Introduction
The development of the surgical microscope and the advent of microsurgical techniques have been milestones in plastic and reconstructive surgery. As a result, surgeons have been able to unlock the highest rungs on the reconstructive ladder1 and consolidate the role of free-tissue transfer as a key tool in complex reconstructions. The field continues to grow as surgeons push boundaries and attempt to handle small vessels previously thought to be inaccessible, such as in the field of supermicrosurgery.2 Microsurgery is now embedded in the armamentarium of the modern plastic surgeon, with trainees expected to be proficient at techniques such as microvascular anastomoses and nerve coaptations by the conclusion of their training.
With the increasing number of applications for the microscope, junior doctors are seeking competency in microsurgical skills at an earlier stage of their training. While the volume of operative cases remains key to one’s mastery, live surgery may not be the most appropriate setting to impart basic instrument and tissue-handling skills, due to factors including time pressures and the high-stakes nature of revascularisation/replantation surgery. Safe and supportive training environments are required to help establish the manual dexterity, three-dimensional visualisation and mental fortitude required. To meet this demand, training courses outside of the normal curricula have emerged as platforms for trainees to receive exposure and attain elementary microsurgical skills. Anecdotally, significant numbers of Australian trainees have ventured overseas to partake in these training courses. The aim of this study is to assess demand for an Australia-based microsurgery training course (MTC).
Methods
For the study an online-based survey was sent to current Australian plastic surgery trainees through the Australian Society of Plastic Surgeons. These included surgical education and training (SET) registrars accredited by the Royal Australasian College of Surgeons, unaccredited/service registrars and hospital medical officers (HMOs). The survey, consisting of 10 questions, was developed by the authors and generated on the SurveyMonkey (SurveyMonkey Inc, San Mateo, California, USA) platform. Responses were kept anonymous and collected from May to June 2019.
Respondents were asked to describe their experiences with MTCs, including location, course satisfaction and whether they felt there was a need for more Australia-based courses. Results were analysed using descriptive statistics.
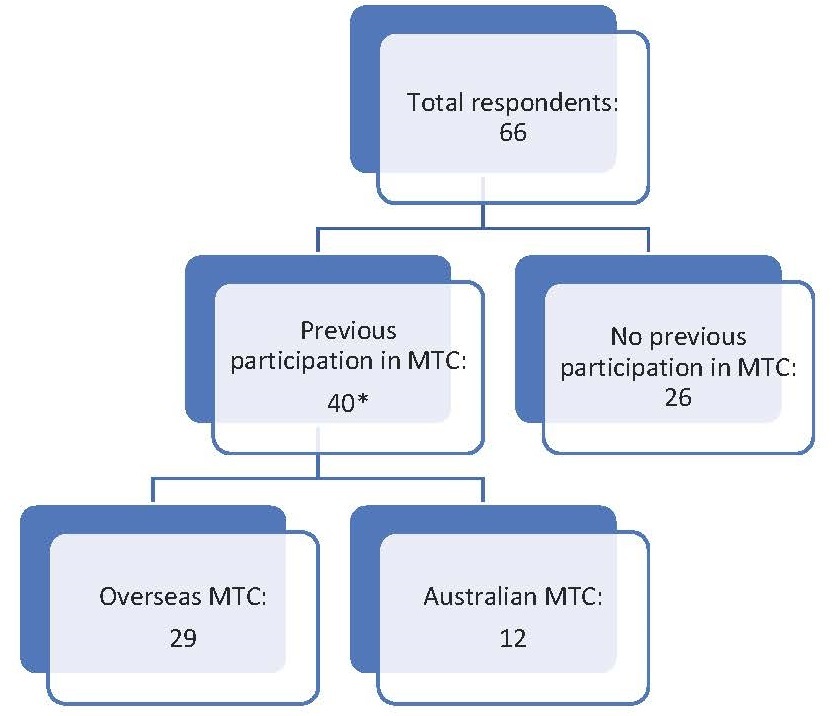
A total of 66 responses were collected, with 63 (95%) respondents being SET or unaccredited plastic surgery registrars and the remaining three (5%) being HMOs. Of the respondents, 40 (61%) had participated in MTCs—28 (70%) had participated at an overseas facility, 11 (27.5%) had participated in Australia and one (2.5%) had participated in both overseas and local courses (Figure 1 and Table 1).
The majority of those who had travelled abroad enrolled in MTCs organised by Columbia University (USA), National University Hospital (Singapore) or Ganga Hospital (India). When asked why they had travelled overseas (with more than one answer allowed to be given), 23 (79%) stated that this was due to a lack of local options, 19 (66%) for the reputation of the course and 14 (48%) for the opportunity to travel. Of those who had participated in Australian MTCs, seven (58%) had done so in Sydney, three (25%) in Adelaide and two (17%) in Perth. Regardless of where they had undertaken their course, all participants stated that they found it useful in their clinical practice.
Finally, the respondents were asked about the utility of MTCs in their training: 55 (87%) believed that independent courses were an important part of training and 56 (85%) believed that there was a need for more courses in Australia.
Discussion
Australia has played a significant role in the development of microsurgery and its expansion into plastic and reconstructive surgery. Daniel and Taylor from the Royal Melbourne Hospital reported one of the earliest free cutaneous flap transfers in 1973,3 and the latter subsequently published the first case report of free fibula transfer in 1975.4 The O’Brien Institute, formerly known as the Microsurgery Research Centre, was established in Melbourne in the 1970s and was at the global forefront of microsurgery education and research. Given a history so richly steeped with milestones and pioneers of microsurgery, it is striking that 44 per cent of trainees who responded to the survey had gone overseas to seek initiation in the field, with the majority stating that a lack of local options was a reason why they did so.
In order to quantify the local training options available, an online Google search was conducted of MTCs available in Australia. This yielded four positive results—one each in New South Wales (part of a postgraduate degree) and South Australia (deferred indefinitely) and two in Western Australia (Table 2). Notably, none were available for registration as standalone courses as of December 2019, and the sole actively running program was offered only to postgraduate students at the University of Sydney. Apart from the paucity of options, there also appeared to be significant variation in the structure and content, with duration ranging from one to nine days and practice models comprising an array of live animal, cadaveric animal and artificial models.
Given the current landscape, we believe that there is demand for an Australian-based MTC. Ideally, it would be targeted at residents and service/unaccredited registrars who have little to no experience under the microscope, with the following objectives:
-
understand the principles of microsurgery and its role
-
develop familiarity with microsurgical instruments and soft-tissue handling
-
learn and perform microsurgical knot-tying
-
practise knot-tying and luminal anastomoses on models (animal or artificial).
It stands to reason that once a regular, well-subscribed MTC has been established, the next step would be to institute a permanent microsurgery training laboratory that is easily accessible to trainees.
Conclusion
MTCs are a valuable extracurricular resource for plastic surgery trainees. A current lack of local options has seen many trainees travel abroad to seek training, and we recommend establishing an Australia-based course to meet this demand.
Disclosure
The authors have no conflicts of interest to disclose.
Funding
The authors received no financial support for the research, authorship and/or publication of this article.
Revised: February 24, 2020 AEST