Summary
Gender-affirming mastectomy (‘top surgery’) is one of the most commonly requested and performed procedures in the transgender, non-binary and gender non-conforming population. The goal of surgery is to treat gender dysphoria by creating an aesthetically pleasing male chest, achieved by removing excess breast tissue and skin, and repositioning and resizing the nipple-areola complex.
We present a modification of the double-incision, mastectomy with free nipple graft (DIFNG) technique that we have called the ‘Pisces’ mastectomy as it is common for fish to exhibit gender fluidity. With some imagination, the skin excision could also be considered fish-shaped. This technique achieves the goals of surgery, provides good access for haemostasis and decreases the need for revision surgery by adequate removal of ‘dog ears’ medially and laterally.
Introduction
Top surgery is one of the most commonly requested and performed procedures in the transgender, non-binary and gender non-conforming population, as patients often define their masculinity by being able to expose their bare chest.1–3 It is an important treatment modality in relieving gender dysphoria. In addition, it helps patients to reach their gender goals, especially as hormonal treatment has little influence on breast size.2–4 The first FtM top surgery case series was published in 19955 and although a large body of literature exists regarding subcutaneous mastectomies in women with breast disease or men with gynaecomastia, there is sparse literature on FtM top surgery.5 While similar in some aspects, FtM top surgery has its own unique goals specific to the transgender, non-binary and gender non-conforming.1 Several operative techniques have been described, including a peri-areolar, concentric circular, transverse or extended concentric circular and an inferior pedicled mammaplasty.1,2,6 The most commonly used technique is the DIFNG.4
Operative technique
All cases were performed under general anaesthesia at a major hospital. Photos and markings were performed preoperatively with the patient standing with arms by their sides.
The upper horizontal line and the lower horizontal line are marked at a level to match the lower border of the pectoralis major muscle. Of note, the lower horizontal line is 2–4 cm higher than the inframammary fold. The lines of excision are extended superolaterally to match the lateral border of the pectoralis major muscle. Burow’s triangles are added medially and laterally to excise dog ears.
A complete subcutaneous mastectomy is performed, with care to excise all breast tissue at the peripheral limits of the breast in order to ablate the inframammary fold and ensure smooth skin flaps, and to avoid any contour memory of a breast.
The skin flaps are quilted to the chest wall and the wound is closed in layers over a drain.
Free nipple grafts are performed by thinning of the nipple-areola complex. The areolar diameter is set at 25 mm and the nipple projection is reduced by adequate thinning of the subareolar tissue. The nipple is inset and quilted with non-absorbable sutures in a position just lateral to the mid-clavicular line at the greatest convexity of the lower border pectoralis major muscle.
Patients are placed in compression vests in the immediate postoperative period. Patients stayed in hospital 1–3 nights. Drains were removed when output was less than 20ml/day. Stitches were removed from the nipple grafts at day 10–12.
Case 1
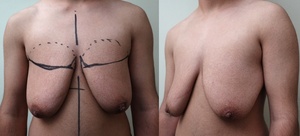
The first case demonstrates the use of the technique in a 22-year-old with medium-size breasts. Figure 1 shows preoperative markings. Figure 2 demonstrates the postoperative result at six months.
