Introduction
Amputations confer significant long-term issues with pain and physical and psychological disability. Many studies have reported a high prevalence of phantom limb pain (PLP) and neuroma-related residual limb pain (RLP) in amputees regardless of time since the limb loss. This negatively impacts prosthesis wear, resulting in chronic immobility and psychological distress.1–3 These issues and socioeconomic challenges are increased for multiple-limb amputees4 and are a disability subpopulation that are often overlooked and under reported. Best reported data comes from the USA, where approximately 185,000 amputations are performed yearly. A recent surgical technique called targeted muscle reinnervation (TMR) has shown promising results in reducing PLP and RLP, interference and intensity of pain with a prosthetic, and development of neuromas.5–11 Built on the findings by Elsberg and colleagues in 1917, whereby severed, transferred nerves in rabbits were shown to grow into existing intramuscular motor branches,12 it involves using the transected nerves to innervate new target muscles.7
Targeted muscle reinnervation also improves myoelectric prothesis control by bringing neuroelectric signals closer to the skin surface or increasing residual muscle contraction strength.13,14 In patients with traditional transradial amputations, residual muscles can only myoelectrically control simple movements in one degree of freedom at a time15 (for example, only flexion/extension or pronation/supination). If these limbs undergo TMR, simultaneous movements in multiple degrees of freedom can be afforded using pattern recognition control.6–8 This involves recruiting bulk muscle groups that the myoelectrically controlled prosthesis obtains signals from to perform specific movements such as pinch or supinate.
We present the first two cases worldwide of quadruple amputees that have undergone immediate TMR in a specialised centre with multidisciplinary team involvement. Our two aims were to reduce pain postoperatively and improve myoelectric prosthetic control, in accordance with the current literature on single amputees.
Methods
Between April and October 2018 at The Alfred Hospital, Victoria, two adult patients underwent TMR of all four limbs at the time of limb amputation in the context of necrotic limbs from sepsis. A retrospective case note review of patient progress was performed. All amputated limbs had muscle flaps raised distally to cushion the bone and serve as donor sites for nerve transfers. Motor and sensory nerves that were to be used for TMR were identified and tagged before nerve coaptations were performed using 8/0 and 6/0 monofilament under microscope guidance. Both patients completed The Alfred Hospital osteointegration survey (TAHOS) for each limb at six, 12 and 24 months post amputation. This novel questionnaire was created as there was no single comprehensive questionnaire available for amputees. It combines nine validated assessments: the Swedish prosthesis survey, brief pain inventory, Pittsburg sleep quality index, hospital anxiety and depression scale, pain catastrophising scale, SF-36, disabilities in the arm, shoulder and hand (DASH), and McGill pain questionnaires. A blank copy is provided for reference (Appendix A).
At three months postoperatively, both patients commenced motor imagery and gross motor patterns at The Epworth Hospital in Victoria. This retrains the motor cortex to generate signals to the coapted nerves as the patient visualises movements previously made with their whole limb. By 12 months, both had begun virtual reality prosthetic training with pattern recognition control.
