Introduction
Measurement of finger range of motion (ROM) is an important physical examination in hand surgery. The resulting measurements can be used to determine the presence or absence of dysfunction, guide interventions and assess treatment effectiveness.
The current method most frequently applied in hand surgery is a manual method using a universal goniometer (UG). Previous research has identified that visual assessment alone of hand position provides inaccurate measurements, although accuracy did increase with increased hand surgery experience.1 By contrast, goniometry measurements of the hand have shown superior inter- and intra-observer reliability than wire tracing2 and superior intra-observer reliability than composite finger flexion,3 which have lent support to their use over other methods. While use of a UG is a relatively easy and accurate technique, it has drawbacks in that the device is inconvenient to transport, not all clinicians possess one and a patient cannot conduct their own measurements at home. Furthermore, a recent systematic review concluded a limited level of evidence to support acceptable reliability in the measurement method of hand goniometers.4
‘Smartphones’ use internal accelerometers that serve as position sensors for phone functionality and to interact with map functions and other positional-dependent applications. These hand-held devices present a powerful potential tool for both clinician and patient—not only do they contain high- quality tri-axial accelerometers but also significant computing power, storage space and internal connectivity. Smartphone apps may be a convenient alternative to the traditional UG for clinicians and patients. A recent audit of plastic and reconstructive surgical trainees in Australia and New Zealand indicated that only one trainee owned and carried a goniometer. Not only are they convenient, smartphone goniometer applications (smartphone apps) have been shown to be reasonably accurate and reliable for angle measurements.5
Several studies have confirmed the validity and reliability of smartphone apps in other joints, including the forearm/wrist,6–10 shoulder,11 knee,12–14 ankle15 and foot.16 The ability for the patient to self-measure with these electronic applications was a frequently noted benefit. A recently published article17 assessed smartphone apps use for hand measurements and found favourable reliability and measurement time relative to conventional goniometers. This study sought to further assess accuracy of smartphone apps compared to a traditional UG in ROM assessment of healthy and diseased hands.
Methods
Participants were selected through a tertiary hospital hand surgery clinic over a two-month period. Patients were over 18 years of age. Exclusion criteria were patients presenting with pain, infected joints of the hand and open injuries requiring surgery within 48 hours or within 48 hours of the postoperative period, exhibiting gross swelling of the hand, suffering from any condition that may restrict shoulder/arm movement, or with a recent history of hand trauma or fracture. Healthy volunteers were also selected through the clinic, mostly being friends or relatives of presenting patients. The middle and little fingers were studied. All patients were right-hand dominant, although this was only by coincidence. Measurements were made at the metacarpophalangeal joint (MCPJ), proximal interphalangeal joint (PIPJ) and distal interphalangeal joint (DIPJ) for both flexion and extension.
Ethics approval for this study was granted as low/negligible risk research [LNR/AU/6/E8DF16]. On arrival, each participant was given an information sheet and informed consent form, which was signed by participants before commencing.
