Background
Skin cancer places a substantial burden on health care in Australia. The largest number of cancers diagnosed in Australia each year will arise in the skin and amount to more than all other cancers combined.1,2 It is estimated that two out of three Australians will be diagnosed with non-melanoma skin cancer (NMSC) by the age of 70.3 Although the number of Australians diagnosed is high, associated mortality is relatively low if the condition is diagnosed and treated early.3 As our population continues to expand and grow older, the burden of disease associated with NMSC is likely to increase, which will exert pressure on health resources.4,5
In its early stages, most NMSC is amenable to treatment in an office setting with simple surgical techniques and anaesthetic maneuvers.3 A proportion of patients will require specialist surgical treatment, mainly owing to tumour site, size, proximity to important structures and cosmetic demands.3 Early diagnosis and treatment of NMSC improves patient outcomes and reduces the cost of care.3 Death from NMSC is rare but delays in treatment may lead to increase in tumour size and stage, which then require more complex treatment that increases morbidity.6 With finite resources available to treat NMSC, it is imperative that resources are optimised to achieve the greatest outcomes for the greatest number.
At present, specialist review in the Australian public healthcare system requires a general practitioner (GP) referral, which is triaged according to urgency, and the patient is placed on a waiting list for outpatient clinical review. Once the patient is reviewed, there is a further delay to definitive treatment amounting to days to weeks on a waiting list for surgery. Non-melanoma skin cancer may progress during this time and require more extensive, costly or complex surgery than would otherwise have been necessary.6,7
In the Australian public healthcare system, outpatient waiting times reflect the challenges in providing equitable and timely access to specialist-level care. A systematic review showed three overarching themes to categorise delays that may be regarded as targets to improve efficiency: resource alignment, operational efficiencies and outpatient processes.8 The goal would be to coordinate these to reduce waiting times. A model of care that offers same-day assessment and treatment would address all three themes concurrently. See-and-treat clinics have been trialled in a number of settings7,9–11 and shown a reduction in waiting time and high levels of patient satisfaction. They offer specialist diagnosis, assessment and definitive treatment in a single visit for a defined group of patients.10 This service benefits both patients and healthcare providers by reducing occasions of service and waiting lists.10
The aim of this project was to explore a comprehensive ‘see-and-treat’ model of care for patients with NMSC at our tertiary referral institution. It was hypothesised that (1) same-day assessment and surgical management of suitable NMSC patients would result in reduced waiting times and (2) surgical outcomes would be equivalent to standard care, with reduced costs and high levels of patient satisfaction.
Methods
Before implementing this new model of care, it was necessary to establish the volume of patients from the existing outpatient waiting list who would be suitable for the service in order to allocate the appropriate resources. Accordingly, inclusion and exclusion criteria based on the existing suitability for day surgery treatment eligibility were developed in consultation with our hospital’s specialist anaesthetic service (Appendix 1). A random sample of 100 referrals waiting to be seen found that 75 per cent would successfully negotiate first-pass screening. This meant that of the 170 patients waiting to be seen at that time, 130 (76.5%) could be suitable for treatment under the proposed model.
A team of key stakeholders was consulted, comprising representatives from plastic and reconstructive surgery, anaesthetics, nursing, patient liaison and general practice. The role of the GP in the workflow (Appendix 1) was critical to limit the number of postoperative visits to hospital but also offer improved GP engagement in the tertiary management of these patients. General practitioner willingness to be involved in the project was assessed through phone interview. One hundred and twenty-nine practices were contacted, and all were happy to be involved. An information event was held to inform referring GPs of the availability of the new model of care, introduce the referral pathway, provide information regarding assessment (including biopsy techniques) and clarify their role in the workflow (Appendix 1). The proposed model of care was then approved by the Princess Alexandra Hospital’s (PAH) executive based upon the business case presented.
The project was funded through a competitive grant for improved models of care offered by the Clinical Excellence Division of the Health Improvement Unit, Queensland Health. The funds were disbursed for a clinical nurse consultant to coordinate and run the clinic, additional outpatients and operating theatre resources and additional surgical clinician time. The funding period was 12 months. A steering committee and governance structure were established to oversee the project implementation. A successful proof-of-concept pilot study was then planned at a peripheral metropolitan hospital which had been offering a plastic surgery service for the treatment of skin lesions under a traditional model of care (Figure 1) for five years. This successful trial was undertaken on 25 November 2017.