Case 2
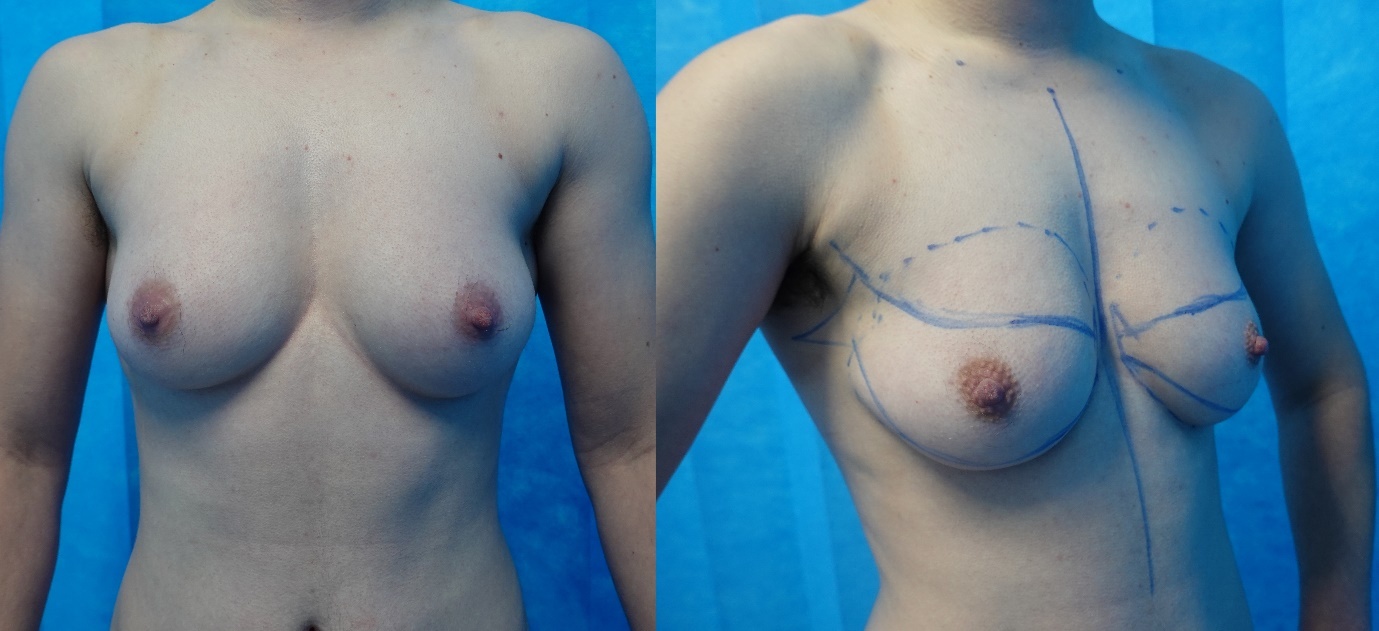
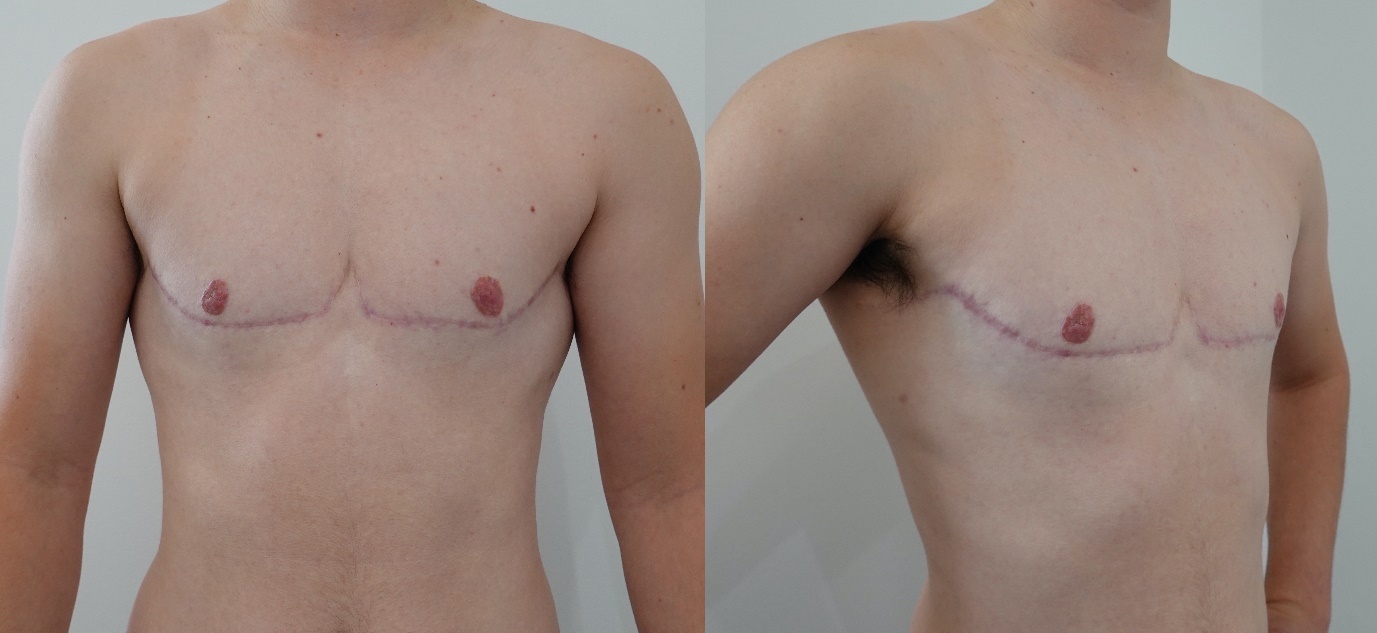
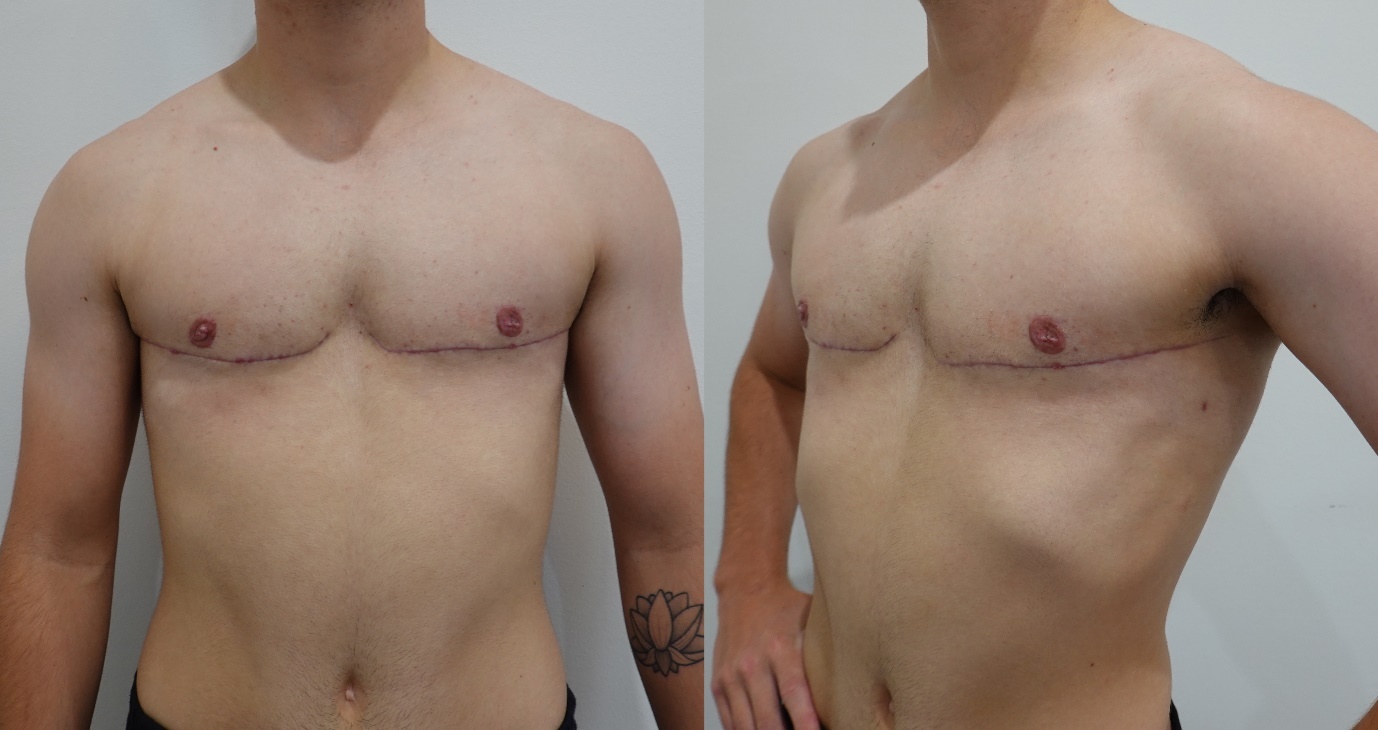
The second case demonstrates the use of the technique in a 22-year-old with small breasts. Figure 3 shows preoperative markings. Figure 4 demonstrates the postoperative result at six weeks.
