Introduction
The fibular free flap is widely used for reconstruction of oromandibular and oromaxillary surgical defects in patients with advanced head and neck cancers. Its long pedicle length, in combination with its periosteal blood supply, which allows for multiple osteotomies to be performed, makes it particularly well suited to reconstruction of midfacial defects.
The fibular free flap pedicle often includes adjacent periosteal tissue from the proximal fibula. However, vascularised periosteum has known osteogenic potential. Delayed ossification of the vascular free flap pedicle has been widely reported in the literature,1 and can potentially cause pain and trismus.2,3
Management of the ossified vascular pedicle is dependent on the patient’s symptoms. Most authors advocate removal of the heterotopic ossification in symptomatic patients. However, the practicalities of this can be challenging in patients with severe trismus limiting access to the pedicle. We report our experience in managing a difficult case of symptomatic pedicle ossification.
Case
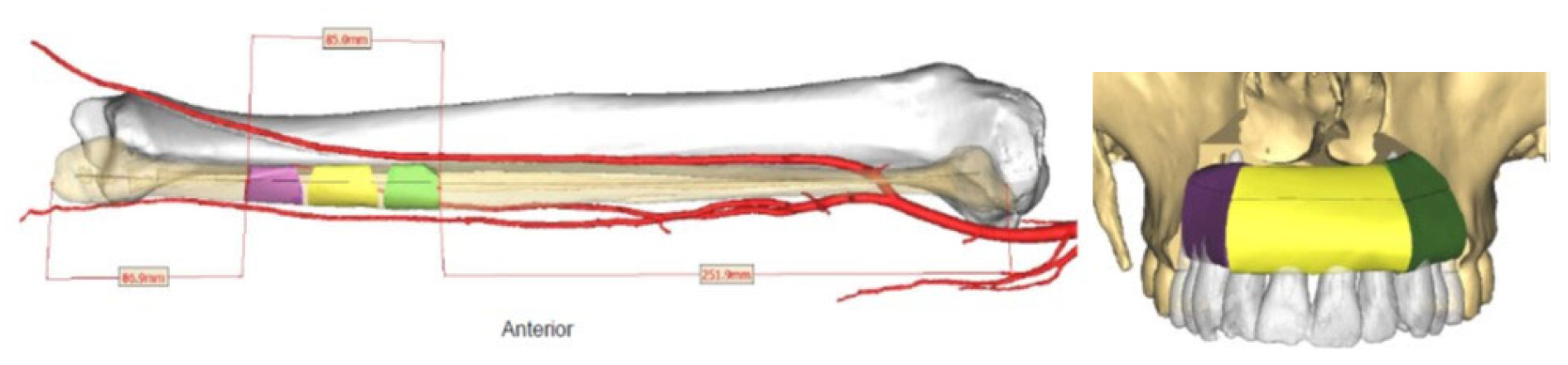
The patient is a 47-year-old man who was diagnosed with T4aN0M0 oral squamous cell carcinoma of the anterior maxillary alveolus. He underwent bilateral infrastructure maxillectomy, bilateral neck dissection and microvascular fibular free flap reconstruction. The vascular pedicle ran from the left side of the maxillectomy defect along the pterygomandibular raphae, medial to the mandible, and was anastomosed to the facial artery and common facial vein (Figure 1). Surgery was followed by postoperative adjuvant radiotherapy to a dose of 60 Gy. The patient recovered well and regained excellent oral function.
Eight months postoperatively, the patient began to develop progressive trismus. Clinical examination revealed a tight mucosal band extending along the pterygomandibular raphae, at the site of the buried vascular pedicle. There was no clinical suspicion of recurrence. Cross-sectional imaging showed heterotopic ossification along the length of the pedicle (Figure 2).
Conservative management in the form of trismus physiotherapy exercises was trialled but was unsuccessful. A decision was made to surgically debride the heterotopic ossification via a transoral approach. Surgical access was limited by trismus but, ultimately, good access was achieved with the use of a Dingman oral retractor (Figure 3). The ossified pedicle was divided in entirety. The peroneal artery was heavily calcified and this was divided as part of the pedicle. The ends of the artery did not bleed following division. Attempts were made to ligate the pedicle but this was challenging due to the ossified vessels, so diathermy was used instead. Following pedicle division, the heterotopic bone was removed and there was an immediate improvement in mouth opening from approximately 10 mm to 30 mm. Haemostasis was confirmed and the overlying mucosa was closed with local flap coverage.
Eight days postoperatively, the patient presented via the emergency department with sudden onset heavy oral bleeding necessitating urgent surgical exploration. The bleeding was found to be originating from the proximal aspect of the divided arterial pedicle. Control of the pedicle was difficult; surgical clips and ties were ineffective as they were unable to compress the ossified arterial wall, and the pre-existing trismus limited access to the proximal vessel. Ultimately, hemostasis was achieved with a combination of electrocautery and proximally placed surgical clips.