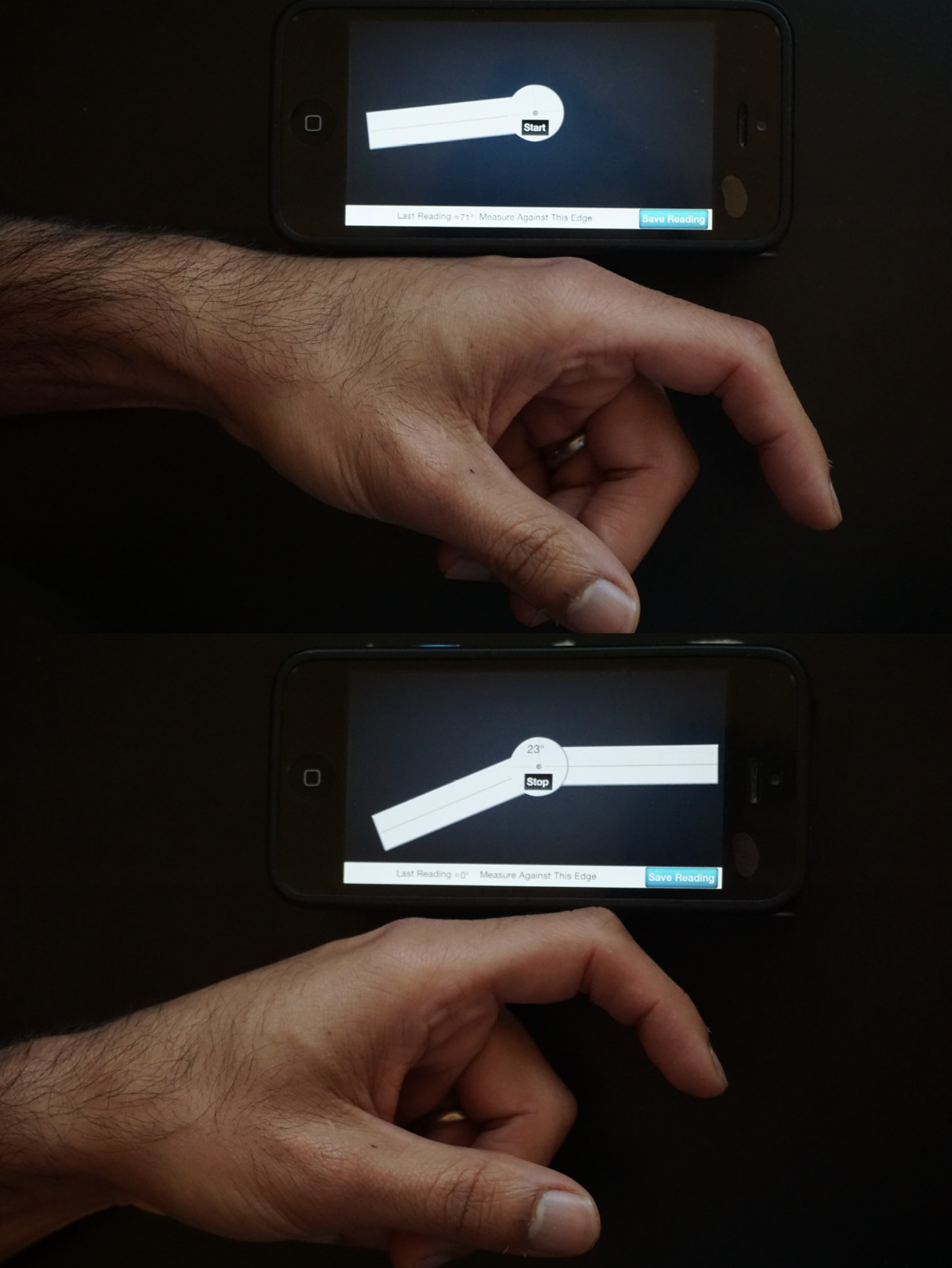
A single UG, with a plastic 180° goniometer face and one-inch movable arm, and an Apple iPhone (Apple Park Way, Cupertino, California, 95014, United States) with Goniometer Pro® (5fuf5 Co, 64 Haines Dr, Bloomfield, New Jersey, 07003, United States), accelerometer-based application installed, were used for all measurements (Figure 1). One evaluator conducted finger ROM measurements using both goniometers twice, using the average value of both measurements to reduce measurement errors. Another independent evaluator repeated the measurements using the smartphone app in a separate room. To reduce the risk of bias, both evaluators were blinded from the scores obtained while using both goniometers with an assistant recording their measurements. Recording was documented using a standardised proforma based upon the Procedural guidelines from the American Society of Hand Therapists (ASHT) (Appendix 1).
Training
Guidelines for measuring finger ROM were provided to evaluators two weeks prior to the day of assessment. These guidelines included position for measurements, goniometer placement and instructions for the patient. All evaluators had at least six months experience in the management of hand patients prior to this study. A follow-up group training session was also conducted two days before the start of assessment, which provided an opportunity for the evaluators to practice and discuss the process with one another.
