Introduction
Cerebral palsy (CP) is a term describing a group of movement and posture disorders due to a non-progressive lesion in the developing brain, with a prevalence of approximately two in every 1000 live births.1–4 The neurological injury can be acquired pre-, perior postnatally. Most commonly, injury is caused by fetal or neonatal challenges such as prematurity, anoxia, trauma at birth, congenital defects and/or postnatal injury.5 The nature and severity of motor impairment vary depending upon the extent of the brain lesion and the anatomical region/s involved.6,7 The cerebral damage can also result in concurrent deficits in cognition, sensation, vision, hearing and speech and increased risk of epilepsy.7 These factors make this population highly heterogeneous in nature.
Impaired hand function affects 83 per cent of children with CP.8 It is the main concern in more than 50 per cent of children with hemiplegic CP.9 Upper limb deficits can impact a child’s manual abilities, cause pain, impair hygiene, alter the cosmetic appearance of the limb/s, cause psychological distress, reduce the individual’s independence and increase carer burden.6 The International Classification of Functioning, Disability and Health (ICF) is the World Health Organization’s framework for describing the effects that impairment has on an individual.10 It takes into consideration the person’s function and the environmental and personal influences affecting their function.
A variety of treatment options are used to reduce the impact of upper limb impairment due to CP. These include rehabilitative therapy, splinting, anti-spasmodic/dystonic medications, botulinum toxin injections, and surgery. Surgery occurs in fewer than 20 per cent of individuals.11 Research shows that surgical intervention provides better functional outcomes compared with non-surgical interventions when careful patient selection is taken into consideration.12,13 However, the evidence base is limited.14 Multiple surgical procedures can be completed within the one anaesthetic episode, known as single-event multi-level surgery (SEMLS). During SEMLS, musculoskeletal structures are altered to facilitate improved muscular control, tissue length and joint stability. Surgical approaches may include musculotendinous lengthening or releases of the deforming spastic muscles, tendon transfers to augment paretic muscles, and joint stabilisations.7,15–19 A SEMLS approach is the preferred method of surgical intervention as it reduces the quantity of hospital visits and anaesthetic episodes while maximising functional impact.15
There is considerable variation in both research and clinical practice regarding the method of patient selection, pre- and postoperative assessment of upper limb function, and the type of surgeries used. A literature review revealed both an absence of data specifically reviewing the baseline characteristics of individuals being selected for surgery and a lack of consistent use of valid and reliable outcome measures. Selection appears to be determined by a historical cluster of characteristics based on conflicting evidence. These characteristics include: age, type and degree of motor impairment, sensory integrity of the limb, cognitive capacity and goals of the intervention.
Currently no routinely recognised clinical guidelines exist to help select individuals who would benefit most from operative intervention. Assessing children with CP for potential upper limb surgery is complex. Baseline characteristics and goals of care can differ for each individual.7,11,20 Clinical decision-making should be made through the integration of information obtained from clinical history, physical examination, radiographic interpretation, motion analysis and examination under anaesthesia.6,11,12,21 A collaborative team of surgeons, rehabilitation physicians, neurologists, paediatricians, physiotherapists, hand therapists, occupational therapists and social workers should assess the patient for eligibility for surgery.11,16,21–23 Assessment of the individual’s baseline characteristics, lifestyle, care goals, motivation and cognitive capacity informs the team towards the most appropriate form of treatment, including surgery.16,22,24
The heterogeneity of this population makes it challenging to collect data to best inform management and potential for functional improvement. However, heterogeneity does not preclude recognition of useful information to guide intervention. The evolution of the Gross Motor Function Classification System (GMFCS), prognostic curves and resulting surgical management guidelines for the lower limb in CP is evidence of this.25 However, it is important to note that the upper limb is more functionally complex compared with the lower limb. In 2006, the Manual Ability Classification System (MACS) was developed. It is recognised as a valid and reliable measure of upper limb function.26 It measures the individual’s functional ability when using both hands in concert, rather than the maximum ability of the most affected hand only.27 This is a key step towards understanding the functional ability of an individual, their goals of surgery and expectations of functional outcome.
