Background
Mycobacterium szulgai (M. szulgai) is a rare human pathogen, first discovered in 1972 and identified in pulmonary infections, olecranon bursitis and cervical adenitis.1 The first case of carpal tunnel syndrome (CTS) secondary to tenosynovitis caused by M. szulgai infection was reported by Stratton, Phelps and Reller2 in 1978 in a young florist— this was the fifteenth overall case of M. szulgai infection documented in the literature. Australia’s first reported case of M. szulgai was a pulmonary infection in 1981.3
Non-tuberculous mycobacterial tenosynovitis is a rare condition, more typically caused by M. marinum followed by M. kansasii.4 Patients typically present with chronic swelling without signs of acute infection, and normal ESR/CRP inflammatory markers.4 It is difficult to diagnose and is frequently misdiagnosed, which often results in delay to treatment (on average roughly six months).4
Case report
A 54-year-old right-hand dominant male presented complaining of six months’ history of gradually worsening right CTS symptoms. There had been intermittent mild symptoms for the preceding three years with deterioration in the past six months. The patient had undergone a steroid and local anaesthetic injection six weeks previously with symptomatic relief. However, the symptoms recurred and were not improved with a subsequent repeat steroid injection four days prior to his presentation. There was no history of trauma. Past medical history included gout and type II diabetes mellitus (managed with metformin).
The patient was born in Vietnam prior to immigrating to Australia 36 years ago. There was a history of frequent travel, particularly to south-east Asia. The patient had previously had the bacillus Calmette-Guerin (BCG) vaccine and currently worked as a welder.
On examination there was considerable swelling of the right wrist with volar tenderness and reduced range of motion. There were no signs of acute infection or inflammation, and no fever. Passive extension of the right index and middle fingers elicited pain in the palm but there was no flexor sheath tenderness. The patient reported reduced sensation in the median nerve distribution, with concomitant motor weakness of the thenar muscles.
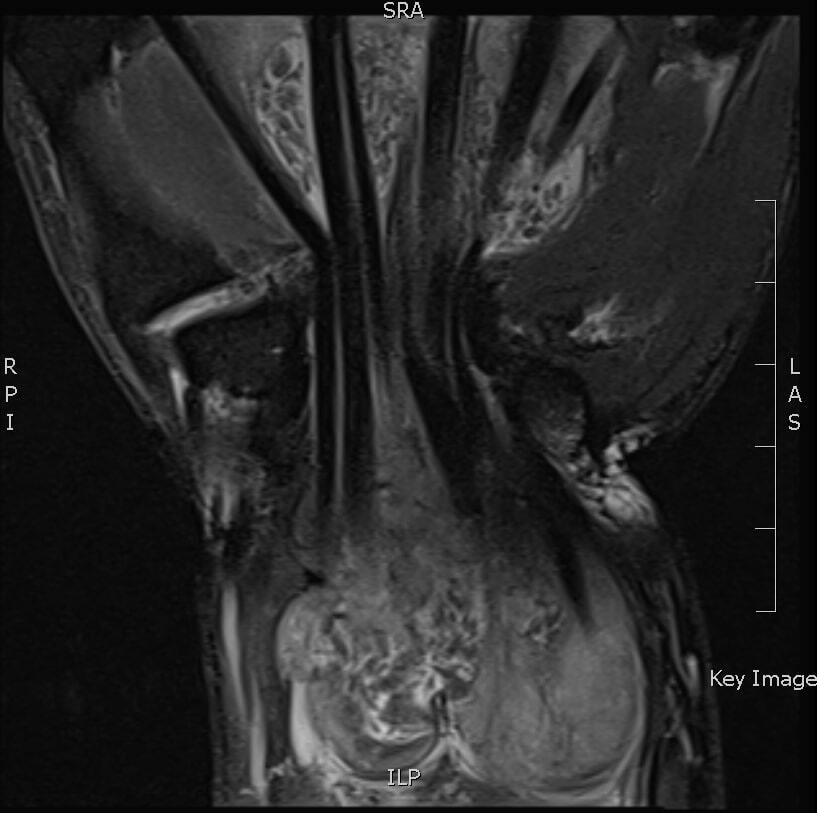
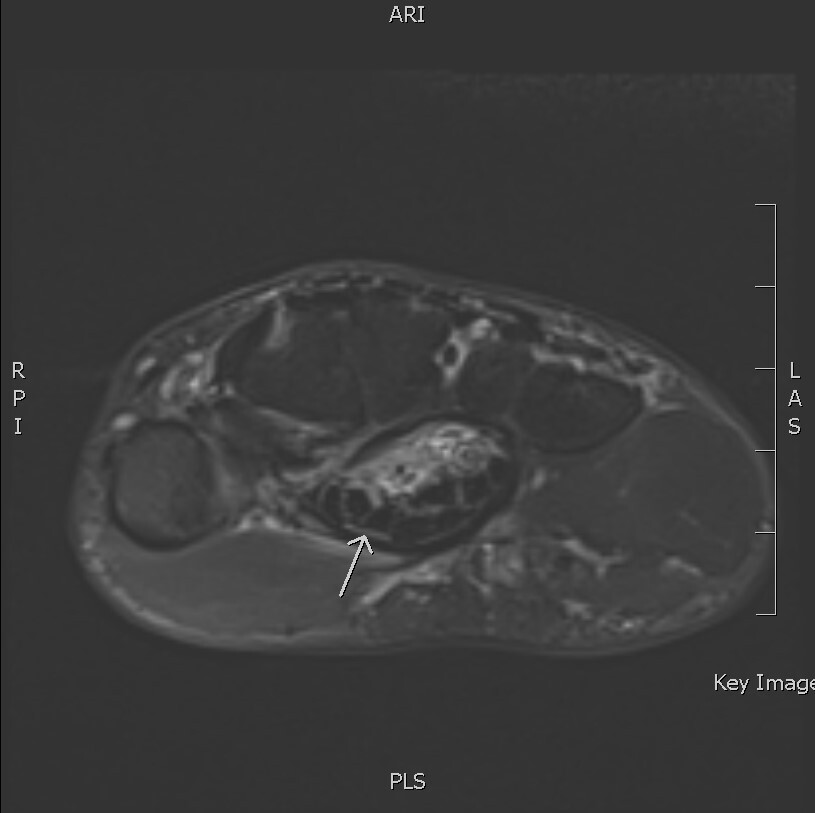
Plain film X-ray was unremarkable. Blood tests showed a normal white cell count (7.9) and C-reactive protein (CRP) for inflammation (5.5). Magnetic resonance imaging of the right wrist was performed (Figure 1) given the atypical picture of subacute CTS and for operative planning of synovectomy. This showed a large collection approximately 10 cm in length centred in the carpal tunnel but extending into the hand and distal forearm. The loculated mass enveloped the flexor tendons. There was marked compression of the median nerve to one millimetre in the carpal tunnel (Figure 2).
