Introduction
Orofacial cleft occurs when embryonic facial processes fail to fuse during development. Cleft palate and cleft lip (with or without cleft palate) have been reported in approximately one in every 700 live births worldwide.1 However, a recent study conducted in New Zealand found the incidence of orofacial cleft to be slightly higher at one in 559 live births.2
Orofacial clefts have a wide range of severity and can create functional and aesthetic issues for the affected individuals. As a result, children with cleft require coordinated interdisciplinary care including surgical and non-surgical interventions that can extend from birth to early adulthood. This treatment is provided by a wide range of health professionals with the goal to establish as near normal functional and aesthetic outcomes as possible. However, it is evident in the literature that often functional and aesthetic challenges faced by children with cleft can have a significant influence on their social interactions and general happiness.3–5 Although there has been an emphasis on assessing various clinical outcome measures in cleft care, more recently patient-reported outcome measures (PROMS) have been given a high priority.6
The Christchurch Cleft Clinic (clinic) was established in the 1960s and is a multidisciplinary clinic for children with orofacial clefts involving specialist input from plastic, otolaryngologist and oral and maxillofacial surgeons as well as orthodontists, speech language therapists and paediatric dentists. Similar to other cleft clinics internationally, the concept of the clinic is based on a holistic assessment of each patient’s needs, resulting in cohesive interdisciplinary decision making and treatment planning.
Over three years from 2016 to 2019, each attending caregiver at the clinic was asked to complete a paper-based survey prior to their child’s appointment. This survey was used by cleft team clinicians to determine the primary areas of concern and to ensure that any issues are addressed during the cleft outpatient visit. In addition to the common functional and aesthetic issues affecting patients with cleft, questions regarding social interactions and general happiness were surveyed to improve understanding of the influence of orofacial cleft on wellbeing.
The aim of this research was to investigate how parents/caregivers score functional and aesthetic aspects of their child’s cleft as well as their child’s overall social interactions and happiness. This research was conducted to enable improvement to cleft clinic services if indicated.
Methods
