Introduction
The New Zealand (NZ) population has grown more rapidly than forecast by Statistics New Zealand/Tatauranga Aotearoa at the time of the last plastic and reconstructive surgery (PRS) workforce study in 2013.1–3 Previous population forecasts predicted that the population would exceed five million by 2027.3 Updated modelling from the 2013 census, which includes more accurate net migration data and data from the 2018 census, shows that this number was surpassed in 2020.2,4 In 2013, an NZ PRS workforce analysis identified six service centres providing public PRS services but that the plastic and reconstructive surgeon (PRSn) to population ratio (PRSPR) in NZ was lower than in Australia, the USA and other comparable countries.3 A recommendation was made to increase the PRSPR to the level of comparable countries and to address the maldistribution of PRSn by increasing the number of centres offering public PRS services nationwide. A total of 12 service centres with a minimum of three PRSn per centre was proposed, to ensure equitable access to public PRS services for all New Zealanders.3 This follow-up analysis provides an update on the current PRS workforce in NZ.
Methods
The population data and projections from Statistics NZ were collected including sub-analyses of the 2013 census and the 2018 census. The number of current practising PRSn was obtained from the Medical Council of New Zealand online registry and cross-checked against the District Health Board (DHB) PRS service centres’ consultant positions and full-time equivalents (FTEs). Data were collected on regional population numbers in 2019 and forecast populations in 2028 and 2033. The PRSPR was calculated using the sub-national population data for each DHB and the absolute number of PRSn within the catchment area. Areas underserviced and with unmet needs were identified. Two models of an ideal PRSPR—a minimal acceptable ratio of 1:80,000 or ideally 1:60,000—were used to calculate regional workforce needs. NZ PRS trainee numbers between 2004 and 2020 were obtained from the Royal Australasian College of Surgeons (RACS) along with FRACS pass rates and annual graduation rates, which were used to model local workforce supply.
Results
The number of practising PRSn in NZ increased from 57 in 2013 to 72 in 2019. Over the same period, the NZ population increased from 4,442,100 to 4,917,000.5 As a result, the PRSPR improved from approximately 1:78,000 to 1:69,000.
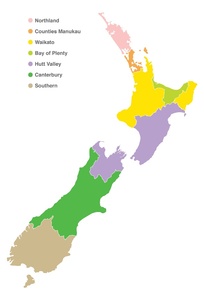
Seven DHBs currently provide onsite public PRS services to their own population. Of these, four regional PRS service centres are based in Counties Manukau, Waikato, Hutt Valley and Canterbury DHBs, and three smaller PRS service centres are based in Northland, Bay of Plenty and Southern DHBs, the latter added since the last PRS workforce review. In addition to providing PRS services to their own region, the three centres based in Counties Manukau, Waikato and Canterbury DHBs also provide tertiary and variable amounts of acute PRS services to Northland, Bay of Plenty and Southern DHBs, respectively. Figure 1 illustrates the geographical catchment for these public PRS service centres.
The population size, the total number of PRSn and the PRSPR for each region, along with the number of PRSn employed, the FTEs and the number of FTEs per 100,000 population served by each public PRS service centre in 2019 are presented in Table 1. Of the 72 PRSn in NZ, 59 were employed for a total of 49.49 FTEs by the public PRS service centres. The Counties Manukau DHB catchment currently has a PRSPR of 1:51,000. Northland has the largest unmet need with a PRSPR of 1:189,000 and would require 1.4 more PRSn to achieve a minimal acceptable PRSPR of 1:80,000. The region served by Hutt Valley public PRS service centre should ideally have a 1:60,000 PRSPR given it is a tertiary referral centre; an additional 5.5 PRSn would be required to achieve this.
Table 2 presents the net increase in PRSn per region by 2028 and by 2033 if the ideal PRSPR of 1:60,000 were to be achieved. In this scenario, by 2033 Northland would have the largest growth (220%), followed by Bay of Plenty (124%), then Waikato, Southern and Hutt Valley (all approximately 45%), Canterbury (14%) and Counties Manukau (10%). The largest increase in the absolute number of PRSn needed between 2019 and 2033 would be in Hutt Valley (5.8) and Waikato (4.2).
