Recent articles published on cosmetic surgery in the Australian media have exposed an industry that is dangerously under-regulated and allows medical practitioners with only a basic medical qualification and no formally accredited surgical training to perform major invasive surgery on an unsuspecting and largely medically illiterate public, in facilities that would not ordinarily meet the regulatory standards for a hospital or day surgery facility. Patients have falsely believed that the person operating upon them was a fully trained surgeon and had undergone accredited surgical training. We know this because every week, as plastic surgeons, we see multiple patients who have been maimed and harmed by these individuals. They exploit a loophole in the regulations that allows anyone with a basic medical degree to call themselves a ‘cosmetic surgeon’.
All surgery entails risk. Cosmetic surgery is no different. There is no such thing as risk-free surgery. The only way to mitigate, but not eliminate, this risk is to ensure that the person who is about to operate upon a patient is properly trained and is actually a surgeon.
The scientific literature is clear that the two key individual or surgeon components directly influencing surgical risk are the training an individual surgeon has received and the number of operations he or she has performed. Complication rates are lowest when surgeons are well-trained and perform large volumes of similar surgical procedures.
This direct relationship between surgical practice and outcome was first suggested by Ericsson and colleagues in 1993.1 In their landmark ‘10,000 hours’ paper investigating the attainment of a particular skill, the authors proposed that if individuals engage in deliberate practice, ‘the amount of time spent practising…will be monotonically (in a straight line) related to that individual’s acquired performance’. On average it takes 10,000 hours to achieve expertise in any given field.
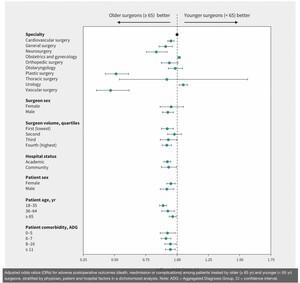
The importance of the time spent practising to achieve a surgical skill—and subsequently to complication rates, is widely reported in the literature. For example, a 2020 study analysing the relationship between surgeon age and postoperative outcomes found that, with the exception of urology and gynaecology, surgeons aged over 65, and therefore presumably having had a longer time to practise surgery, had lower complication rates than younger surgeons, particularly in plastic surgery.2 The complication rate progressively decreased as surgeons got older (Figure 1).
But experience by itself is only half of the story. The training provided to an individual has also been found to be of critical importance. Indeed, training was a key part in the original ‘10,000 hours’ paper. Training, or as Ericsson and colleagues called it, ‘the deliberate practice’, must be structured and entail focused practice under direct supervision and tuition, with feedback. It follows that the instructor, and the type of tuition is critical.
The journey to truly superior performance is neither for the faint of heart nor for the impatient. The development of genuine expertise requires struggle, sacrifice, and honest, often painful self-assessment. There are no shortcuts. It will take you at least a decade to achieve expertise, and you will need to invest that time wisely, by engaging in “deliberate” practice—practice that focuses on tasks beyond your current level of competence and comfort. You will need a well-informed coach not only to guide you through deliberate practice but also to help you learn how to coach yourself.3
This is also supported in the literature. A 2020 study looking at the time taken for recently graduated plastic surgeons in the UK to acquire the additional skills necessary to perform autologous breast reconstruction using a DIEP flap (in the UK, not Australia) in three differing training institutions found that all three groups eventually acquired the necessary skills but there was a longer learning curve in the non-specialised facility and that specific directed teaching and training by specialist surgeons leads to a ‘quicker attainment of the necessary’ skills.4
This importance of surgical training is reflected in other studies. In their systematic review of cancer surgery literature, Bilimoria and colleagues assessed the effect of surgeon training, specialisation and experience on outcomes for cancer surgery showing that in 25 of the 27 studies analysed, surgical specialisation with specialist training and increased surgeon experience correlated with better outcomes and lower complication rates.5
In a retrospective study of gynaecological complications in 2000 patients undergoing laparoscopic gynaecological total hysterectomy (TLH) at the same single institution, the incidence of any major intraoperative complication was significantly lower among surgeons with subspecialist training compared to general gynaecologists (1.1% vs 3.3%, p = 0.002) and ‘despite a higher level of surgical acuity and the performance of additional and more complex procedures, surgical morbidity was lower in patients undergoing TLH by gynaecologic surgeons with a higher level of subspecialist training’.6