Landmarks
So that the evaluator could not read the measured angle, the on-screen goniometer and the angle were covered, as was one side of the UG face. The assistant could lift the cover on the phone to reveal the angle and could read the angle on the opposite side of the UG.
Measurements were taken from the dorsal midline of the metacarpal or the phalanges. For flexion of the digits, the participants’ elbows were placed on the table, wrist in 30° extension (neutral position), and the patient was asked to make a full fist (Figure 2). All instructions were standardised with a scripted proforma for the evaluators to use.
‘Make a full fist as best as you can and squeeze into your palm.’
‘Squeeze as tight as you can but not causing you pain of more than 2 out of 10 (10 being the most pain experienced).’
Measurements of the MCPJ and PIPJ were then taken. For the DIPJ, the patient was asked to make a ‘hook fist’ by extending the MCPJs as much as possible.
‘Keep your fingers as tight as you can but now slowly straighten your knuckles, and only your knuckles.’
For extension, the patient’s wrist was now placed at 0° and they were told to straighten their fingers as much as possible. Measurements were again taken at the MCPJ, PIPJ and DIPJ.
‘Keeping your wrist still, slowly straighten your fingers as best as you can at every joint.’
Statistical methods
The sample size was calculated using the formula for reliability studies based on confidence intervals (CIs) described by Steiner and Norman18 with the number of instruments (k) equal to 2, the CI around r (reliability coefficient) of 0.05 and an estimated r of 0.95.
Paired T-test analysis was used to compare the observer’s measurements using a UG and smartphone app for each joint, as well as the average measures for a UG and smartphone app to determine any significant differences.
Results
Twenty patients were recruited (10 male, 10 female; mean age 32 years). Of these, 13 were healthy volunteers and seven patients had previous hand pathology (three proximal phalangeal fractures, one bony mallet finger, one subtotal wrist amputation, one subtotal mid-forearm amputation, one MCPJ dislocation). All were right-hand dominant by chance.
Smartphone app
There were no significant differences in the measurements obtained by the smartphone app of the two observers (Table 1). The largest variation was for right middle finger DIPJ extension; however, the mean difference here was only 2.1° and this was not significant (p = 0.13).
Universal goniometer
There was a significant difference between observers using the UG for little finger PIPJ flexion. Observer 1 measured an average 2.5° less than Observer 2 (p = 0.04). No other measurement variables showed significant difference between observers (Table 2).
Device comparison—universal goniometer versus smartphone app
Comparison between average measurements using the UG and smartphone app found six significant results, four of which were highly significant (p ≤ 0.005) (Table 3). However, none of these differences were greater than 5°. The joint with the largest difference (4.6°) was the middle finger MCPJ extension.
Discussion
Goniometer usage has previously been advocated in hand examination as the preferred method for assessment of joint angles.2 Such examination aids are relevant given the documented inaccuracy of purely visual estimation of finger angles. These angles were inaccurately judged by hand surgeons and therapists by approximately 25 per cent on average in the study by Rose.1 Another study19 reported neither visual assessment nor goniometers had shown high levels of accuracy in hand measurements relative to radiographic measurements. A further systematic review highlighted the low level of evidence to support the reliability of goniometer measurements.4
There is thus a need to ascertain a reliable and convenient method of assessing finger ROM. Early work in this field20 noted the particularly complicated nature of measuring hand joints, including the large number of joints in a small area, short motion axis and the difficulty of stabilising forces affecting the multiple joints.
Smartphone photography goniometry has previously been found to be a reliable tool for assessing finger ROM compared with manual goniometry, including when photographs were taken by patients’ family or friends.21 Previous work using smartphone apps to assess angles on irregularly shaped pyramids identified 14 apps (10 Apple iPhone; 4 Google Play) that were reliable and valid with < 3° deviation compared to a traditional UG.5 Two sub-groups of applications existed: those based on measurements from smartphone photographs and those making use of the device’s built-in accelerometer. There were no significant differences in measurements between these two groups.5 The application used in this project (Goniometer Pro®, an accelerometer-based application) was one of these validated applications.