The aim of this study is to evaluate the current methods of assessment and selection of surgical candidates for upper limb management in CP. This will assist in determining what clinical characteristics are currently considered suitable for surgical intervention and determine whether historically accepted characteristics are in line with clinical practice.
Materials and methods
Study design
This study is a retrospective case series. Suitable individuals were identified in collaboration with the Department of Health Information Services at the Royal Children’s Hospital (RCH), Melbourne, Australia. A search was performed with the IBA Health’s patient administration system using the International Statistical Classification of Diseases and Related Health Problems (ICD) ICD-10 code for the diagnosis of CP. This was narrowed by only including individuals who had been admitted to the RCH by the Department of Plastic and Maxillofacial Surgery between 1 January 2008 and 31 December 2017 (a 10-year time period). The list was cross- checked using the operating room management information system to remove admissions for surgical events other than for the management of upper limb motor impairment due to CP.
This study received ethics approval from the RCH Human Research Ethics Committee prior to commencement (reference number 37313A). It also received governance authorisation at the Melbourne’s Children’s Campus (including the RCH, Murdoch Children’s Research Institute and The University of Melbourne Department of Paediatrics). Data were de-identified and kept in accordance with ethics guidelines.
Setting
The RCH is the major tertiary paediatric centre of the state of Victoria, Australia. All individuals with CP requiring upper limb surgery at the RCH are assessed by the Department of Plastic and Maxillofacial Surgery. This study was undertaken in the Rehabilitation Department in collaboration with the Department of Plastic and Maxillofacial Surgery.
Data collection
Relevant information was extracted from the patient files of each individual. Extraction was performed solely by the primary investigator to ensure reliable interpretation. A second investigator independently collected data from the first three files processed. There was 100 per cent inter-examiner reliability across all data points.
Information from patient files between February 2011 and December 2017 was available on Epic Systems (1979 Milky Way, Verona, Wisconsin, WI 53593, United States of America), the electronic system used by the RCH. Older information was obtained through recall of archived paper files. The data were managed using REDCap (2 Nd Street, Ste 500, Encinitas, California 92024, United States).
Due to the retrospective nature of this study, collecting data regarding the predominance of motor impairment type was not possible. Documentation often did not explicitly note whether, for example, the dystonia or the spasticity was the predominant motor characteristic within a mixed patient. Therefore, motor impairment categories could be determined only by the presence of a type, or types, of impairment irrespective of its relative severity.
Goals of surgical management were included only when specifically referenced preoperatively. Position care was considered a goal where the aim of repositioning the limb was for a reason other than function for an activity or participation, hygiene, cosmesis or comfort; for example, improving ease of dressing for the caregiver. Cases where improved posturing was sought for better use as a stabilising hand were considered an activity goal rather than a position care goal.
Cognition was categorised as ‘impaired’, ‘intact’ or ‘not recorded’. An individual was considered impaired only when there was a diagnosis of intellectual disability or an IQ < 70 was recorded.
The recorded level of MACS and GMFCS often varied within a patient’s file, differing between health professionals and visits. All functional levels attributed to the individual were recorded.
Only objective outcome measures were included for perioperative assessment. Range of motion (ROM) was included only if numerical values were identified.
Operations were considered separate when they were performed under a different episode of anaesthesia. Removal of K-wires was considered follow-up care, not a separate surgical event, and thus was not recorded.
Ethics
This study received ethics approval from the RCH Human Research Ethics Committee prior to commencement (reference number 37313A). It also received governance authorisation at the Melbourne’s Children’s Campus (including the RCH, Murdoch Children’s Research Institute and The University of Melbourne Department of Paediatrics). Data were de-identified and kept in accordance with ethics guidelines.