Case series
Patient A
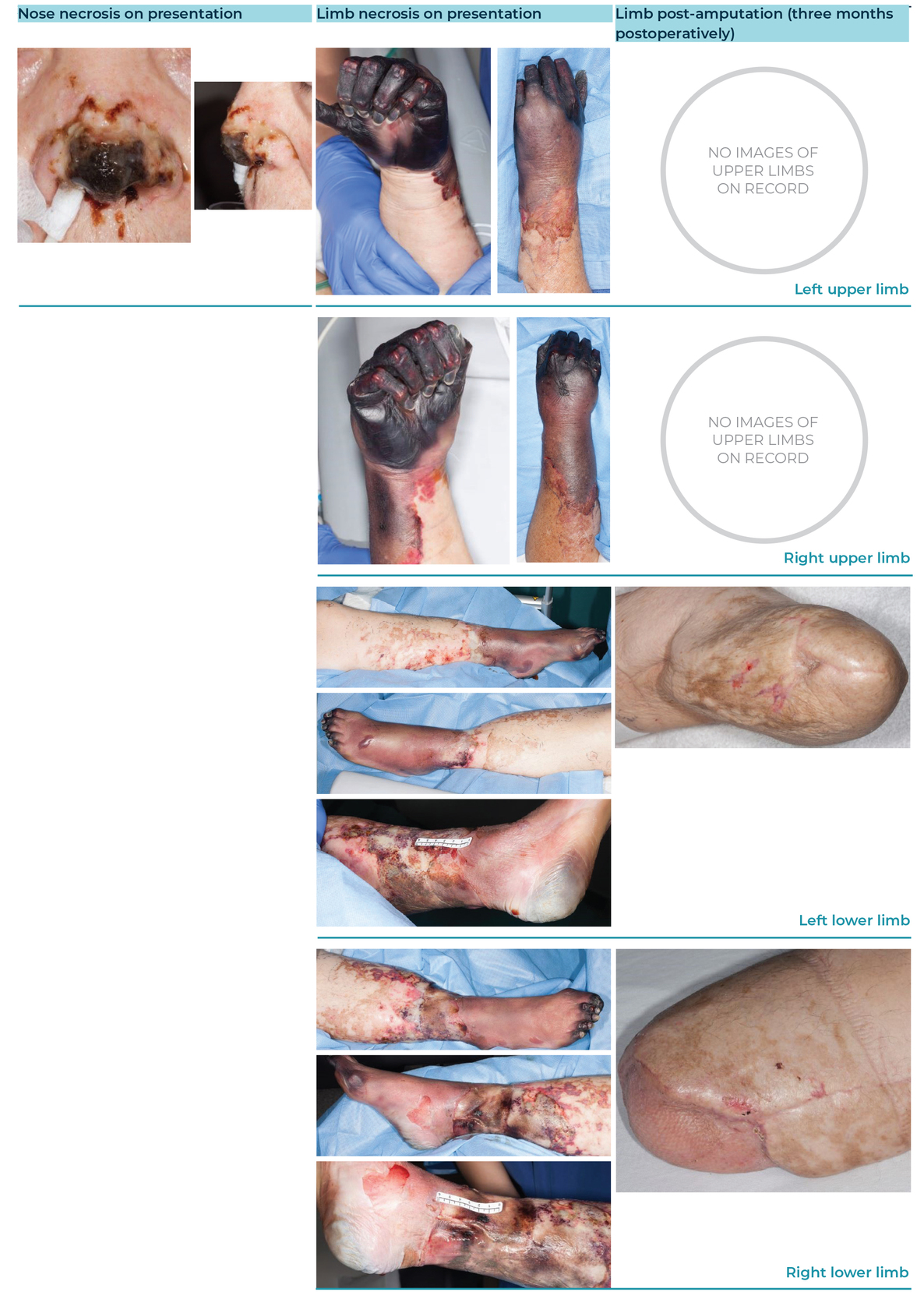
Patient A was a 55-year-old male who had meningococcal sepsis, later developing four limb necrosis unsalvageable by hyperbaric oxygen treatment. He underwent serial debridements, eventually resulting in bilateral transradial and bilateral transfemoral amputations (see Figure 1). Nerve coaptations are listed in Table 1. At three months postoperatively he was fitted with a right upper limb universal cuff allowing him to hold a single small item (for example, a toothbrush or fork). Analgesic use can be seen in Table 2.
At six months postoperatively, Patient A had ischial weight-bearing lower limb prostheses with silicon liners and seal-in suspension and body-powered upper limb prostheses with hook terminal devices (requiring physical movement of a joint to operate the distal end). The patient was wearing his upper limb prostheses seven to nine hours per day, four times a week. He recorded his overall activities being ‘slightly limited’ with ‘no difficulty’ in pushing open a heavy door or placing an object on a shelf above his head, and only ‘mild difficulty’ turning a key or using a knife to cut food. He did not have any PLP or RLP.
