Introduction
Australia has one of the highest incidences of skin cancer in the world. It is two to three times that of the United States of America, Canada and the United Kingdom.1 Cutaneous malignancies account for approximately 80 per cent of all newly diagnosed cancers in Australia. In 2020, melanoma was the third most common cancer in Australia, excluding all non-melanotic skin cancers (NMSCs).1,2
The coronavirus disease (COVID-19) pandemic led to the Australian state and federal governments implementing a range of coordinated measures aimed at reducing disease transmission and preventing the healthcare system from being overwhelmed. As part of this response, all non-urgent elective surgery was suspended from 25 March 2020, with hopes to ensure adequate hospital capacity and preservation of personal protective equipment.3,4 Outpatient services were also encouraged to transition to telehealth with the addition of temporary government rebates for telehealth consultations.5 These measures, as well as stay-at-home orders, resulted in an initial successful suppression in COVID-19 cases. Since the easing of the first lockdown period in May 2020, each state has planned to resume normal surgical activity in a staged manner.3
Despite continuation of category I elective surgery during the lockdown periods of the COVID-19 pandemic in Australia, service providers observed substantial reductions in the procedures relating to skin cancer investigation and treatment.5 This study aimed to quantify the impact of the COVID-19 pandemic on the diagnosis and management of cutaneous malignancies in Australia.
Methods
Data source and extraction
The Australian Medicare Benefits Schedule (MBS) database provides information on the use of a comprehensive range of government-subsidised services, including diagnostic procedures and investigations, and therapeutic interventions.6 Monthly data between January 2017 and June 2020 for service item numbers related to the diagnosis and management of cutaneous lesions and malignancies were extracted from the MBS database then stratified into three groups: diagnostic biopsies of skin (item number 30071), excision of NMSC (item numbers 31356, 31358, 31359, 31361, 31363, 31365, 31367 and 31369) and excision of melanomas (item numbers 31371, 31372, 31373, 31374, 31375 and 31376). Ethics board review and approval were not required given this study used publicly available data.
Statistical analysis
Holt-Winters modelling is a commonly used forecasting technique that applies triple exponential smoothing in order to capture and account for three key components in a time series: average values, trend over time and seasonality.7 In the present study, a Holt-Winters model was built using monthly data between January 2017 and December 2019 in order to predict monthly data between January 2020 and June 2020 with a 95 per cent CI. Observed monthly services between January 2020 and June 2020 were compared with predicted monthly services over the same period to calculate absolute and percentage residual differences (RDs). An RD was considered statistically significant if the observed data point was outside of the 95 per cent CI of the model’s prediction (p < 0.05). A total of three models were developed: (1) diagnostic biopsies of skin, (2) excision of NMSC and (3) excision of melanomas. All statistical analyses were performed using SPSS version 22 (IBM SPSS, 1 New Orchard Road, Armonk, NY, 10504-1722, USA) and LKS-CHART Forecasting Tool (St Michael’s Hospital, 36 Queen St E, Toronto, ON, M5B 1W8, Canada).
To determine the accuracy of fit of the model, the mean absolute percentage error (MAPE) between observed and predicted monthly services between January 2017 and December 2019 was calculated. The MAPE is one of the most commonly used metrics of model fit and predictive accuracy.8 To determine the six-monthly predictive accuracy of the model, cross-validation was performed by using observed monthly services between January 2017 and December 2018 to predict the number of monthly services between January 2019 and June 2019. The predicted number of monthly services was then compared with the observed number of monthly services for this same period in order to determine the MAPE in the model’s prediction. Model fit and predictive accuracy was calculated for all three models.
Results
Model fit and predictive accuracy
All three models demonstrated excellent model fit and six-monthly predictive accuracy. The model fit MAPEs for the biopsy, NMSC and melanoma models were 2.47 per cent, 2.19 per cent and 3.41 per cent, respectively.
