Introduction
We present a case of positron emission tomography (PET)–avid internal mammary lymphadenopathy, prompting open excisional biopsy of the lymph node in the setting of concern about breast-implant associated anaplastic large cell lymphoma (BIA-ALCL) or breast cancer recurrence. Histopathological examination revealed reactive lymphadenopathy with tattoo ink and no malignancy. We undertook a review of the literature to investigate the frequency of tattoo ink related PET-avid lymphadenopathy, and false positive PET scan results from tattooing. Lymphadenopathy related to tattoo ink has been reported previously, however this is the only case of benign PET positive tattoo lymphadenopathy resulting in unnecessary invasive surgery reported to date.
Case report
A 54-year-old woman presented in January 2020 with acute onset left breast pain. Her background medical history includes left T2N1M0 hormone positive Her2 negative breast cancer diagnosed in 2004. In the same year, she underwent a left skin sparing mastectomy and axillary lymph node dissection, followed by a textured breast implant insertion (Natrelle®; Allergan Inc, Longphort House, Block J, Leeson Street Lower, Saint Kevin’s, Dublin 2, D02 NY60, Ireland) and contralateral mastopexy. In the years following her breast reconstruction she commissioned a large cosmetic tattoo on the reconstructed breast which represented part of her psychosocial recovery from breast cancer (Figure 1).
The morning of her presentation she woke with sudden onset pain in her left breast and a sensation that the implant had migrated. She had no constitutional symptoms. On examination the reconstructed breast appeared grossly normal although was tender to palpation.
Her full blood count, urea, electrolytes and creatinine were normal except for a mildly raised white cell count of 13.5 x10^9/L (Normal 4–11 x 10^9/L). Ultrasonography of her left breast and axilla showed a small volume periprosthetic effusion within the fibrous capsule. There were no axillary lymph nodes identified. She required an overnight stay in the emergency department for analgesia before being discharged home.
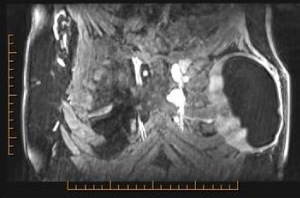
She went on to have a MRI scan to exclude device rupture which showed an enhancing periprosthetic fluid collection surrounding an intact implant. There was abnormal enhancement of the lymph nodes in the left second and third intercostal space and an enlarged node in the fourth intercostal space (Figure 2). An ultrasound guided fine needle aspirate (FNA) of the left pericapsular fluid and internal mammary node was then completed. The pericapsular fluid showed no sign of malignancy with a population of small to medium lymphocytes. The flow cytometry for this specimen showed a normal lymphoid population and surface molecule expression. The left internal mammary node FNA was non-diagnostic, and due to the location of the node, core biopsy was deemed unfeasible.
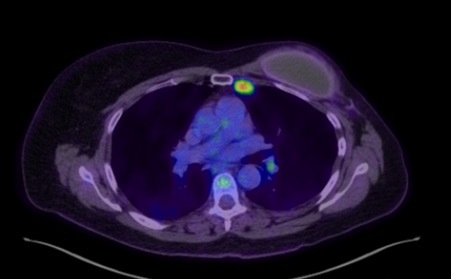
A PET CT scan following the FNA showed intense fluorodeoxyglucose (FDG) uptake in two enlarged left internal mammary lymph nodes at the second and third intercostal space with standardised uptake value (SUV) max of 7.35 (Figure 3). Low grade FDG uptake, likely reactive or inflammatory, was seen in the left axilla and bilateral cervical nodes. There was no significant uptake surrounding left breast prosthesis.
Given the grossly abnormal imaging findings, open biopsy of the node was mandated by a multidisciplinary meeting involving breast and plastic surgeons, oncologists and radiologists. The internal mammary nodal chain was approached by removal of the fourth costal cartilage. Intraoperatively, a minimal amount of periprosthetic fluid was seen and the implant was not ruptured. The histopathology of the breast capsule and implant showed mixed inflammation and perivascular aggregates of small lymphocytes. The seroma fluid contained predominantly blood with scattered macrophages. An enlarged black node was removed from the left third intercostal space. Microscopic examination showed a reactive node with tattoo pigment consistent with the large tattoo on her left breast. No sign of malignancy was seen in any of the specimens. Three months after these extensive investigations the patient was able to undergo autologous reconstruction of the breast with a deep inferior epigastric perforator flap.