A dataset from the clinic records was retrospectively accessed for those attending the monthly cleft outpatient clinic from February 2016 to March 2019. The survey was developed primarily as a communication aid between parents and cleft team professionals and was focused on similar key areas of concern that were advocated by the Cleft Hearing Appearance and Speech Questionnaire (CHASQ) that was being developed at that time.
Survey forms from parents/caregivers that had been uploaded to their child’s electronic clinical notes were included in this study. If there were repeat surveys, only one form was used for each child (the most recent form) and only fully completed forms were included. Survey forms were excluded if the child was older than 17 years, had a noted syndrome or did not have an orofacial cleft.
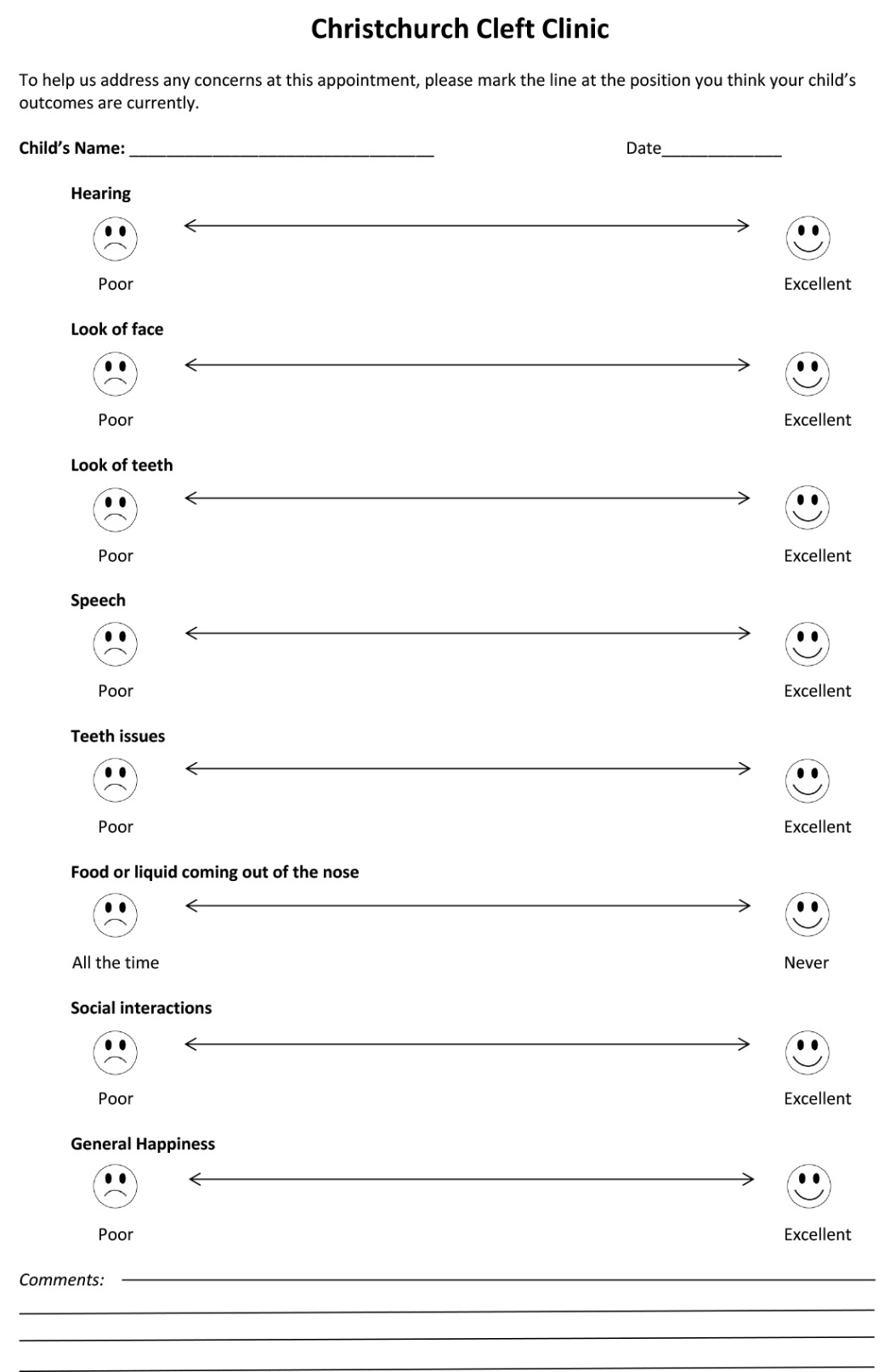
This research was a mixed-methods study involving both quantitative and qualitative analysis of the paper-based survey used in the clinic. The survey comprised eight items—hearing, look of face, look of teeth, speech, teeth issues, food or liquid coming out of the nose, social interactions and general happiness. The items were scored using a 100 mm visual analogue scale (VAS) that was rated from poor (0 mm) to excellent (100 mm). Additionally, the survey included a free-text comment section so that additional information, concerns and questions could be added by the attending parent/caregiver (Figure 1).
De-identified demographic and clinical data for each patient were entered into a Microsoft® Excel® (version 2007, Microsoft Corporation, North Ryde, NSW, 2113, Australia) spreadsheet. A score for each item was determined by manually measuring the distance of the mark along the scale. Descriptive statistics were conducted on the data using STATA® statistical software (StataCorp LLC, College Station,Texas, United States of America). To determine the re-test reliability of the VAS, a sub-sample of 15 attending parents/caregivers was asked to score two surveys approximately 30 minutes apart. Spearman’s correlation demonstrated adequate re-test reliability (0.86).
Qualitative analysis of survey free-text comments was conducted via thematic categorisation as per Maykut and Morehouse, and Pope and colleagues.7,8 Three researchers (ZB, MS, PF) independently conducted analysis and predominant themes were identified after consensus with the research group.
The study was deemed an out-of-scope audit from the New Zealand Health and Disability Ethics Committee; locality approval was granted by the Canterbury District Health Board [RO# 19069] and consent was obtained from all participants.