Diagnostic biopsies of skin lesions
A total of 697,951 diagnostic biopsies of skin lesions were performed between January 2020 and June 2020. There was not a statistically significant difference between observed and predicted monthly skin biopsies in January 2020 and February 2020. There was a statistically significant reduction in skin biopsies performed in March 2020 (RD: –23,137, –15.6%, 95% CI: –20.7% to –9.9%), April 2020 (RD: –38,614, –31.0%, 95% CI: –35.8% to –25.4%) and May 2020 (RD: –30,350, –21.3%, 95% CI: –26.2% to –15.8%). There was not a statistically significant difference between observed and predicted skin biopsies in June 2020 (Figure 1; Table 1).
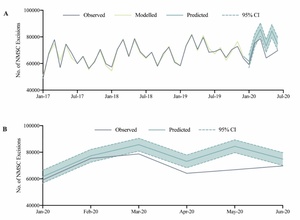
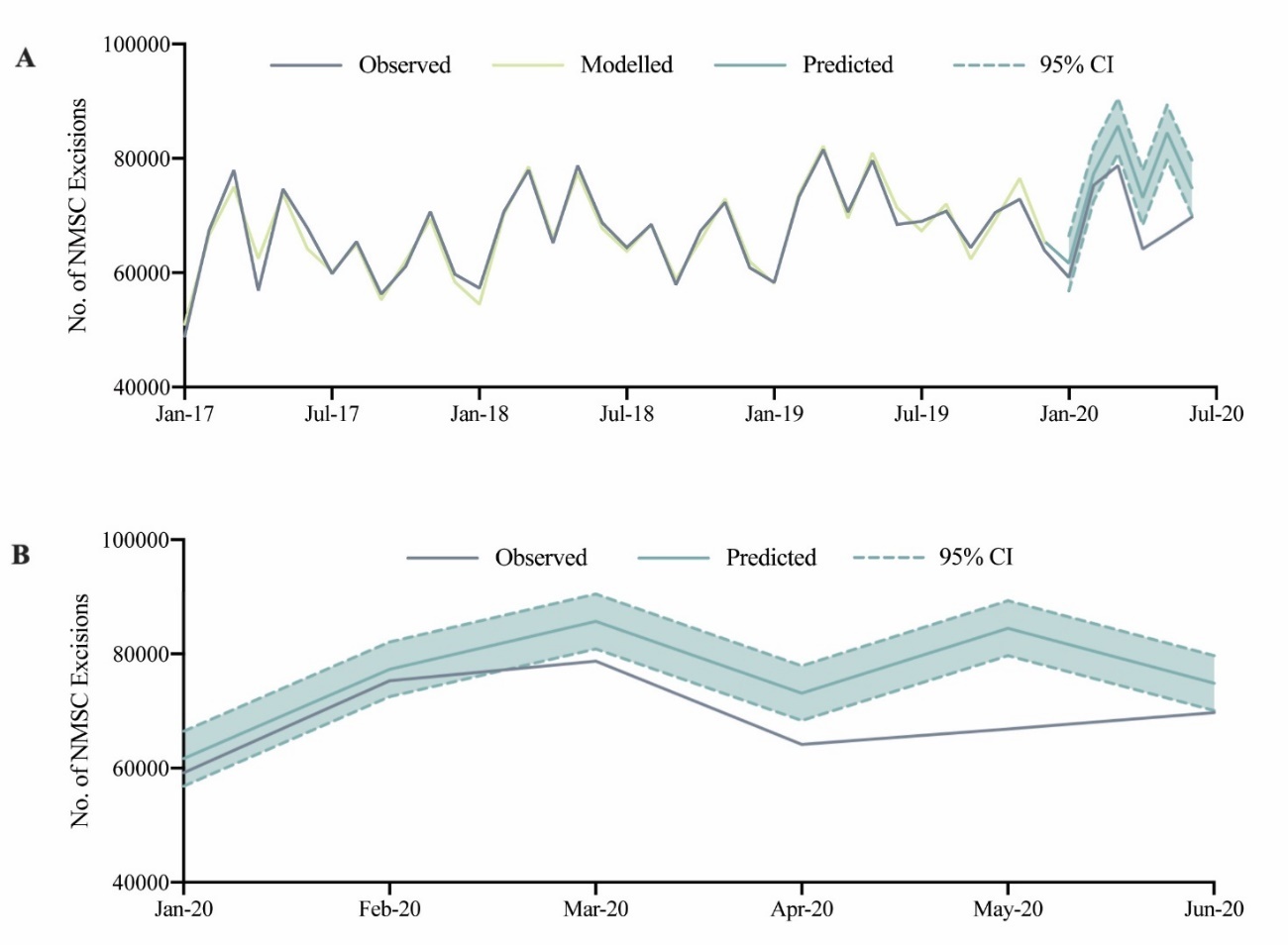
Excision of NMSC
A total of 413,920 NMSC excisions were performed between January 2020 and June 2020. There was no statistically significant difference between observed and predicted monthly NMSC excisions in January 2020 and February 2020. Compared to predicted, there was a statistically significant reduction in observed NSMC excisions performed in March 2020 (RD: –6943, –8.1%, 95% CI: –13.0% to –2.6%), April 2020 (RD: –8954, –12.2%, 95% CI: –17.7% to –6.1%), May 2020 (RD: –17,667, –20.9%, 95% CI: –25.2% to –16.1%) and June 2020 (RD: –5152, –6.9%, 95% CI: –12.5% to –0.5%) (Figure 2; Table 1).
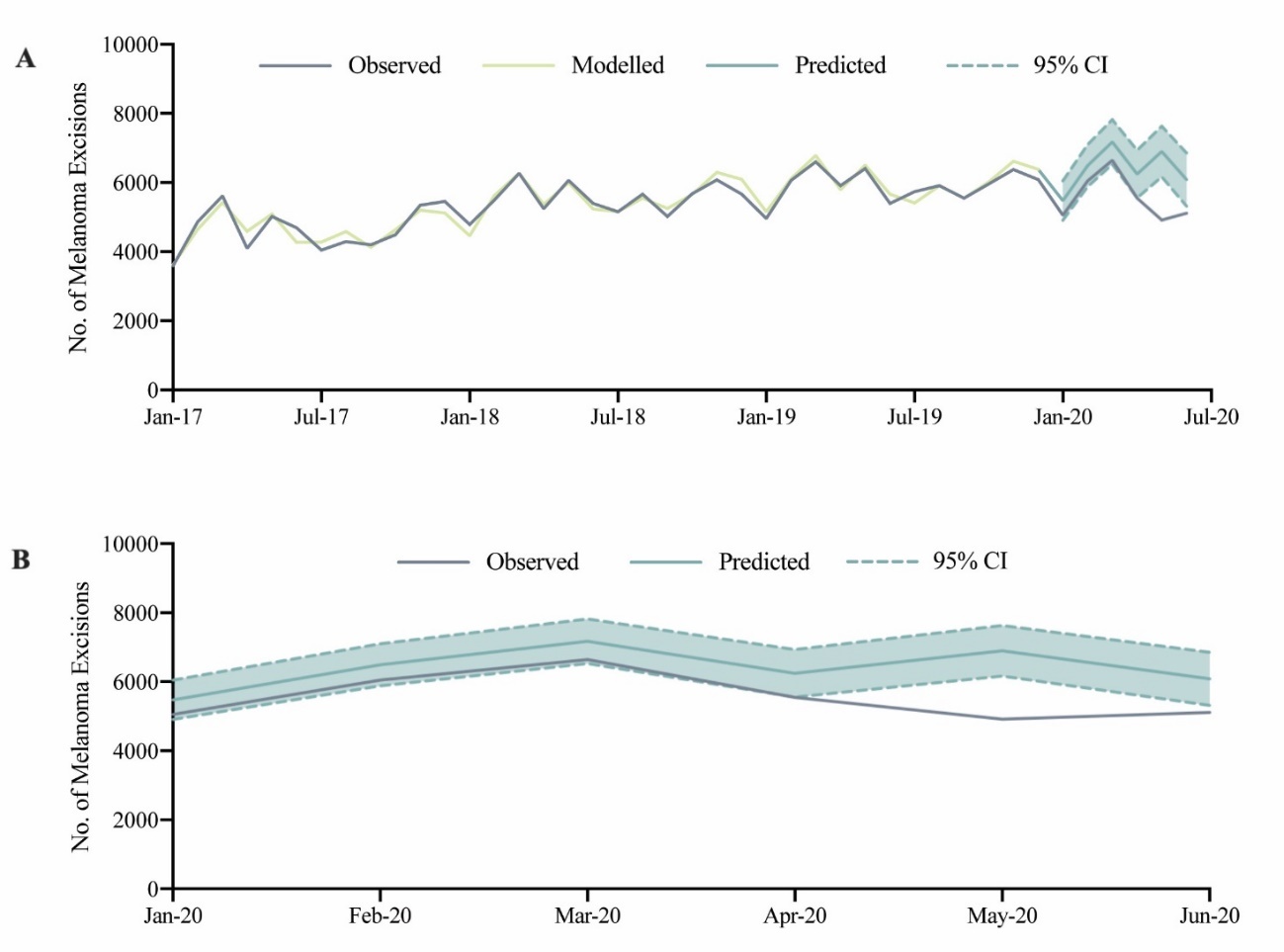
Excision of melanomas
A total of 33,323 melanoma excisions were performed between January 2020 and June 2020. There was no statistically significant difference between observed and predicted monthly melanoma excisions in January 2020, February 2020 and March 2020. Compared to predicted, there was a statistically significant reduction in observed melanoma excisions performed in April 2020 (RD: –695, –11.1%, 95% CI: –20.1% to –0.1%), May 2020 (RD: –1982, –28.7%, 95% CI: –35.5% to –20.3%), and June 2020 (RD: –973, –16.0%, 95% CI: –25.4% to –3.8%) (Figure 3; Table 1).
Discussion
The abrupt arrival and spread of the COVID-19 pandemic continues to have profound impacts on healthcare delivery worldwide.9–16 In Australia, the relatively low incidence of COVID-19 at that time is in part due to the stay-at-home orders and implementation of movement restrictions. Since the lockdown period between March and May 2020, resumption of elective surgery has been in an incremental and cautious manner.3,17 This is the first study to use interrupted time series modelling to quantify the impacts of the COVID-19 pandemic on the investigation and surgical excision of cutaneous malignancies in Australia.
With regards to NMSC, excisions were 8.1 per cent, 12.2 per cent and 20.9 lower than expected for March, April and May 2020 respectively. Interestingly, reduction in melanoma excisions was not observed until April 2020, but a greater reduction in excisions was noticed when compared with NMSC. The delayed decline in melanoma excision is likely an after effect of cutaneous biopsy reduction in the preceding month. It is likely that with less excisional biopsies, less diagnoses—and hence excisions—of melanomas would be evident in the following month. Single institution studies in Europe, UK and the US noticed similar trends of a reduction in the diagnosis, surveillance and management of skin cancers by approximately 27–54 per cent.10–16These findings not only aid with predicting how future waves of COVID-19 may affect skin cancer management but will also assist in the development of strategies in the recovery phase.