The PAH’s ‘see-and-treat’ project began in February 2018. Once a fortnight, outpatient clinic space and the day surgical treatment unit (DSTU) was allocated to the project. Referrals received from the central referral hub were triaged by a consultant plastic and reconstructive surgeon. Patients with NMSC who met existing DSTU suitability, were independently mobile, had a body mass index (BMI) less than 35, and had transport and carer availability for 24 hours postoperatively, were included. Among those excluded were patients with melanoma skin cancers (excisional biopsy of suspicious pigmented skin lesions was acceptable), benign lesions, lesions on the leg, diabetes requiring insulin, anticoagulant treatment for comorbid conditions (excluding acetylsalicylic acid), those requiring ambulance transport, lesions requiring frozen sections and any case requiring special equipment outside of a usual set-up (Appendix 1).
Selected patients were contacted, and further screening was undertaken via telephone consultation to make a final assessment of eligibility. This is a billable service in Queensland Health. Eligible and consenting patients subsequently presented to PAH for same-day assessment and treatment. One or two patients who had already been seen and booked but who were suitable for day surgery treatment were treated first on the operating list (these were not project patients). This ensured that patients who had already been seen and booked for surgery through a standard model of care were not disadvantaged. It also allowed the consulting and operating sessions to run concurrently and on time. Otherwise, the consulting session would need to start before the operating list, affecting the scheduling template.
On the day of assessment and treatment, patients presented to the surgical outpatient clinic appropriately fasted from midnight (to allow anaesthetic choice). After being checked in, they were assessed by a consultant plastic surgeon. The consultation included a discussion of anaesthetic options (local anaesthetic, local anaesthetic with sedation, general anaesthetic) and establishment of a clear surgical plan with informed consent. The patient’s lesion(s) and planned method of reconstruction were clearly marked on the patient; patients were subsequently seen by the clinical nurse consultant and given information relating to their procedure and postoperative care. Patients were accompanied for the short walk to the DSTU and were checked in by administrative and nursing staff. A review by the anaesthetic team was undertaken where appropriate.
A bedside handover was then performed between the consultant plastic surgeon and operating registrar to clearly communicate the surgical plan. The patient was offered a final opportunity to ask any questions regarding their procedure and then taken into the DSTU operating room. The surgical procedure was performed by the registrar with support of the consultant plastic surgeon as required. More complex cases were scheduled for the latter part of the operating list so that the consultant plastic surgeon could be directly involved in the delivery of care and teaching after all the consulting for the day was completed. After their procedure, patients went to recovery and were then discharged home the same day.
A follow-up appointment with the patient’s GP was arranged before discharge from DSTU. This appointment was scheduled five to seven days after surgery for wound review and removal of sutures where required. A clinic review was also scheduled three to four weeks after surgery to review graft and wound healing, general patient progress and histopathology results, and to determine disposition. Patients were asked to complete a survey of their experience with the ‘see-and-treat’ clinic. Patient satisfaction was recorded via a Likert scale (Appendix 2). The opportunity was taken to reinforce primary prevention strategies, including the use of sunscreen, wearing of a hat and long-sleeved clothing and avoiding sun in the middle of the day.
Data were collected in a FileMaker Pro Advanced® database (version 12.0) (Claris International Inc, 475 Potrero Ave, Sunnyvale, CA 94085, United States), comprising patient name, age, lesion site and size, medical comorbidities, anaesthetic type, procedure type, reconstructive technique, histopathology, margins and complications.
Results
Of the patients referred to the PAH with NMSC between 1 February 2018 and 1 February 2019, 211 met the inclusion criteria. Of these, 206 (97.0%) proceeded to surgical treatment, comprising 286 skin lesions on 23 operating lists. An average of nine patients were treated per operating list, with an average age of 61 years.
The type of procedure undertaken was predominantly excision of a primary skin lesion (212 excisions, 74.1%). Other procedures performed were excisional biopsy (29/286, 10.1%), shave biopsy (17/286, 5.9%), punch biopsy (8/286, 2.8%) and re-excision of incompletely excised skin lesion (7/286, 2.5%). The anatomical location of the majority of these lesions was the face (216/286, 75.5%). Of these lesions, the nose was the most common anatomical location for treated lesions, making up 32.9 per cent (94/286). Facial lesions in other anatomical locations were distributed more evenly (Figure 2). Anatomical locations outside the face, including the trunk (19/286, 6.6%), upper limb (15/286, 5.2%), and scalp (11/286, 3.8%), were less common.
Most excision defects were reconstructed with primary closure (169/286, 59.0%). Full thickness skin graft (56/286, 19.5%) and local flaps (50/286, 17.4%) made up the majority of the remainder. Split thickness skin grafts (4/286, 1.3%) and healing by second intention (9/286, 3.1%) were uncommon. When offered a range of suitable anaesthetic techniques, most patients opted for local anaesthetic with sedation (117/206, 57.0%). Substantially fewer patients were comfortable with local anaesthetic only (84/206, 41.0%) and a minority opted for general anaesthesia (4/206, 2.0%). Given the inclusion and exclusion criteria (Appendix 1), it is likely that most patients would be fit for any anaesthetic technique, though data regarding this were not specifically collected.