The appearance of multiple small rice bodies yielded a differential diagnosis including fungal or tuberculous synovitis, sarcoidosis, autoimmune conditions (including rheumatoid arthritis) and gout. Rheumatoid factor and anti-cyclic citrullinated peptides (anti-CCP) were normal. A rheumatology consult concurred with the favoured provisional diagnosis of infective rather than inflammatory arthritis.
The patient proceeded to surgery for right wrist synovectomy and extended carpal tunnel release. A pseudo-capsule containing multiple rice bodies with associated florid synovitis encompassing the flexor tendons and deep to the median nerve (Figure 3) was excised and sent for microscopy and culture.
On review the next day the patient’s median nerve paraesthesias had considerably improved. Given the suspicion for atypical infection, an infectious disease consult was sought. The patient had no systemic symptoms of tuberculous disease and no known exposure to potential contacts. Chest X-ray was negative for pulmonary tuberculosis.
Histology showed a florid granulomatous synovitis with sarcoidal-type granulomas. No acid-fast organisms were identified with Ziehl-Neelsen and Wade-Fite stains. QuantiFERON and tuberculosis polymerase chain reaction (PCR) testing were negative.
Two weeks after surgery, one of three cultures from surgery returned positive for M. szulgai. On the advice of infectious disease specialists, the patient was started on 12 months’ treatment with rifampicin and clarithromycin antibiotics.
Overall recovery of hand function was excellent. Five months postoperatively the patient had normal hand sensation and fist formation. The patient was discharged from hand therapy, having returned to work as a welder. There had been no recurrence or requirement for re-debridement at the time of writing (nine months postoperatively), with the patient tolerating the antibiotic regimen without issues.
Discussion
Subsequent to the initial report of CTS secondary to M. szulgai in 1978,2 there were further similar presentations,5 including two patients who had cleaned a fish tank with their bare hands.6
Mycobacterium szulgai is known to be present in certain environments such as fresh water, tropical fish and plants, which have been suggested as potential sources of human infection.7 Most recently, a case of CTS from M. szulgai-associated tenosynovitis was reported in the owner of a Mississippi mud turtle.8
On subsequent further questioning, it was discovered that our patient had in fact kept pet goldfish in an aquarium for approximately fifteen years. The patient reported cleaning the aquarium with his bare hands, and did not keep any other species of fish or turtles.
Overall, many aspects of this patient’s history and examination reinforce trends in the limited literature available regarding non-tuberculous tenosynovitis presenting as CTS. Particularly, there were no classic signs of infection and inflammatory blood markers were normal. A notable risk factor for this patient’s presentation was environmental exposure to fresh water/aquariums, which has been similarly reported by two institutions for M. szulgai-associated tenosynovitis.6,8 The preceding steroid injections may also have unmasked a latent infection for this patient, similar to the hypothesised role of systemic steroids in the presentation reported by Harvey and Russell.8
Conclusion
This is the first known Australian case of M. szulgai-associated tenosynovitis presenting as CTS. Non-tuberculous mycobacterial infections should be considered in the differential diagnosis as an unusual cause for this presentation, although M. szulgai remains an uncommon bacterium for this clinical picture compared with other non-tuberculous mycobacterial species. The presence of rice bodies on imaging and at surgery is highly suggestive of this type of chronic tenosynovitis. The major risk factor identified thus far for this infection appears to be exposure to aquatic environments.
Prior publication
This paper is based on a poster presentation from the Royal Australian College of Surgeons’ Annual Scientific Congress 2020.
Patient consent
Patients/guardians have given informed consent to the publication of images and/or data.
Conflict of interest
The authors have no conflicts of interest to disclose.
Funding declaration
The authors received no financial support for the research, authorship, and/or publication of this article.
Revised: July 15, 2020 AEST