The observed reduction in skin cancer diagnosis and treatment during the first lockdown period is likely multifactorial. The first being the restrictions placed on the delivery of healthcare in Australia. This includes cancellation of non-category I elective surgery, reduction of procedures in general practice and a transition of outpatient services through telehealth. While both the Royal Australasian College of Surgeons and Australian Society of Plastic Surgeons deemed skin cancer surgery category I and urgent, there was encouragement to defer smaller lesions on the back, trunk and legs.18 This could have partly contributed to the reduction in NMSC excisions. Prioritising skin cancers also poses a dilemma as their aggressiveness is not always apparent in the first consultation.10,15
A recent Cancer Australia publication showed that approximately one-third of general practice and specialist services attendances between April and June 2020 were by means of telehealth.5 The majority of these services were delivered by telephone, with videoconferencing comprising of only 1–5 per cent of all consultations.5 While total consultations remained similar, expectedly there was an overall reduction in face-to-face consultations during the lockdown period.5,19 Tele-dermatology has been shown to be reliable in providing diagnoses of cutaneous lesions but it is reliant on clinical photography or videoconferencing.20 While telephone consultations allow for a detailed history, they do not allow for appreciation of appearance, cross-sectional anatomy and tactile feedback on mobility of skin lesions, unlike an in-person review.19 This higher portion of telephone consultations also inherently means the opportunity to incidentally detect or conduct a biopsy on new lesions is missed by primary care physicians. Both reasons highlight a shortcoming in current telehealth practices in managing skin cancer.
Another factor that could have contributed to overall reduction in biopsies and skin cancer excisions is patients’ reluctance to seek medical attention or burden the healthcare system, despite the governments’ and health bodies’ advice to continue regular medical checks. Other contributing factors include reduced regular skin cancer check attendances5 and nursing home lockdowns, minimising general practitioner reviews and the ability for elderly patients to attend hospital or outpatient clinics for surgery.
Skin cancer management has been negatively affected both in Australia and worldwide during the COVID-19 pandemic.10,11,13–16 This overall reduction in the diagnosis and treatment of skin cancer will inevitably lead to more advanced disease during the post-lockdown period. The detrimental consequences of lockdown on the management of cutaneous malignancy is still not fully realised.10,11,13–16 Ultimately, a need for increased activity in screening and managing skin cancer in the recovery phase of this pandemic will be required.
In planning for possible future COVID-19 waves, as seen in Victoria, particular measures need to be considered in the assessment and management of skin cancers in Australia. Firstly, patient education regarding recognising new lesions and still seeking medical help is important. Secondly, primary care and specialist clinics need to adopt visual aids such as clinical photography and videoconferencing in the use of telehealth to help with diagnosing skin cancer.19,20 Furthermore, clinicians need to have a low threshold for bringing patients in for a face-to-face consultation if diagnosis or assessment is difficult via telehealth.19 The Royal Australian College of General Practitioners provides guidelines for stratifying risk of skin cancer in patients.21 ‘See-and-treat’ skin cancer clinics, where patients are assessed by specialists and undergo definitive treatment in one setting, is also a possibility to minimise presentations to healthcare settings during pandemic times.
Limitations
The findings of this study should be interpreted in the context of several limitations. Firstly, MBS data do not represent all services performed in Australia. The MBS does not include services provided to inpatients at public hospitals. As such, this modelling did not include skin cancer patients who were still seen as public outpatients and treated in public hospitals during lockdown periods. Further, the MBS does not cover services qualifying for benefit under the Department of Veterans’ Affairs, WorkCover or the Transport Accident Commission. Despite this, these findings are still largely reflective of the overall impact of the COVID-19 pandemic on skin lesion services in Australia. Finally, the MBS item number 30071 pertains to all skin lesion biopsies not just cutaneous malignancies.
Conclusion
There was a significant reduction in total cutaneous malignancy excisions compared to predicted during the first wave of the COVID-19 pandemic in Australia. Explanations for this reduction include an overall decrease in total biopsies for cutaneous lesions as well as patients’ reluctance to seek medical attention. This observed reduction in skin cancer surgery has significant public health implications, highlighting the need for improved surveillance, diagnosis and management of cutaneous malignancies during the recovery phase of the pandemic.
Conflict of interest
The authors have no conflicts of interest to disclose.
Funding declaration
The authors received no financial support for the research, authorship and/or publication of this article.
Revised: 2021 Aug 30 AEST