Introduction
The applications of a simple technique are invaluable. I have used the boutonniere (button-hole) Elastoplast (adhesive dressing) splint technique (BEST) throughout my hand surgical career for simple and complicated injuries. With patients with fractures over 30 per cent of the articular surface of the distal interphalangeal joint (DIPJ) this technique avoids open intervention and open reduction internal fixation (ORIF). Unsuccessful conservative management where the treatment sometimes extends over eight months also can be successfully handled by this technique.
The accompanying audiovisual presentation is the basis of this teaching tool. Slides are supplemented by voiceover descriptions explaining the intricacies of this three-layered Elastoplast technique creating a boutonniere reduction position which needs to be reapplied with fresh Elastoplast weekly over a three week period. This produces an excellent outcome. I have included perspectives from patients in the video presentation where the details of the technique are discussed and the patient’s satisfaction is evident.
The technique
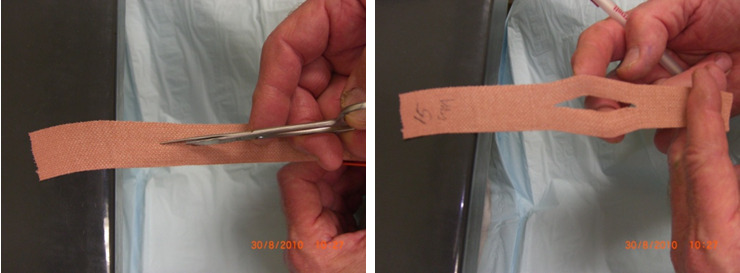
The technique consists of using 15 cm Elastoplast (Beiersdorf Australia, 4 Khartoum Rd, Macquarie Park, NSW, 2113, Australia) strips divided in the middle one third so the collateral strands along the divided segment can bridge over the proximal interphalangeal joint (PIPJ) (mimicking the position of the collateral ligaments of the PIPJ) (Figure 1a). This initially holds the flexed position while straddling the joint. The DIPJ is forced into 5–10° hyperextension. Because of the painful state of this reduction, long acting local anaesthetic gives pain relief in the first 24-hours using bupivacaine blockage. The Elastoplast is firmly applied to the pulp area of the distal phalanx, stabilising the hyperextension position. The split strands create the boutonniere shape at the PIPJ and the proximal strand of the Elastoplast is applied to the dorsum of the hand along the metacarpal. Sequential tightening of layers reinforces the alignment.
Figure 1b shows the hyperflexing of the PIPJ with the DIPJ in hyperextension in the first Elastoplast layer, thus creating the boutonniere reduction position. Layering the Elastoplast sequentially—layers one, two and three—at each stage creates a gradual increase into hyperextension of the DIPJ and a similar hyperflexion of the PIPJ.
Long-acting bupivacaine provides local digital analgesia, initially to help the manoeuvre and subsequently to help maintain the reduction during the first 24 hours which can be a painful period, which is its single drawback.
Week two
Re-splinting on a weekly basis helps to maintain the reduced position because of the laxity that develops in the Elastoplast strands. It is noteworthy how the symptoms have disappeared and the droop has not recurred at this early phase (Figure 1c).
Week three
Reapplying the splint ensures that the initial reduced position is maintained and locked into hyperextension and with any DIPJ fracture this ensures alignment in the articular surfaces without the need for open intervention and ORIF. The joint fracture heals ensuring repair of the avulsion of the extensor complex into anatomical normality achieving joint congruity.
Week four
From week four onwards the patient is under the care of a hand therapist with an orthoplast splint moulded to accommodate resolution of oedema and the improvement of functional range of activity. These orthoplast splints are removable for social reasons and ensure the avoidance of any inadvertent direct injury which may detract from the success, particularly when resting.
Acute injury
Figure 2a-c shows results of BEST treatment for an acute case with fracture of the DIPJ over 45 per cent caused by a soccer ball sporting injury. The 21-year-old man endured two weeks of pain using a Ferrule stack splint before undergoing treatment using this technique.
Chronic case
A 62-year-old woman suffered a separated extensor pollicis longus (EPL) tendon after a domestic cleaning episode. Following eight months of conservative management with splint the patient was still in pain and had been put on a waiting list for operative intervention (Figure 3a). Following two weeks of treatment using the BEST technique the patient showed improvement in the range movement and reported almost a total disappearance of pain (Figure 3b). By six weeks function is approaching normality and the patient is asymptomatic and extremely satisfied (Figure 3c). This has been achieved after three short dressing sessions.
Discussion
The BEST technique is a non-invasive procedure. The outcomes regarding range of movement have been universally acceptable and usually a four-week hand therapy practice, even six weeks, produces an excellent outcome without subluxation of the joint. It is pain free after the first 24 hours, with no extensor lag, no flexor deficit in the range of movement. After routine splinting, complete at six weeks, the patient does not warrant repeat X-rays as they universally say they ‘feel normal’. Complications like Elastoplast sensitivity have not been recorded in the number of cases done over the years and bony union occurs back to normal in all fracture cases performed.
Controversy surrounds the management of mallet fracture deformities because of the lack of consistency in optimal results. Savage and colleagues discuss type IIB fractures and recommend surgery.1 Wehbé and Schneider report difficulty with unreliable outcomes from surgical treatment, stating it offered no advantage over conservative treatment and had a greater rate of morbidity.2 King and colleagues report 24/59 (41%) of surgically treated mallet fractures developed postoperative complications with marginal skin necrosis, extensor lag, permanent nail deformities, transient infections along the K-wires and pull-out steel wires and osteomyelitis observed.3 No one has mentioned the umpteen attendances at outpatient clinics when conservative management may go on for months. The BEST technique, in my experience, is a five minute visit weekly over the four week period reapplying the Elastoplast.
The BEST technique is successful because it respects the three points governing mallet finger repair—enlocation, pain score and extensor lag. It offers a simple non-surgical solution for mallet deformities, with or without fractures, acute or chronic, in the young and the elderly, and avoidance of hospital admissions which means it has applications for regional services but best applied by a person experienced in hand surgery.
Patient consent
Patients/guardians have given informed consent to the publication of images and/or data.
Disclosure
The authors have no financial or commercial conflicts of interest to disclose for any of the products, devices, or drugs mentioned in this case series.
Funding declaration
The authors received no financial support for the research, authorship, and/or publication of this article.
Supplementary Material
Supplementary audiovisual material accompanies this text: https://youtu.be/KjaPcce-MxI



_on_presentation_(**b**)_week_six_(**c**)_week_14_showing_perfect_joint_alignmen.jpg)
__eight_months_of_failed_conservative_splint_management__(**b**)_two_weeks_of_treatmen.jpg)


_on_presentation_(**b**)_week_six_(**c**)_week_14_showing_perfect_joint_alignmen.jpg)
__eight_months_of_failed_conservative_splint_management__(**b**)_two_weeks_of_treatmen.jpg)