Results
A total of 226 surveys from 154 parents/caregivers were collected for this study representing approximately 50 per cent of possible clinic attendees. Surveys with incomplete questions (24) and/or that had repeat submissions (72) due to multiple clinic attendances over the study’s duration were excluded from further analysis. This reduced the sample to 130 surveys with a mean child age of 8.04 years (95% CI: 7.29–8.78) and 54 per cent were male. New Zealand European was the most common ethnic group within this study, followed by Māori. Overall, the ethnic distribution in this study was similar to that of the wider New Zealand population based on census information (Table 1).9
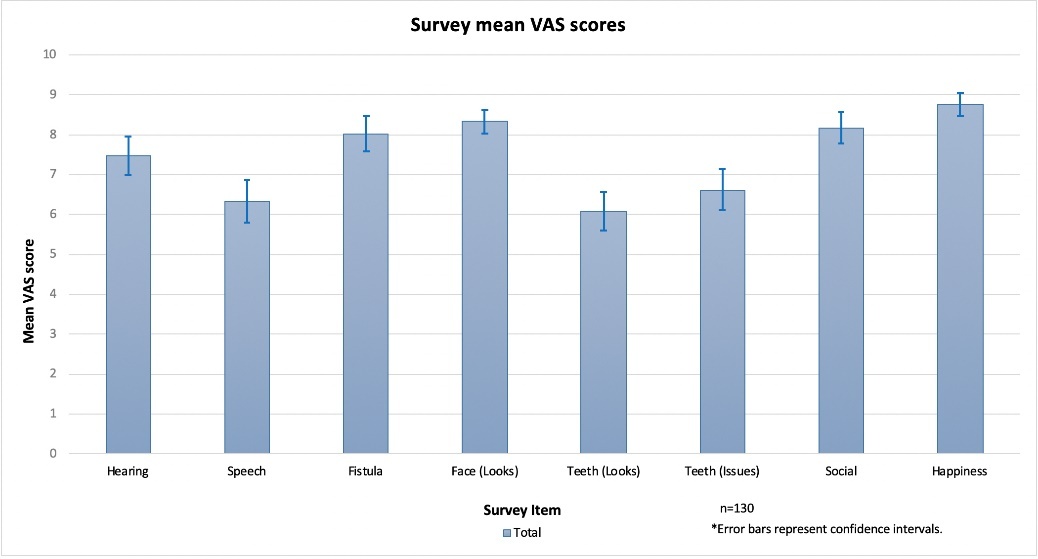
The mean VAS for each of the eight items was calculated (Figure 2). Speech, teeth issues and look of teeth had lower mean scores, which represent a higher degree of parent/caregiver concern. Food or liquid coming out of the nose (that is, fistula) and hearing were additional key issues of concern. There were significant differences (ANOVA, Scheffe post-hoc test) between cleft type (CL = cleft lip, CLP = cleft lip and palate, CP = cleft palate) for hearing (p = 0.033, CP < CL), look of face (p = 0.003, CLP < CP) and fistula (p < 0.001, CLP < CL). Speech, look of teeth, teeth issues, social interactions and general happiness did not have significant differences between cleft type.
Qualitative data of 107 free-text parent/caregiver comments was assessed by thematic categorisation (Table 2). Most comments involved negative functional issues (n = 58), with speech being the most common concern (n = 28), and fistula (n = 16) and dental concerns (n = 14) also recorded.
Discussion
Speech was a common area of parent/caregiver concern in this study in both the qualitative and quantitative assessments. Hearing, look of face and food or liquid coming out of the nose (fistula) differed by cleft type in the expected clinical direction.10–12
Our study did, however, have several limitations. These include the lack of a non-cleft control group, the lack of validation of the items used within our survey (which prevented us from performing linear regression analysis) and the absence of clinical-based outcome measures.13 Despite this, self-reported ratings of common cleft-related items associated with function and aesthetics could be considered valuable as these reflect everyday experiences for that individual.
Visual analogue scale has been shown to have satisfactory reproducibility and correlates well with health-related measures similar to those used in our study for children with orofacial cleft.14,15 Additional strengths of this study were the ability to analyse both quantitative and qualitative aspects of parent/caregiver concerns and the sample size, although an improved responder rate would have benefited the study.
