0.04). This difference was not sustained at later follow-ups, suggesting that the difference was specific to the dressing and not to differences in wounds or the pain tolerance of patients in the two groups. There was no statistically significant difference in patient reported comfort of the dressing (p = 0.21). In addition, there was no statistically significant difference in the median WoundQoL scores between the PICO and standard groups recorded either preoperatively or at the first postoperative follow-up ([Figure 2c](96715), p = 0.8 and p = 1.0 respectively).
Differences in graft take
There was no statistically significant difference between median percentage graft take treated with the standard versus PICO dressing on the first and second follow-ups (p = 0.16 and p = 0.23, respectively). Graft take for the third follow-up was statistically significant with a median (IQR) of 100 (6) per cent of graft take in the standard group versus a median (IQR) of 84 (19) per cent in the PICO group (Figure 3a, p = 0.02).
Differences in complications
One graft in the standard group failed at the first follow-up visit and was re-grafted. Four grafts in the standard group and three grafts in the PICO group had complete failure after the second follow-up and were managed conservatively. One graft in the standard group and three in the PICO group were complicated by infection requiring antibiotic treatment but these were all detected after the second follow-up, by which time both groups were being treated with standard dressings.
Compliance and loss to follow-up
A number of patients were discharged from the clinic with 100 per cent take of their graft and were assumed to have 100 per cent take for the remainder of the follow-up appointments. Follow-up attendance is summarised in [Table 2](96718).
Discussion
Lower limb wounds can take a long time to heal, fail to heal or can recur, causing significant pain and discomfort to the patient, decreased quality of life and increased cost to health services. Dressing improvements could make a significant difference in this area. Studies have reported that topical negative pressure is effective in treating large difficult and traumatic wounds,15,16 but there is a paucity of literature on NPWT use for lower limb SSGs. Our study found comparative graft take between the NPWT group and the standard dressing group, which is consistent with current findings in the literature.5,8
Despite advances in dressing options and perioperative management, graft failure and wound infection continue to be critical adverse events after surgery. Our study found no difference in failure and infection rates between the standard and PICO dressing groups but the rates of failure and infection were less than those reported in the literature with studies finding failure rates of up to one- to two-thirds.17,18 It is unclear why this is the case due to the number of variables present in studies evaluating graft take rates.
Patients were more likely to be mobilised earlier with the PICO dressing compared with the standard dressing. The timing of mobilisation was determined by the treating surgeon’s preference. Early mobilisation may prevent adverse events such as venous thromboembolism and deconditioning19,20 and may also reduce overall costs from hospitalisation.21 Evidence has shown that early mobilisation after SSGs to the lower limbs has no effect on graft take.22 A recent survey of Australian plastic surgeons found a tendency towards early mobilisation when NPWT was used compared with standard dressings, although the reason for this was not clear.10
The reason why patients with PICO dressings were mobilised earlier in our study is also unclear but it could be attributed to the surgeon’s belief that PICO dressings are more effective in providing graft to graft-bed contact and removing exudate than standard dressings. It would be interesting to repeat this study with a protocol for mobilisation to see whether this has an impact on graft take success.
The economic benefit of early mobilisation is logical given success rates of SSG are non-inferior compared with those who receive bed rest. Poole and Mills23 described the economic advantage of immediate mobilisation. In their retrospective study of 100 consecutive patients requiring SSG to lower limb lacerations, patients had a mean bed stay of 14.5 days, accumulating a NZ$551,390 aggregate cost associated with their care. None of these patients underwent early mobilisation, therefore it was suggested that significant savings would have been made if earlier discharges were sought. Furthermore, support for the economic value of early mobilisation is noted by Smith,24 Wallenberg25 and Shankar and Khoo26 in their studies. The economic analysis of standard dressings versus PICO dressings and a formal cost analysis is outside the scope of this study but could be a focus of further research.
The secondary objective of this study was to determine the superiority of PICO dressings with regard to health-related QOL of adult participants during their lower limb wound healing. There was no difference between pain on dressing removal, patient-reported comfort or median questionnaire scores but PICO dressings were found to be significantly easier to remove than standard dressings. Easier dressing removal may reduce patient follow-up times and therefore clinic wait times, improving the patient experience.
Limitations
Limitations in this study include the lack of analysis of wound depth, lack of a standardised postoperative mobilisation protocol, technical differences in the application of dressings, variable documentation at follow-up appointments and variability in ‘standard’ dressings. PICO dressings were used for the first five to seven days only. Grafts had frequently deteriorated by the third follow-up visit and we query whether NPWT should be maintained longer for greater graft stabilisation. A larger sample size could allow multivariate analysis in a future study.
Conclusion
PICO dressings are not inferior to standard dressings for graft take in adults with lower limb wounds. Patients in our study were more likely to be mobilised earlier with PICO dressings compared with standard dressings, which may have economic advantages. Patient quality of life was similar in both groups but PICO dressings were found to be significantly easier to remove.
Acknowledgements
We acknowledge Dr Vicky Tobin for her assistance with the statistical analysis of this paper and editorial input.
Conflict of interest
The authors have no conflicts of interest to disclose.
Financial declaration
The authors received no financial support for the research, authorship, and/or publication of this article.





_graft_take_at_follow-up_visits_for_pico_versus.png)




_graft_take_at_follow-up_visits_for_pico_versus.png)