Results
During a 10-year time period, 102 individuals received surgery to the upper limb at the RCH for management of musculoskeletal impairments as a result of their CP. During this time, 138 separate operative events were performed. Details of patient characteristics are represented in Table 1 and details surrounding the surgical events are shown in Table 2.
Of the 102 individuals, 56.9 per cent were male and 43.1 per cent were female. The age at the time of surgery ranged from 4.9 to 25.8 years (median age 14.2) (Figure 1a). Motor involvement was 51.0 per cent bilateral and 49.0 per cent unilateral. The motor effects of CP were predominantly spastic with 62.7 per cent classified as purely spastic and 30.4 per cent as a mixture of spastic and dystonic (Figure 1b).
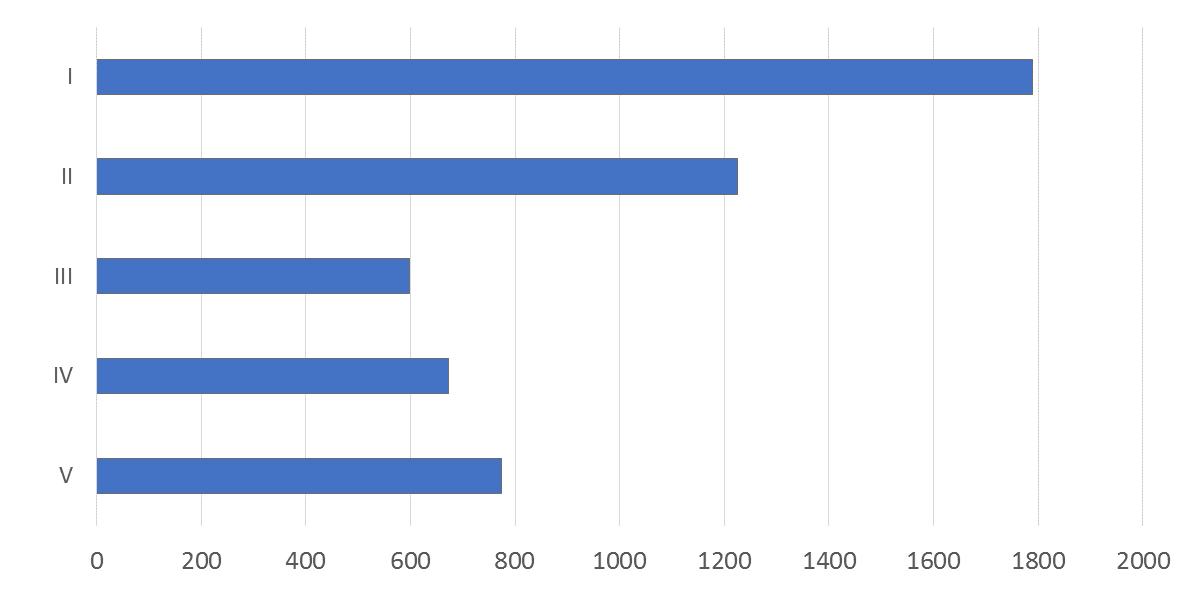
The functional ability of participants as per their recorded GMFCS and MACS level are charted in figures 1c and 1d respectively.
Preoperative goals were recorded in 87.7 per cent of cases. Often there were multiple goals for each surgical event, with the most common goal type being position care (50.4% of cases) (Figure 2). Preoperative outcome measures were used in 69.6 per cent of cases. The most commonly used was ROM (90.6%). Postoperative measures were used in 73.2 per cent of cases, whereby again ROM was most common (90.1%). Patient and/or caregiver satisfaction was not recorded in 68.8 per cent of cases.
Details regarding the surgical procedures performed can be found in Table 3. The number of procedures per surgery varied considerably, from a single transfer to extensive multilevel operations. The mean number of procedures per surgical event was 4.2, with a mean of 1.4 surgical events per patient.