The relatively low scoring for speech and the number of concerns raised in the parent/caregiver free-text comments relating to speech were important findings of this study. Access for advanced hospital-based speech assessments and surgical intervention are generally unrestricted and dealt with on an as-needed basis. Although similar findings related to speech were noted in other international studies,3,16,17 the findings of this study may reflect the perceived under-resourcing of speech language therapy, which has been an ongoing concern raised by the New Zealand Cleft Support Group.18 In New Zealand there is no priority given for children with cleft to access ongoing speech therapy within the community where speech therapy is funded by the Ministry of Education. Although short, intensive hospital-based speech therapy can be provided by the Ministry of Health via the respective district health boards, there are constraints in the provision of this care.
In our study, teeth issues and look of teeth both received relatively low mean item scores. Teeth issues scoring may be related in part to the fact that New Zealand children with cleft have poorer dental health status than general population-based data at age five years.19 It should also be noted that although a small proportion (14.3%) in a study of UK children with cleft were reported to be dissatisfied with the looks of their teeth,4 parents/ caregivers tend to rate the aesthetic concerns of their child’s teeth as more severe than the child themselves.20 It was interesting to note that our qualitative findings also suggest that dental issues are of particular concern to parents.
The literature supports the concept that social interaction and general happiness of children with cleft are strongly associated.21–23 It is important to note, however, that any association between social interaction and general happiness is complex and further research is required to understand the individual factors that contribute to these surrogate markers of wellbeing.23 Antia and colleagues found that although children who are deaf or have hearing impairments tend to initiate social interactions at a similar frequency to children with no hearing impairment, they are less likely to thrive in these interactions. It was also found to be more challenging for these children to maintain interactions, as hearing is required to reciprocate in most social circumstances.24 Recently an otolaryngologist surgeon has joined the clinic team, and this specialist input will hopefully help address concerns related to hearing.
Previous research has also reported that patients with cleft are negatively evaluated based on their appearance.25 Consequently, clefts that are visible extra-orally are likely to impact on social interactions. Tobiasen and Hiebert assessed the response of children and young adults when looking at photographs of cleft lip and palate patients. They found that faces with more severe cleft impairments were seen as being less socially desirable than faces with moderate impairments.25 Similarly, another study by Shaw had participants rate photographs of patients with normal incisors, cleft lip, crowded incisors, absent lateral incisors and prominent incisors. They reported that participants rated those with an aesthetic dental and facial appearance as more socially desirable, more intellectual and less likely to exhibit aggressive behaviour.26
It is clear when evaluating the literature that patients with orofacial cleft face social and emotional challenges related to their condition. One study reported 25 per cent of children with cleft indicated that they had been teased about their cleft and over half conveyed that their confidence and ability to find a partner had been impacted.4 However, the psychosocial impact of cleft lip and palate on an individual is difficult to assess given its complexity and variation among studies. Although specific difficulties with anxiety, depression, behavioural problems and dissatisfaction with facial appearance have been reported in the literature,27 there is currently limited psychological support available upon referral from the clinic team. The inclusion of a psychologist in the team (a recommendation from the American Cleft Palate-Craniofacial Association Team Accreditation Standards) could better equip those children who have difficulties coping with these challenges.28
The generalisability of the study’s findings may be limited as the sample patients were all treated in a single cleft centre. Further investigations extending to other cleft centres using similar surveys of parent/caregiver concerns of children with cleft would be advantageous, particularly within New Zealand, as the findings may help drive improved service outcomes at a national level.
Conclusion
This study found that speech was a common functional concern for parents/caregivers of children with cleft attending the Christchurch Cleft Clinic, along with the look of teeth and teeth issues. The findings support the need for interdisciplinary care, where speech language therapy should be well resourced as a key focus in cleft services along with dental services. Cleft care healthcare providers should also consider active otolaryngology and psychology input to ameliorate issues that arise for children with cleft.
Patient consent
Patients/guardians have given informed consent to the publication of images and/or data.
Conflict of interest
The authors have no conflicts of interest to disclose.
Funding declaration
The authors received no financial support for the research, authorship, and/or publication of this article.
Revised: June 24, 2020 AEST