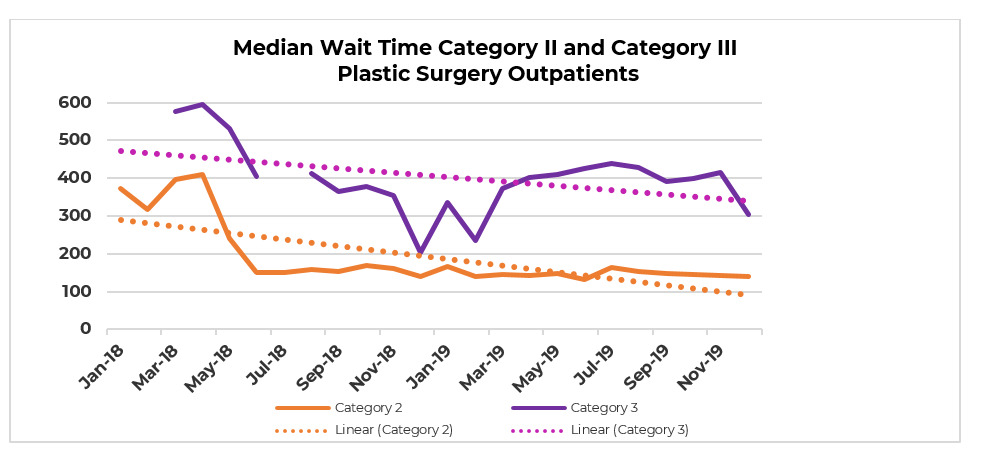
The ‘see-and-treat’ model resulted in a substantial reduction in waiting times at all stages of workflow. The average time from referral to treatment for NMSC became 38 days, which compares favourably with an average wait of 188 days prior to the commencement of the clinic. These patients had a significant reduction in occasions of service with 66 per cent discharged following a single review appointment. The average waiting time for suitable patients was reduced by 76 per cent, from 159 days to 38 days (see Figures 3 and 4). These changes are directly attributable to the ‘see-and-treat’ model of care provided by the project. Outpatient waiting lists for other categories of referrals also improved. Overall category I unbooked long-waits reduced by 100 per cent (200 to 0); category II unbooked long-waits reduced by 92 per cent (128 to 10); and category III unbooked long-waits reduced by 100 per cent (30 to 0).
Histological outcomes for excised lesions are presented in Table 1. Basal cell carcinoma (BCC) was the most common histological diagnosis (158/286, 55.2%) followed by no residual lesion after WLE of biopsy confirmed malignant skin lesion (89/286, 31.0%). Squamous cell carcinoma (SCC) (8/286, 2.8%) and melanoma (4/286, 1.4%) were all less common, as well as non-invasive skin cancers (intraepidermal carcinoma (18/286, 6.3%) and other benign pathologies (10/286, 3.5%).
There were 22 complications, affecting 7.5 per cent of procedures and 10.7 per cent of patients. These included graft failure (15/286, 5.2%), postoperative infection (12/286, 1.4%) and wound dehiscence (3/286, 1.0%). The total incomplete excision rate was 4.2 per cent (12/286) in 11 patients (Figure 5). The deep margin was involved in three excisions and in one additional excision where deep and lateral margins were involved (4/286, 1.4%). The histological diagnosis in all of these lesions was BCC of infiltrating sclerosing or micronodular subtype. The lateral margin was involved in excision of eight lesions (2.8%). The histological diagnosis in these lesions was BCC in six (two solid, two infiltrating/sclerosing, one micronodular and one superficial multifocal), squamatised BCC in one and moderately differentiated SCC in one. The superficial multifocal BCC was arising in field change and did not require re-excision. Re-excision to achieve a clear margin was successfully performed in all other cases. Therefore, only 11 of the 12 lesions with a positive margin required re-excision, bringing the clinically significant positive margin rate to 3.8 per cent.
The total hospital cost for the management of a patient through the project is AU$3258. An estimated cost of managing a patient in the traditional setting, based on activity based funding data, is AU$4597 (new appointment AU$216 + preadmission clinic AU$216 + AU$404 + AU$420 + surgery AU$3125 + postoperative review AU$216).12 This presents a gross cost saving of AU$1339 per patient managed through the project (Appendix 3). There is also a reduction in costs to the patient. These are difficult to measure but when surveyed, patients reported reduced travel time and related costs as well as less downtime and time off work.