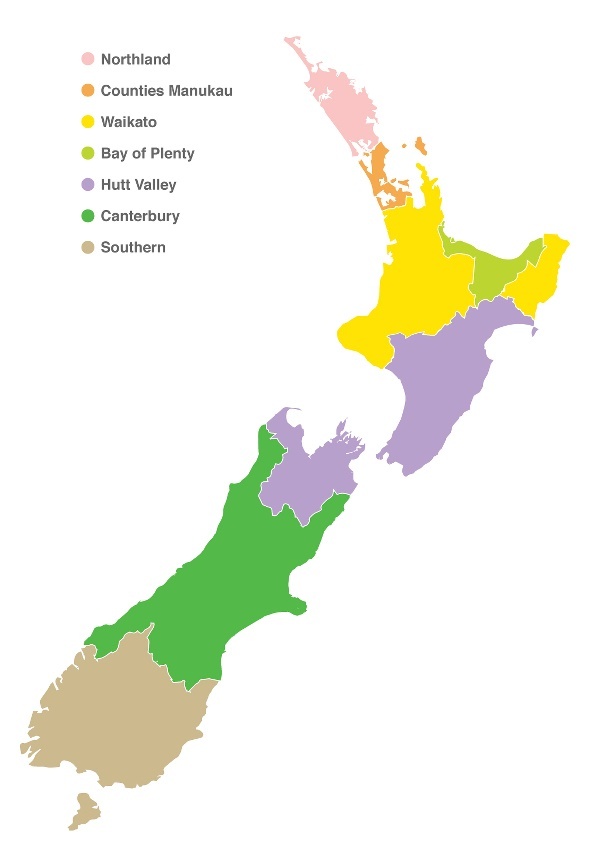
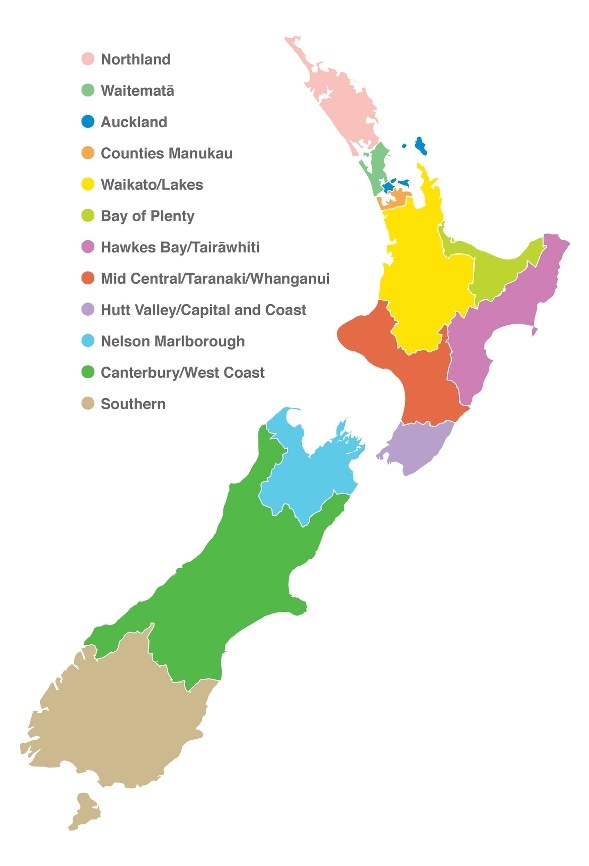
In 2013, an additional five public PRS service centres were proposed nationwide in order to improve equity of access to public PRS services and to correct the vast maldistribution of PRSn among the NZ population. Furthermore, it was proposed that the Counties Manukau regional centre be subdivided into three service centres including Auckland and Waitematā, and the Hutt Valley regional centre be subdivided into four service centres including Hawke’s Bay/Tairāwhiti, Mid Central/Taranaki/Whanganui and Nelson Marlborough, as illustrated in Figure 2. Table 3 presents these 12 public PRS service centres named by DHB, or combination of DHBs, with up-to-date population projections and ideal PRSPRs in 2028.