Discussion
To date there has been no literature reviewing data specifically on the characteristics of individuals selected for upper limb surgery. The Australian Cerebral Palsy Register is a national database describing characteristics of the general population diagnosed with CP in Australia.28 Comparing the surgical cohort with this register can help reveal notable features specific to the surgical population. Due to the retrospective nature of this study and the small sample size, this should be interpreted with caution.
There were no marked differences between gender distribution in this study compared with that of the register. Study participants were 51.0 per cent bilaterally and 49.0 per cent unilaterally impaired, while the register reports 60.9 per cent bilateral and 39.1 per cent unilateral involvement. Thus, it may be possible that unilateral involvement is more commonly selected for surgery. Patients with unilateral involvement tended to have lower GMFCS scores of disability (Figure 3a) and their most common goal of surgery was improved activity and participation, while those with bilateral involvement tended to have higher GMFCS scores and most commonly sought improved hygiene and position care (Figure 3b). It may be possible that greater weight is placed on activity-related goals when determining whether to embark on surgical intervention.
The median age at surgery was 14.2 years old. Influential research regarding ideal age for surgical intervention does not currently exist for the upper limb, unlike for the lower limb. It is widely believed that early intervention is favourable.5,7,18,22,29,30 This is a balance between being old enough to adequately adhere to postoperative rehabilitation but young enough to intervene before severe contractures have developed. Intervention should reportedly be considered from six years onwards.5,7,29,31 Few interventional studies have been conducted into the influence age has on surgical outcome. Malizos and colleagues completed a small interventional study of 34 participants with cerebral palsy undergoing upper limb surgery, which observed that both the younger (four to 14-year-old) and older (15 to 34-year-old) participants received benefit; however, greater benefit was achieved with early intervention.22
Clinical recording of GMFCS was highly variable. For 96 individuals, 125 different GMFCS levels were recorded. Six had no recorded level. Some individuals were recorded across disparate functional levels, for example as both I and III, II and III, or III and IV. Factors that may have influenced this include different reporting clinicians and/or the patient history reflecting different functional levels depending on the questions asked and the details shared by the individual on that particular visit. Despite this, the data show that those sent for surgery appear to adhere to a bimodal distribution of very low and very high levels of impairment (Figure 1c). It is possible that this is because patients whose functional level classifies as GMFCS III generally have a predominantly diplegic lower limb involvement. The GMFCS levels of the register population can be seen in Figure 4 for comparison of distribution. Of note, bimodality does not feature. High level of motor impairment is believed to reduce the likelihood of improved surgical outcomes.6,7,11,18,24,29,32–35 However, surgical outcomes can vary drastically depending on the individual’s particular goals of intervention. This can be seen in the paper by Gong and colleagues, where the cohort was split into high and low levels of physical function.33 Better results of activity and participation were achieved for the high-functioning group, and better results regarding hygiene were achieved in the low-functioning group.
It is difficult to extrapolate any trends regarding MACS levels. Seventy five per cent of individuals did not have a MACS level recorded (Figure 1d). The MACS is currently the most widely accepted method of describing and classifying upper limb function in CP, so it is interesting to see very low uptake in its clinical use. The variable quality of GMFCS and MACS recording reduces the ability to compare data across individuals of differing ability and across studies. Further investigation into why the GMFCS and the MACS are unreliably used is warranted. Improved clinical use may assist improvements in translatability of data across studies in the future.
