Introduction
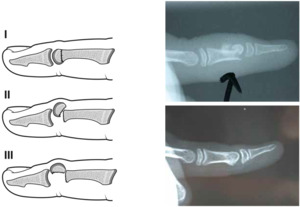
Subcapital phalangeal fractures occur primarily in children. Al-Qattan classified these into three types based on the degree of displacement1: type I (20%) is undisplaced; type II, the most common (70%), has dorsal displacement and rotation of the phalangeal head with bony contact to the proximal fragment; and the type III (10%) has a displaced fragment without bony contact to the shaft. Without intervention, type III fractures proceed to non-union. Type II fractures also present a challenge as they often proceed rapidly to malunion with the consequence of joint stiffness because of impingement of the distal phalanx upon the prominent volar edge of the proximal fragment of the phalanx. In cases of delayed presentation of type II fractures, osteotomy has been encouraged, though this can be challenging given the small size of the head fragment.2 An alternative for an established malunited type II fracture is an ostectomy of the volar edge of the phalangeal shaft to clear the subcondylar fossa.
In the growing hand in particular, the deformity of a malunited fracture has the potential to remodel according to Wolff’s law where physiological loading influences bone deposition and resorption to adapt the bone conformation to resist that load.3 Remodelling a displaced fracture depends on the magnitude and direction of the deformity, its distance from the physis and the amount of remaining skeletal growth. Circumstances where significant remodelling will not occur, and malalignment will persist, include significant intra-articular incongruity, rotational deformity and angular deformity in the radio-ulnar plane. In a typical subcapital phalangeal fracture, the deformity is in the dorsal-volar plane which is favourable for remodeling as it is in the plane of motion and there have been reports of isolated examples of radiographic remodelling and good clinical results treating displaced subacute subcapital phalangeal fractures non-operatively.4–8 The concern is, however, that the typical deformity of this fracture type is remote from the physis and therefore potentially less likely to remodel, resulting in a poor prognosis if not corrected.9 The purpose of this case series is to characterise outcomes among early malunions of subcapital phalangeal fractures that are treated conservatively.
Case series
We reviewed our experience with non-operative management of subcapital phalangeal fractures with early malunions from 2005 to 2015. We identified six patients, (age range four to 10 years). All were little finger injuries. One fracture was of the middle phalanx, the others were of the proximal phalanx. Patients presented two to six weeks post injury. Follow-up ranged from nine months to four years. All patients showed radiographic evidence of remodeling in the dorso-volar plane, with elimination of the prominence of the volar edge of the proximal phalangeal fragment and regained mobility at the affected joint (Figure 1). No patients in the series required osteotomy for residual deformity.
Discussion
Matzon and colleagues reported an algorithm for the treatment of displaced paediatric phalangeal neck fractures.10 Within their stepped framework, fractures are classified as acute, early healing/incipient malunion or healed, each having implications for non-operative treatment, treatment with closed/percutaneous/open reduction and pinning or salvage procedure.10
Non-operative treatment for malunited subcapital fractures was initially discredited due to the presumption that fractures remote from the phalanx physis have poor potential for remodelling.9 However, several case reports have supported skeletal remodeling of dorso-volar plane deformity in subcapital phalangeal fractures.4–8 Conversely, when rotational deformity or radio-ulnar angulation are present, there is not data to support potential for significant skeletal remodelling.7 In this situation, percutaneous osteoclasis and pinning lowers the risk of avascular necrosis compared to open reduction and pinning and has been successful up to 36 days post injury.2,10
Cornwall and colleagues reviewed phalangeal neck malunions and emphasised that, while reducing and fixing the fracture provides the best chance of re-establishing normal joint motion in a timely manner, in the type II group with incipient or established malunions in the dorso-volar plane, surgery should not be considered mandatory.4 The authors outline their criteria for non-operative management: no rotational or radio-ulnar plane malalignment, the adjacent interphalangeal joint is congruent, bony union of the fracture is achieved, significant growth potential exists, family and patient can tolerate the limitation of joint motion during remodelling and are willing to be patient.4
Conclusion
In our practice, undisplaced type I fractures are treated with a splint and closely monitored to ensure there is no late displacement. Where acute, type II and III fractures undergo closed reduction and pinning. Type III fractures that are unable to be reduced closed may need to be opened to allow direct manipulation of the fragment and stabilisation. Patients with type II fractures with typical dorsal angulation deformity are now treated conservatively and allowed to remodel, avoiding the risks of devascularising or fragmenting the phalangeal head fragment with osteotomy and pinning.
Patient consent
Patients/guardians have given informed consent to the publication of images and/or data.
Disclosures
The authors have no conflicts of interest to disclose.
Funding
The authors received no financial support for the research, authorship and/or publication of this article.
Revised: September 3, 2019 AEST