Most literature supports a 5° threshold as an acceptable level of measurement error for hand goniometric measurements.22 Using a traditional Rolyan® (Patterson Medical Supply, 1000 Remington Blvd, Suite 210, Bolingbrook, Illinois, 60440-5117, United States) goniometer, a report by Ellis and colleagues3 found that 95 per cent of the time, repeated intra-rater goniometric measures were within 4–5° of each other; inter-rater goniometric measurements were within 7–9°. Their study found goniometry measurements exhibited superior intra-rater reliability compared to assessment of composite finger flexion, with equal inter-rater reliability between the two methods.3 Subsequent research by Lewis and colleagues,23 also using a Rolyan finger goniometer, corroborated these findings, and found higher intra-rater reliability (measurements differing by > 4° in < 5% of cases) than inter-rater reliability (measurements exceeding 5° in > 80%). However, using experienced evaluators following standardised guidelines, Engstrand and colleagues’ study22 found high to very high inter-rater reliability for goniometer measurements of finger ROM in Dupuytren’s disease.
From these studies, it is accepted that traditional goniometry measurements have a good intra-rater reliability, and reasonable inter-rater reliability (perhaps depending on the heterogeneity of experience and technique in the evaluators employed). In line with this, there were no clinically significant differences within or between the traditional UG and smartphone app in our study, as no measurement differences were > 5°. These findings confirm that the smartphone goniometer application measurements are as reliable as traditional goniometry techniques.
A recent article by Miyake and colleagues17 explored ROM measurements using both a traditional protractor-based goniometer and a smartphone goniometer application across 1007 finger joints. The authors found that the smartphone application had a high intra-class correlation coefficient (0.927) and its measurements took an average 49 per cent less time to perform.17 Smartphone-based measurements thus exhibited the same reliability but took half the time compared to a traditional goniometer. Their study, using an Android application that the research team had developed themselves (and is currently only available through Google Play in Japan) was the first to specifically assess finger ROM using a smartphone goniometer. Our study is the first to assess finger ROM using a validated smartphone app with broader community availability. This allows for patients’ own involvement in using the smartphone app as part of their therapy and follow-up. We envisage that future patients will download the application, with a clinician then able to use the application on the patient’s phone to measure relevant finger angles. These results could then be safely and privately stored on the patient’s own smartphone for future reference, facilitating continuity of care across clinicians and services.
Limitations
A limitation of this study is the modest number of patients assessed, with further recruitment needed to improve the study’s power. Strengths of the study include its assessment of finger ROM measurements across a broad range of pathologies (rather than limiting to Dupuytren’s disease, which is common in the literature). The smartphone app used also has widespread commercial availability which facilitates broad clinical and community uptake and use.
The practical advantages of smartphone applications (such as a goniometer) over traditional devices are clear—particularly with their portability and the ubiquitous presence of smartphones in our personal and professional lives. Few surgeons reliably carry a handheld goniometer, yet nearly all of them have a smartphone, as do a vast majority of our patients. These electronic devices could provide easier recording and tracking of measurement data to assess patient progress and for research, and would provide continuity of care across different clinicians and hospital services (for example, surgical clinic and hand therapy clinic). Potential issues include confidentiality of the data, as well as the cleanliness of the device. This could be limited by providing independent hospital-owned and operated electronic devices in hand clinics, or by the patient downloading the application and using their own device, as mentioned above.
Further to the advantages within the hospital setting, wider adoption of smartphone goniometer applications would facilitate patients self-measuring at home to assess their own progress. This certainly has practical utility for the follow-up of patients, as it may obviate the requirement for frequent reviews in-person in the clinic. In a country like Australia where patients may travel large distances to attend specialist hand clinics (traditionally focused in sub-specialty centres in the major cities), this could be convenient for patients and cost effective for the health system with reduced travel subsidies required. Other literature has also previously advocated the advantages of smartphone and photography-based goniometry applications in telemedicine.24
Conflicts of interest
The authors have no conflicts of interest to disclose.
Funding declaration
The authors received no financial support for the research, authorship and/or publication of this article.