The way motor type was recorded in this study differs from that of the register. As previously discussed, motor type predominance was not able to be captured in this study. However, comparison with the register can be performed if only the population who are solely spastic, solely dyskinetic (dystonic and athetoid/choreoathetoid) or mixed spastic and dyskinetic is considered. The register revealed that 82 per cent of individuals are solely spastic, 14 per cent are mixed spastic and dyskinetic and 4 per cent are solely dyskinetic. The study revealed that 65.3 per cent of individuals are solely spastic, 31.6 per cent are mixed spastic and dyskinetic, 3.1 per cent are solely dystonic. The rate of pure spasticity observed in the study is 16.7 per cent lower than that of the register. However, the percentage of individuals with a spastic component to their motor impairment is identical. It is possible that the population who have a mixed motor type is artificially overrepresented in this study due to differing thresholds of inclusion of dystonic features. Dyskinesia is considered as a feature that would increase caution when considering operative intervention due to the risk of producing posturing that an individual may find more difficult to control.5,21,34,36 As such, it is interesting to see that rates of mixed motor impairment in this study are much higher than that recorded in the general population with CP.
Cognitive impairment is believed to be a predictor of poorer surgical outcomes.7,11,13,24,30,34 Some 60.8 per cent of surgical candidates had impaired cognition, while 18.6 per cent had an unknown level of impairment. These figures cannot be compared with the register due to differing criteria used. Two features of the surgical cohort are of note here. Firstly, cognition is often not formally assessed or recorded. Secondly, individuals with cognitive impairment make up the majority of surgical candidates. While adequate cognition is helpful when embarking on a comprehensive rehabilitation program involving functional tasks and goals, it is of reduced importance for those who are more severely functionally impaired and where the goals are to improve the caregiver’s ability to perform dressing and hygiene related tasks. The rehabilitation of this latter cohort more frequently centres around more passive interventions such as serial splinting, requiring lower levels of patient cooperation. When goal setting for an intervention such as surgery, one should ideally consider all aspects of the ICF model. The Cerebral Palsy Quality of Life (CPQoL) questionnaire effectively achieves this; however, it was used in only one individual’s postoperative assessment.
Upper limb sensation was recorded for only eight individuals, whereby it was recorded as impaired each time. Sensation as a determinant of surgical outcome is contentious in the literature. Poor stereognosis is sometimes noted to perhaps negatively influence outcomes due to sensory neglect, but it is mostly believed not to be a contraindication to surgical intervention.5–7,23,34 The literature review by van Munster and colleagues did not support a poorer outcome with increased sensory impairment. This may explain the lack of use of this measure in the cohort.37
Many types of surgical procedures were performed on the individuals in this study. Each surgical plan was tailored to the individual due to the diverse effects of spasticity on the structures of the upper limb, the differing environmental factors that influence each individual’s ability, the varying levels of desired participation and the diversity of goals seen in the cohort. The ICF model highlights the variety of influences that affect decision- making in each individual case. These operative plans appear to be made using highly variable preoperative data along with the personal clinical experience of the surgeon.
It is common for an individual to undergo multiple surgical events for the upper limb during their lifetime. Within the 10-year time period at the RCH 74 individuals had one surgical event, 21 had two and seven had three or more. However, many of these individuals had additional surgeries either outside the 10-year time frame or at a hospital other than the RCH. The multiple surgeries may reflect the quantity of changes required to alter the impaired limb/s, the child’s anatomical changes through growth, changing motor type such as increasing dystonia with age, and/or the differing needs and environment of the child over time.
Objective outcome measures were used for the majority of individuals. They were performed preoperatively 69.6 per cent of the time and postoperatively 73.2 per cent. Unfortunately, the outcome measures used varied markedly in type and reliability. Range of movement was by far the most used. Of those who had outcome measures performed, 90.6 per cent had ROM measured preoperatively and 90.1 per cent had ROM measured postoperatively. Of note, in this study ROM was recorded as having been performed if there was a numerical value noted for any movement of the upper limb. There were many circumstances where only one range of movement was performed for the whole upper limb ROM assessment. The minority had full ROM records for multiple levels of the upper limb. The methods of obtaining ROM also varied in reliability. Some were visually estimated and others were measured using a goniometer. The majority did not report method of attainment.