The clinic was regarded as a convenient, efficient same-day service resulting in reduced stress and sick leave, less waiting and reduced occasions of service (Figure 6). All patients surveyed (Appendix 2) (n = 120) would recommend the ‘see-and-treat’ clinic to a suitable patient. Patient’s Likert scale satisfaction scores on key variables included quality of care 9.6/10, procedure outcome 9.1/10, recovery process 8.8/10 and treatment process 9.6/10.
Discussion
We believe that the anatomical distribution of lesions treated in the project’s clinic would be in keeping with a tertiary referral plastic and reconstructive surgery service. The fact that nearly one-third of all treated lesions were on the nose is further confirmation of this. Basal cell carcinoma is the single most common histological diagnosis for skin lesions in Australia.13 The histological outcomes and distribution of types of reconstruction from the clinic are, in our view, also in keeping with a dataset that is representative of tertiary plastic and reconstructive surgery practice in Australia.
The incidence of surgical complications at the clinic is comparable to other series.14 There was a total of 22 complications across 286 excisions: graft failure (5.2%), postoperative infection (1.4%) and dehiscence (1.0%). A clinically significant positive margin rate of 3.8 per cent compares favourably to other series,15 which should not be surprising as the lesions suitable for treatment in the clinic are the ‘low fruit’ by design, and one would expect a better margin control than for a unit-wide series of excised NMSCs. This should be balanced against the fact that lesions suitable for the clinic are those that arise in anatomical locations conducive to ambulatory care (nose, eyelids, ears) and are recognised as having a higher risk of positive excision margins.
This study demonstrates that the ‘see-and-treat’ model of care is a successful, efficient and fiscally beneficial model of care for suitable patients. The resources necessary to provide this service were assembled with the help of a grant but existing public hospital resources could be used to implement this model of care. The majority of patients were seen only twice: on the day of initial appointment and surgery, and then at one follow-up appointment. This is fewer than a traditional model of care with at least three patient encounters, and occasionally more, particularly where there is a postoperative complication. The ‘see-and-treat’ model leads to a reduction in cost for both the hospital and the patient, and overall increased patient satisfaction. Removing these patients from routine outpatient clinics and operating lists frees up resources for more complex cases. This is demonstrated in the unanticipated but welcome reduction in waiting times for category II and III referrals (Figures 3 and 4).
‘See-and-treat’ approaches to NMSC management have been trialled elsewhere7,9–11 and have been incorporated to varying degrees into private surgical practice for some time. These models are often limited by the capacity to offer surgical treatment under local anaesthetic only, for example a study based in New Zealand by McLaughlin and colleagues.7 Our model differs by virtue of being highly collaborative, incorporating GPs, anaesthetists and specialist nurses into its workflow. In our series of patients, more than half (57%) opted for surgical treatment under local anaesthetic with sedation. This is not a service that can be provided outside of a day surgery facility and without the input of a specialist anaesthetic service.
Our data suggest that while a same-day service that offers local anaesthetic only may be useful, adding anaesthetic support to this service and thereby offering a range of anaesthetic options is important. Given the survey data, a same-day service is appealing to patients. Patients who are not comfortable with local anaesthetic may then be forced to weigh up this discomfort against the benefits of a same-day treatment. Patients who have an unpleasant experience are less likely to seek early assessment of lesions and may end up requiring more complex treatment for other lesions in the future.6,7 Feedback from GPs is positive and related to better engagement with the tertiary service provided to their patients and opportunities for education. Registrars are also afforded a better learning experience with real-time consultant involvement in planning and performing complex cases.
Conclusion
The introduction of a ‘see-and-treat’ model of care significantly reduced the Princess Alexandra Hospital’s waiting list and times. We believe that it provides a blueprint for surgical innovation that can be extended beyond skin cancer and into other areas that may benefit from a new approach. Ongoing funding for the project has been secured and the model has been expanded to include the management of suitable patients with in-situ and type 1a invasive melanoma with plans to extend into hand surgery services in the near future. This model of care has been implemented at other care facilities within the same health service. The recent pandemic also provided the opportunity to implement telehealth as a modality for follow-up to further reduce the occasions of service required in the hospital environment. This is a feature that is likely to continue as part of this model of care even after the pandemic abates.
Our healthcare system is under increasing pressure to deliver high-quality healthcare within the limitations of finite resources. As the Australian population ages and grows, it is imperative that innovative ideas be explored to provide solutions to our healthcare needs.
Patient consent
Patients/guardians have given informed consent to the publication of images and/or data.
Conflicts of interest
The authors have no conflicts of interest to disclose.
Funding declaration
Provision of funds for this project was obtained through a competitive grant from the Clinical Excellence Division of the Health Improvement Unit, Queensland Health. The authors received no financial support for the research, authorship, and/or publication of this article.
Revised: March 8, 2021 AEST
_model.jpg)



.png)



_model.jpg)


.png)