In this model, the Counties Manukau PRS service centre would undergo the most significant change. After subdividing, the Auckland PRS service centre would require 10 PRSn, and the Waitematā centre would require 12 PRSn. The need within the Counties Manukau PRS service centre would decrease to 10 PRSn on a population equity basis. The proposed extended Mid Central PRS service centre, which would also provide services to Whanganui and Taranaki, would need more than six PRSn. At least four of these PRSn could be redistributed from the Hutt Valley/Capital and Coast PRS service centre. The Nelson Marlborough and Hawke’s Bay PRS service centre would need three or more PRSn to reach both an ideal PRSPR and to provide a practical roster to allow local provision of acute services. Both the Northland and the Bay of Plenty PRS service centres would require two additional PRSn within this nine-year period. The Canterbury/West Coast and the Southern PRS service centres would require at least one further PRSn each, and the Waikato/Lakes PRS service centre would require less than one PRSn, as long as the Bay of Plenty and Taranaki DHBs were appropriately resourced.
Four of the current seven public PRS service centres are accredited to provide training for PRS registrars through the RACS with a duration of training of five years. The total number of PRS trainees has increased from 14 in 2009 to 17 currently, nationwide. PRS graduation rates have remained relatively static, with three trainees passing their final exams and a similar number initiating training each year, since 2012. Therefore, over the next nine years until 2028 an additional 27 NZ-trained PRSn are expected to join the PRS workforce—ten more PRSn than our model forecasts are needed by 2028.
Discussion
The current number of PRSn in NZ has improved since 2011, resulting in a PRSPR of 1:69,000 which is comparable with the PRSPR in Australia. According to the RACS, Australia currently has 360 registered PRSn6 for a population of over 25 million,7 giving a PRSPR of 1:70,000. The USA has a higher PRSPR of 1:50,000.8 However, despite an improvement in the overall workforce, the vast maldistribution of PRSn in NZ remains largely unchanged.
Currently, public PRS services are provided from the seven PRS service centres comprising four regional service centres and three smaller centres. In addition to providing PRS services to their own region, the regional PRS services based at Counties Manukau, Waikato and Canterbury DHBs also provide tertiary and variable amounts of acute PRS services to Northland, Bay of Plenty and Southern DHBs, respectively. DHBs that do not directly employ PRSn receive some consulting and/or operating PRS services from partner DHBs. These include visiting services to the following hospitals: North Shore, Auckland City, Starship Children’s, Taranaki, Gisborne, Rotorua, Hawke’s Bay, Palmerston North, Whanganui, Nelson, Blenheim, Timaru and Greymouth. Some of these hospitals are up to 370 km from their nearest PRS service centres. For example, the Gisborne Hospital outpatient clinic is staffed by Waikato-based PRSn. Services provided vary from clinics to visiting operating services but are not supported by resident PRSn in those centres. For more urgent treatment and more complex procedures, and for inpatient care, patients must travel to a DHB providing PRS services.
The delivery of tertiary PRS services at the DHBs affects the workforce requirements in each region. For example, there are four regional PRS burns centres at the Waikato, Hutt Valley and Christchurch regional PRS service centres, while the Counties Manukau regional PRS service centre provides regional burns services and also hosts the National Burns Centre. There are approximately six PRSn practising in these four regional PRS service centres who primarily provide burns services to patients from their regional catchments. Similarly, cleft lip and palate services are also provided in these four regional PRS service centres by eight surgeons, and craniofacial surgery is provided in two locations by five surgeons. Supra-regional services such as vascular anomalies including laser surgery, gender affirmation surgery, head and neck resection and reconstruction, skull base surgery and sarcoma reconstruction are also provided by one or more of these regional PRS service centres. It is recognised that this simple population based model is imperfect as the catchment area for subspecialised tertiary hospital services will encompass multiple regions thereby slightly underestimating the workforce needs of large regional centres and overestimating the needs of the smaller centres.