The second most popular method of measuring outcomes was to record one or more selected activities of daily living that the individual had difficulty completing. This was used in more than 30 per cent of pre- and postoperative measures. A shortfall of this method is that the level of ability or difficulty in completing the task was often not recorded, only that difficulty existed. This reduces sensitivity for change. The Canadian Occupational Performance Measure (COPM) and Goal Attainment Scaling (GAS) are valid and reliable outcome measures that use an objective numerical scale to record task competency and performance satisfaction in a range of patient-specific tasks.38 Unfortunately, GAS was not used at all in this cohort and COPM only made a small (7.3–8.9%) of the outcome measures recorded pre- and postoperatively, respectively. The Canadian Occupational Performance Measure is a quick, easy tool to use and lends itself well to the types of task-oriented details already sought pre- and postoperatively. Standardising the recording of task-oriented measures would greatly assist in objectifying outcomes that are already being collected from individuals undergoing operative care.
Other measures that were less frequently used included individualised video recordings of selected tasks, the Melbourne Assessment, dynamometer pinch and grip strength testing, manual muscle testing, the handwriting speed test, the CPQoL questionnaire and the Paediatric Quality of Life Inventory (PQoL-I) (Table 2). Individuals rarely had pre- and/or postoperative assessment that considered all aspects of the ICF model of impact.
There are currently many valid and reliable outcome measures that are used for assessment of CP and that capture many domains of disability impact.38 Implementing the use of a standardised collection of valid, reliable and easy-to-use measures would reduce unnecessary diversity in the quantity and quality of patient assessment. The study results suggest that there is a need to increase uniformity in perioperative assessment of individuals with CP undergoing upper limb surgery to better assist in determining outcomes within future research.
A deficit exists in the literature regarding patient/caregiver satisfaction post-surgery.34 This is supported by the infrequent recording of postoperative satisfaction in this study. Satisfaction was not recorded in 68.8 per cent of cases. Of those responses that were recorded, 93.0 per cent were satisfied. It can be hypothesised that perhaps clinicians are generally less willing to record patient dissatisfaction. Johnstone and colleagues have produced one of the few papers where satisfaction of all patients and/or caregivers was objectively recorded postoperatively. They showed that 85.4 per cent of patients and/or caregivers were satisfied.34 It is unclear why collection of data regarding overall satisfaction is so rarely performed in this setting considering that the intervention involves elective surgery for a permanent disability with a complex functional impact.
Conclusion
Currently, it seems individuals are selected for surgery using preoperative assessment that is highly variable in quantity and quality with little to no elements of standardisation across individuals. This results in inhibition of research progress and poor understanding of this population and their surgical outcomes. According to the literature, surgery continues to be an effective intervention for improving function, hygiene and cosmesis of the upper limb for individuals with spastic CP. Results can be variable and currently no clear evidence-based guidelines exist to assist with identifying candidate characteristics that are more likely to result in a better surgical outcome.
Surgical selection is determined by broadly observed and variable parameters that have great potential to differ between clinicians. These compounding issues provide rationale for initiating further research into the characteristics of this patient group. It suggests a requirement for routine use of valid, reliable and easy-to-use standardised outcome measures for perioperative assessment, including follow-up regarding function and patient satisfaction. Only then can meaningful data be achievable to better explore how individual characteristics influence the outcomes of surgery and to better assist this population in receiving recommendations and prognoses with improved confidence and reliability.
Acknowledgements
Thank you to Sarah Knight and the Victorian Paediatric Rehabilitation Service team at the Royal Children’s Hospital, Melbourne for their support throughout the conception and execution of this project. We would also like to thank Chris Coombs, Damon Thomas and Sian Fairbank from the Department of Plastic and Maxillofacial Surgery for their contribution to the project’s design and identification of relevant data. Finally, thank you to Marg Costa and Allison Lusher for their invaluable assistance with data capture.
Patient consent
Patients/guardians have given informed consent to the publication of images and/or data.
Conflict of interest
The authors have no conflicts of interest to disclose.
Funding declaration
The authors received no financial support for the research, authorship, and/or publication of this article.