A British study examining recurrent laryngeal nerve palsy in thyroid surgery found complication rates were directly related to the number of operations a surgeon had performed and the training provided. Beginner resident surgeons under direct supervision by an experienced mentor had very low complication rates. The incidence of nerve palsy then increased when the supervision was stopped, peaking after further experience up to the fiftieth operation before decreasing exponentially to under 1 per cent after another 130 operations.7
Locally, Deva and colleagues found that the incidence of ‘double bubble’ or breast implant malposition related to surgical technique was 2.1 times higher when the breast augmentation surgery was performed by non-specialist practitioners with a ‘general’ Australian Medical Council (AMC) registration as compared to an AMC accredited specialist plastic surgeon.8
In summary, the literature highlights that the very worst outcome occurs when a medical practitioner with little or no training embarks upon surgery in the infancy of their career, with no supervision. And yet this is exactly what is currently happening in cosmetic surgery in Australia.
Drawn by the opportunity to make eye watering amounts of money with no additional training, new medical graduates are flocking to cosmetic surgery and medicine in unheralded numbers. Operating without formal accredited surgical training or supervision and clearly inadequate ‘deliberate practice’ hours, their results and complications could be predictably foreseen from any analysis of the widely published literature.
Worse, within Australia, existing regulations allow these individuals to be able to camouflage their dangerous lack of training and experience and use carefully scripted social media websites to convince the public, and the regulators, that as so-called ‘cosmetic surgeons’, they are the experts in 'cosmetic surgery’.
In Australia, the only independent body formally accrediting medical training programs is the AMC. The AMC accredits ophthalmology, dentistry, obstetrics and gynaecology, medicine, surgery, and many other training programs to a national predetermined standard.
As would be expected, this body not only meticulously scrutinises medical training but also specifies the ‘extra’ skills required to become a surgeon. Through the Royal Australasian College of Surgeons (RACS) these skills form a set of 10 key competencies that are fundamental to becoming a surgeon in Australia and New Zealand.9 They are taught, examined and form part of the RACS continuing professional development (Figure 2).
Surgical training is not only about being able to perform a particular surgical procedure safely; it is also about training to be a ‘doctor’ first. All surgeons must operate within a strong ethical and moral framework. This should fundamentally guide decision-making and must place the patient at the centre of any medical care. If we were to single out the most appalling aspect of what was exposed on the recent Four Corners and 60 Minutes television programs, it was a complete lack of empathy, of integrity, and of ethics and care.
Moving forward, it would make sense that, as a prerequisite, any medical practitioner undertaking surgery in Australia must be accredited by the AMC and must also adhere to these 10 surgical competencies. Australian Medical Council surgical training takes a minimum of an additional five years on top of three years of basic general resident surgical training. That is, more than 10,000 hours of deliberate supervised practice, and therefore fits within the Ericsson model of the attainment of expertise in a particular skill. The 10 competencies ensure the surgeon is holistic, fully trained and performs to the standard the community demands and expects.
Formal accreditation by the AMC would therefore provide an independent guarantee as to the level and type of specialised training a particular individual has received and would serve as a benchmark of that individual’s surgical experience and competency. We already require this of all our surgeons operating in the public hospitals of Australia, but not in private. We don’t understand why not?
The regulation of the cosmetic surgery industry in Australia is broken and is currently not working. People are being hurt. We urgently require an independent, objective investigation into cosmetic surgery regulation. This investigation must have the power to force the disclosure of critical documents that will almost certainly be withheld and the capacity to provide legal protection to the nurses, doctors and patients who bravely come forward to testify. This enquiry will take time.
In the interim, a national requirement that all practitioners performing surgery must have received training to the Australian Medical Council standard in the surgery that they are performing, would be a logical first step.