At 12 months, Patient A wore his prostheses less than three hours a day as he felt ‘life was easier without them’. Some self-reported functional abilities with his upper limb prostheses briefly reduced to ‘moderate difficulty’ at 12 months before improving to ‘mild’ or ‘no difficulty’ at 24 months, such as turning a key or using a knife to cut food. At 12 months, he was able to walk unaided in the home and on even ground outside, and stand up from a chair with one assistant.
Patient A only recently obtained definitive myoelectric controlled prostheses for both upper limbs. Despite this, at 24 months he reported ‘no difficulty’ in many tasks previously listed as ‘mildly difficult’ or ‘unable to perform’, such as doing heavy household chores, recreational activities which required force through the arm (for example, golf or tennis) and managing transportation needs. Physiotherapy and prosthetist assessments agreed with an objective functional improvement for bilateral upper limbs when performing tasks (such as cutlery manipulation and collecting items from shelves) and the patient is developing control within multiple positions in space.
Patient B
Patient B was a 69-year-old female who had streptococcal pneumoniae sepsis complicated by disseminated intravascular coagulation (DIC) and multiorgan failure resulting in four-limb necrosis and nasal tip eschar. Like Patient A, Patient B failed limb salvage with hyperbaric oxygen therapy and underwent serial debridement resulting in bilateral below knee amputations (BKA) and bilateral trans-radial amputations with immediate TMR to all four limbs (see Figure 2). Her nerve coaptations are listed in Table 1.
At six months, Patient B was wearing a right lower limb prosthetic and had just received her left upper limb transradial two-site control myoelectric prosthesis. The latter allowed her to use a simple utensil, such as a fork. Due to this, she recorded being unable to perform any tasks that Patient A had been able to perform at the same time, such as opening a heavy door or turning a key. Patient B recorded an RLP of 1/10 in her left lower limb on average and was not using any analgesia.
By 12 months, Patient B was wearing bilateral lower limb prostheses 10–12 hours a day and bilateral upper limb prostheses up to three hours a day. Due to this increased use of prostheses, in contrast to Patient A, she recorded performing the following unaided: standing up from a seated position, walking indoors or outside on even ground, walking while carrying an object and walking upstairs with a handrail. With one assistant, she was able to walk outside on uneven ground. At an occupational therapy assessment, she had good control of three prehension patterns (power, lateral and pinch grips) and forearm rotation (supination and pronation) bilaterally. As seen in Table 2, she had no PL or RL pain and did not require analgesics.
Function continued to improve for Patient B at her 24 month follow-up. She recorded being able to pick up an object off the floor alone while standing, walk across the room carrying a tray in both hands and step up and down a kerb, all while someone was near but not assisting. These were previously recorded on her six and 12 month TAHOS as requiring an assistant or being unable to be performed entirely. Her previously recorded unaided abilities continued to her 24 month TAHOS. Due to COVID-19, Patient B chose to delay further follow-up and have physical therapy via TeleHealth.
Discussion
Targeted muscle reinnervation in amputated limbs is a technique that has garnered increasing success for preventing and treating neuroma-related residual limb and phantom limb pain. Our two quadruple amputee patients had an average of 1/10 neuroma-related residual pain by six months postoperatively and no pain by this time, achieving our first aim.
Our second aim of improving myoelectric control was also achieved whereby Patient B showed intuitive control with virtual prostheses for bilateral upper limbs by six months while fitted with a left upper limb myoelectric prosthesis and both patients gained marked improvements at 24 months both in self-reported and objective assessments in prosthetic control.
Conclusion
We present the first two cases globally of quadruple amputees who have undergone immediate targeted muscle reinnervation. Used in a specialised centre with a multidisciplinary team, it has clinically important benefits in major amputees by reducing or eliminating neuroma-related residual limb and phantom limb pains and improving myoelectric prosthetic control.
Patient consent
Patients signed informed consent regarding publishing their data and photographs.
Conflict of interest
The authors have no conflicts of interest to disclose.
Financial declaration
The authors received no financial support for the research, authorship, and/or publication of this article.
Revised: 18 July 2020, 9 December 2020