Case 3
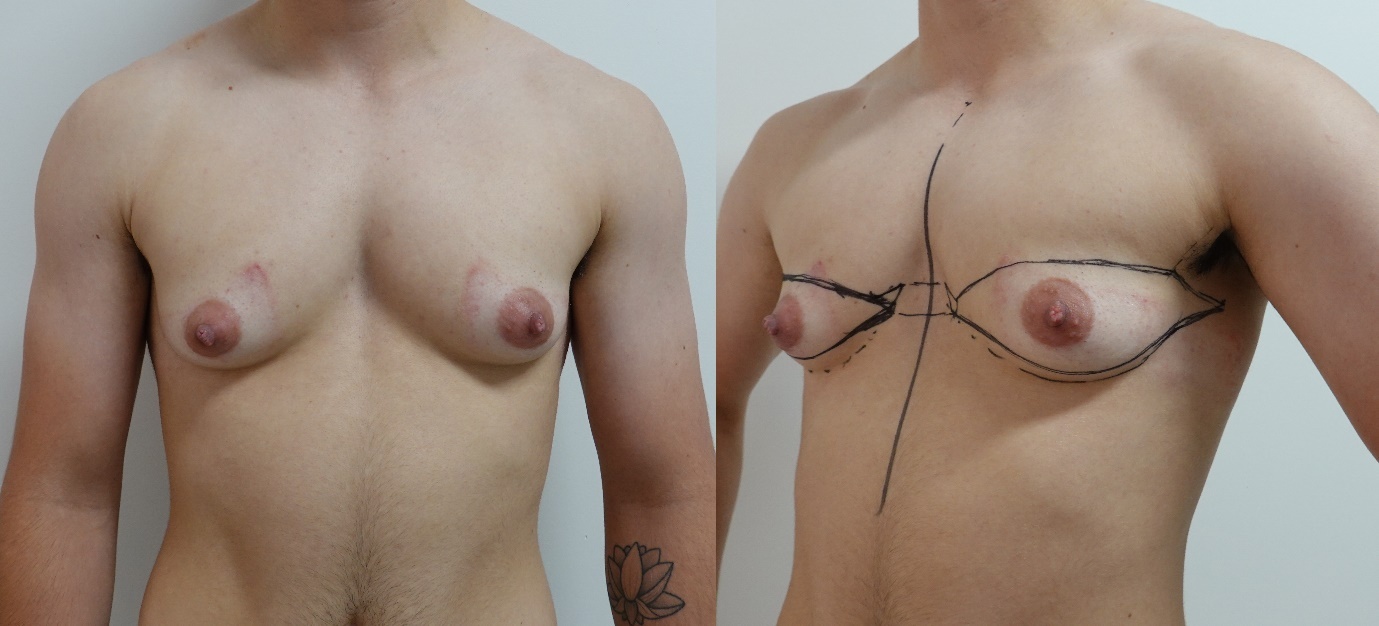
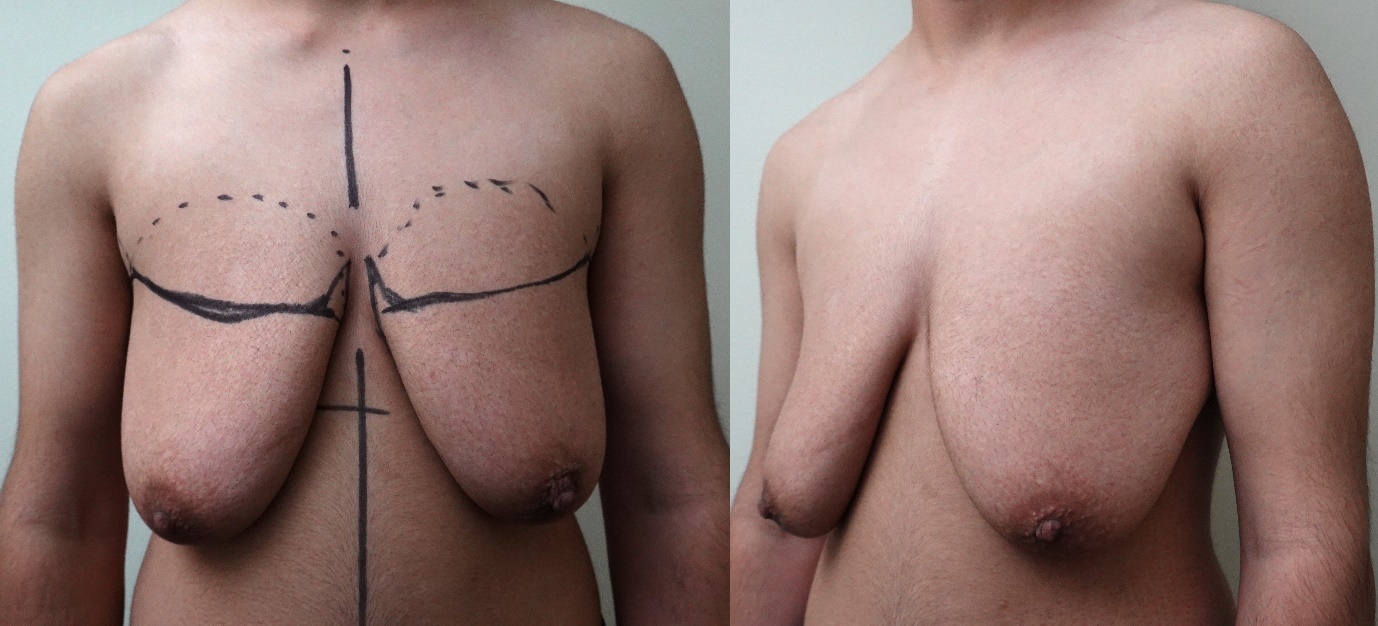
The third case demonstrates the use of the technique in a 21-year-old with large breasts. Figure 5 shows preoperative markings. Figure 6 demonstrates the postoperative result at six months.
Discussion
The objective of FtM top surgery is primarily to treat gender dysphoria by creating an aesthetically masculine chest. This is achieved by removing breast tissue and excess skin, and by repositioning and reducing the size of the nipple-areolar complex (NAC).2,3 Obliteration of the inframammary fold is vital as the masculine chest does not have this feature. It is the inferior margin of the pectoralis major muscle that delineates the inferior limits of the masculine chest.2,7
Several techniques have been described and algorithms have been proposed for choosing the optimal technique for FtM top surgery based on breast size, skin quality, degree of ptosis and size of the NAC.2,5,8 There remains debate over the optimal technique to achieve the best aesthetic outcome while minimising postoperative complications.8
The technique described is a modification of the DIFNG. The goal of this modification is to create a scar that follows the inferolateral border of the pectoralis major muscle to emulate the masculine form. The advantages of this technique are therefore in part aesthetic, but also the long incision allows good visualisation for smooth flaps, provides confidence in ablating the edges of the breast and also allows good haemostasis. This can result in a smooth flat finish with a scar that mimics the pectoralis major fold. The long incision also allows excision of dog ears laterally and medially, minimising the need for revisional surgery. This technique is versatile and can be used in patients with small to large breasts with varying degrees of ptosis.
A limitation of this technique is the length of the scar. For patients who are scar averse, preoperative discussions should be directed at the advantages and limitations of other techniques. It is our experience that most patients do not mind the scar and see it as a necessary evil to achieve an arguably better cosmetic result.
Conclusion
Current literature regarding FtM top surgery supports the use of more invasive techniques with longer scars to achieve a better aesthetic outcome,2,5,6,8,9 minimise the risk of haematoma5,8 and reduce the rates of revisional surgery.2,4–6,9 This certainly reflects our experience with this technique as it results in a flatter, better contoured chest when compared to limited scar approaches, making it our favoured technique for FtM top surgery for the vast majority of patients.
Patient consent
Patients/guardians have given informed consent to the publication of images and/or data.
Conflict of interest
The authors have no conflicts of interest to disclose.
Funding declaration
The authors received no financial support for the research, authorship, and/or publication of this article.
Revised: October 27, 2021 AEST