Discussion
The popularity of tattoos is increasing both for cosmetic and medical reasons with 10 per cent of Australians having at least one tattoo.1 Nipple tattooing in breast reconstruction is relatively common and offers significant improvement in patient satisfaction.2 Following tattooing, the carbon-based pigments can activate macrophages and white cells to migrate to the regional lymph nodes. The pigment may then cause a foreign material reaction, non-caseating granulomas then persist for years propagated by delayed type hypersensitivity. Tattoo lymphadenopathy has previously been reported to raise a diagnostic dilemma in cases involving melanoma as the enlarged, pigmented node was concerning for metastases.3–7 In these cases the lymphadenopathy was diagnosed at the time of presentation or the enlarged pigmented lymph nodes were discovered during a sentinel lymph node biopsy.
The use of PET scanning is expanding with applications ranging from diagnosis, staging and surveillance of malignancy to detecting infection and regions of inflammation. The avidity of a FDG-PET scan relies on radio-labelled fluoro-deoxy-glucose (18F) uptake by cells with higher turnover and metabolic rate.8,9 False positive results in up to 6.5 per cent can occur due to concurrent inflammation, such as post-surgical, radiation, chemotherapy or infection.10 It is presumed that the tattoo ink inflammatory and hypersensitivity reaction is responsible for the observed PET avidity.
We searched the PubMed®, Cochrane and Medline® databases for publications in English between January 1966 to and April 2020 using the terms ‘tattoo’ and ‘PET’ or ‘positron emission tomography’. Our predetermined inclusion criteria were articles which reported false positive PET scan as a result of tattoo lymphadenopathy.
Our literature review resulted in five case reports of PET-avid lymph nodes from tattoo inflammation (Table 1). Patients ranged from 32–48 years of age with tattoos performed between 1.5 and 24 years prior to PET scanning. Pathologies prompting the PET scans included sarcoidosis, thymoma, lung, cervical and testicular malignancies. Four patients had biopsy of the lymph nodes for histological diagnosis, which confirmed reactive lymphoid tissues with black ink pigmentation.
In the literature review, PET-avid lymph nodes were found related to tattoos where scans were performed to investigate lung, melanoma, thymoma, cervical cancer and sarcoidosis.11–15 In some cases, nodal avidity was even higher than the primary tumour. These false positive PET scans have the potential to cause a great deal of anxiety for patients and potentially over-investigation, prompting invasive procedures.
In the reported case, the diagnostic dilemma raised was the presence of lymphadenopathy in the setting of breast pain, textured breast implant, peri-prosthetic implant fluid, a non-diagnostic FNA and PET avidity of the node. Breast-implant associated anaplastic large cell lymphoma is an uncommon T cell lymphoma arising around textured surface breast implants, including those used in post-mastectomy breast reconstruction.
Symptoms of BIA-ALCL include pain, swelling, asymmetry and seroma. In our patient presenting with sudden breast pain, concerning differential diagnoses included implant rupture or BIA-ALCL. The investigative algorithm for BIA-ALCL includes contrast enhanced MRI, ultrasound and fluid aspirate for cytology and to test for immunohistochemistry markers CD30 and ALK (CD30 positive and ALK negative in BIA-ALCL). It is recommended to use PET CT in confirmed cases of BIA-ALCL to identify distant disease.
A MRI scan was performed to assess implant integrity, revealing the enlarged internal mammary lymph nodes. As the FNA on the enlarged nodes yielded an undiagnostic result, a PET CT was performed to investigate malignant potential. The PET CT had concerningly high FDG uptake, suggesting malignancy. Core biopsy might have avoided the invasive open procedure. Unfortunately, due to the location of the node it was deemed unfeasible. Open biopsy is not without risks, as resection of a segment of rib was required, a procedure that has been associated with cardiac tamponade and arrest.16
This case highlights the importance for clinicians and radiologists to be aware of the potential for tattooing to cause PET-avid lymphadenopathy. This is especially relevant given the prevalence of tattoos in post-mastectomy breast reconstruction, for whom lymphadenopathy raises concerns of breast cancer recurrence or BIA-ALCL. Treating teams need to be aware of the possible effects of tattoo ink on PET-CT findings while counselling patients and formulating treatment plans.
Conclusion
Positron emission tomography images from patients with large-volume tattoos should be interpreted carefully as avid uptake may be a result of tattoo inflammation. Radiology departments should consider documentation of tattoos in patient clinical information when processing PET scan requests to help accurately interpret the scan and reduce the risk of false positive results and further unnecessary procedures. Given the increasing prevalence of tattooing in the community it is anticipated that this phenomenon is under-reported and the true incidence actually higher. A prospective trial to accurately ascertain the frequency of tattoo related FDG avid lymphadenopathy, as well as identify possible risk factors such as specific pigments, is recommended.
Patient consent
Patients/guardians have given informed consent to the publication of images and/or data.
Disclosure
The authors have no financial or commercial conflicts of interest to disclose.
Funding declaration
The authors received no financial support for the research, authorship, and/or publication of this article.
Revised: 2021 January 30 AEST