The patient recovered well from the procedure without the need for a blood transfusion. He was monitored carefully but had no further bleeding episodes. His trismus continued to improve with physiotherapy exercises. He is now 18 months post his original surgical date and remains disease free with excellent mouth opening. At the time of writing, the free flap remains viable. Bony union at the osteotomy sites was confirmed prior to the pedicle revision surgery and those sites remain intact currently. The patient remains at risk of long-term bony breakdown due to chronic flap ischaemia, particularly in the post-radiotherapy setting.
Discussion
Ossification of fibular free flap pedicles within the head and neck region has been observed in 20 to 50 per cent of patients.1,4,5 It is more common in maxillary reconstructions.4 Although asymptomatic in the majority of patients, cases resulting in pain and trismus often require intervention. Subperiosteal dissection of the pedicle with removal of muscle cuff and periosteum has been proposed to reduce the risk of heterotopic ossification;6 however, this does not entirely prevent the phenomenon.7
Alternative osseous reconstructive options, including scapular and radial forearm flaps, have not demonstrated the same propensity for heterotopic ossification, likely due to the absence of vascularised periosteum along the pedicle.1 However, these flaps are limited by shorter pedicle length, higher donor site morbidity and lower bone height, which make them less well suited to head and neck reconstruction, most notably when dental rehabilitation is planned. Pedicle length is of particular concern in reconstruction of maxillary defects, where adequate length is required to enable anastomosis within the neck.
Previous reports in the literature describe removal of heterotopic bone from the vascular pedicle. Ideally, this would be performed while leaving the underlying vascular pedicle intact. However, dissection of the ossified tissue away from the vessels without disruption of the vascular integrity can be extremely challenging. This is particularly true in cases where surgical access is difficult, such as this patient in whom the pedicle could only be accessed transorally. Mandibular osteotomy could be considered to improve access in patients with complete trismus. However, this has the potential to worsen oral morbidity (particularly in the irradiated patient) and therefore we do not advocate its routine use in this setting. In our experience, we prefer the combined use of the Dingman oral retractor and rigid endoscopes to access the posterior oral cavity in patients with trismus.
The delayed haemorrhage of the ossified vascular pedicle was an unexpected complication. To our knowledge, this has not been previously reported. It highlights the need to achieve proximal control of the pedicle if the integrity of the vessels is to be disrupted. In our case, this could have been achieved via concurrent transcervical ligation of the facial vessels at the time of pedicle division. We would recommend this be considered as a routine part of the procedure in future cases, to avoid delayed haemorrhagic complications.
In the case of acute haemorrhage, control could also be achieved through radiologically guided embolisation of the vessel. This has certain advantages over surgical control, including precise identification of the bleeding vessel, avoiding repeated disruption to the surgical bed and avoiding access issues in the case of trismus. However, identification of the culprit vessel can be challenging when the bleeding has temporarily ceased—this is particularly the case following free flap anastomosis, where the normal vascular anatomy is disrupted. In these cases, discussion between the surgical and radiology teams is helpful to identify the most likely source of bleeding. We considered radiologically guided embolisation in our case but, ultimately, we elected to manage the bleeding surgically because access to theatre was more emergently available at our institution.
Pedicle division of a bony flap at eight months postoperatively confers a risk of flap ischaemia. This can result in non-union of osteotomies, loss of bone stock or complete loss of the free flap. It also increases the risk of complications with future placement of osseointegrated dental implants. It is our standard practice to wait at least six months, and ideally 12 months, before considering pedicle division. This allows time for collateral circulation to develop. In our case, the rapid development of trismus increased the urgency of pedicle division. We were reassured by the presence of bony union at the osteotomy points on preoperative imaging. Thankfully the flap remained viable. Nevertheless, we recommend that the timing of pedicle division be carefully balanced against the risks of flap devascularisation in these cases.
Conclusion
Pedicle ossification is relatively common in fibular free flap reconstruction of the head and neck region. This case illustrates some of the pitfalls to consider when managing the condition, and highlights the necessity of achieving good surgical access and proximal vascular control.
Patient consent
Patients/guardians have given informed consent to the publication of images and/or data.
Conflicts of interest
The authors have no conflicts of interest to disclose.
Funding declaration
The authors received no financial support for the research, authorship and/or publication of this case report.
Revised: January 12, 2022 AEST

_axial_computed_tomography_scan_(b)_coronal_computed_tomography_scan__both_(a)_and_(b)_sho.jpg)

_axial_computed_tomography_scan_(b)_coronal_computed_tomography_scan__both_(a)_and_(b)_sho.jpg)