The majority of the 72 registered PRSn have public hospital appointments which provide almost 50 FTE PRSn nationwide, with only 13 (18%) practising exclusively privately. Private practice provides both cosmetic and reconstructive plastic surgery including Accident Compensation Corporation funded services, melanoma and non-melanoma skin cancer surgery, breast reconstruction and other PRS services such as breast reduction and setback otoplasty, which are underserviced in most of the public PRS service centres. Specific services provided by individual DHBs are beyond the scope of this paper; however, it is self-evident that with improved resourcing of PRSn, more adequate public PRS services can be offered. For example, the Counties Manukau and Canterbury PRS service centres have the highest FTEs per 100,000 population served (Table 1) and provide reasonable access to both breast reduction and otoplasty services through the public hospital system. The PRS service centre based at Hutt Valley DHB has a large geographical catchment area and the lowest FTEs per 100,000 population served of the four regional PRS service centres (Table 1), so does not have the capacity to provide such worthwhile services.9,10 Maldistribution of PRSn has therefore created a ‘postcode lottery’ whereby access to public PRS services depends on which DHB the patients are domiciled.
Demand for PRS services is predicted to increase with accelerated population growth, particularly within the over-65 age group. By 2036, 258,500 people will be over the age of 65—a 77 per cent increase from 2016,8 35 per cent of whom will be over 80 years old. In contrast, there will only be a 7.6 per cent increase in those under 14 years old.11 A large proportion of the workload within the public PRS service centres is the management of skin cancer, of which New Zealanders have the second highest rate in the world (33.3/100,000 age-standardised).12 The demand for PRS services per capita will therefore rise steeply with the nation’s changing age distribution. This underscores the need to meet the ideal PRSPR of 1:60,000, to ensure adequate and equitable access to PRS services.
It is predicted that provincial centres will have greater than the national average proportion of older adults, while Auckland is forecast to have a median age below the national average.13 This disparity in age distribution between larger urban centres and smaller provincial centres means that a pure population estimate will overestimate the need for large ‘younger age’ centres and underestimate the need for smaller ‘older age’ provincial centres. By 2043, the projected average age of patients for smaller provincial centres will vary from 37 years in Palmerston North to over 50 years in Kaipara, Thames-Coromandel, Hauraki, Central Hawke’s Bay, Horowhenua, Kapiti Coast, South Wairarapa, Tasman, Marlborough, Timaru and Central Otago districts, and Nelson city.13 Patients in these smaller centres are at risk of reduced access to PRS services due to their relative remoteness from the current seven public PRS service centres.
The vast maldistribution of PRSn leads to unequal access to PRS services. In 2013, a NZ PRS workforce analysis identified this maldistribution within the PRS workforce and recommended an increase in the number of centres offering public PRS services nationwide from six to a total of 12, to ensure equitable access of public PRS services to all New Zealanders.3 These 12 proposed PRS service centres could arrange themselves into clusters or ‘hubs and nodes’ working collaboratively within their regions. Regional PRS centres have so far failed to correct this vast maldistribution despite the local population needs. Attempts by local DHBs to establish a new PRS service centre in Hawke’s Bay DHB in 201314 failed despite extensive planning from a Health Workforce New Zealand-commissioned working group that included clinicians of multiple disciplines and management from both Hutt Valley and Hawke’s Bay DHBs. A lack of government planning has led to an unintended consequence of decentralised DHB control of local service provision and therefore allowed the inequity to continue.
Conclusion
The NZ population has increased faster than predicted. Despite this, the overall PRSPR appears satisfactory for the ageing population. However, the vast PRSn workforce maldistribution remains unchanged, presenting a barrier to equitable access to PRS services, especially in provincial areas. A strong mandate from the central government is required to resolve this longstanding problem of increasing inequity to public PRS services in NZ.
Acknowledgements
We thank Michael Chapman of YJK Design for providing figures 1 and 2.
Disclosure
The authors have no conflicts of interest to disclose.
Funding
The authors received no financial support for the research, authorship and/or publication of this article.
Updated: new formatting (17 June 2021); new pagination (6 June 2023)