Background
The median artery is the embryonic arterial axis of the upper limb that usually atrophies in the second month of intrauterine development, after which supply to the upper limb is by the radial and ulnar arteries.1 In some cases, the median artery does not regress and persists after birth, accompanying the median nerve as a persistent median artery (PMA). A PMA presents in two forms based on its vascular territory: an antebrachial type whereby it supplies the median nerve but does not reach the hand, and a palmar type that provides arterial supply to the hand.2 The antebrachial PMA occurs more commonly (> 50%) and is slender with a short course arising from the anterior interosseus artery that terminates before reaching the wrist. The palmar type of PMA (20%) is larger, with a longer course, and is more liable to result in complications. Anatomical studies have demonstrated that PMA occurs more frequently on the left side than on the right, is more commonly unilateral and affects females more than males (1.3:1).1,3
Symptomatic PMA thrombosis leading to compression of the median nerve at the wrist has been historically treated by either anticoagulation therapy and/or excision of the thrombosed artery in combination with carpal tunnel decompression.4
The COVID-19 vaccine has been developed using two technologies: viral vectors and mRNA. Both types of vaccine have been linked to several rare and serious adverse effects, notably thrombosis and vaccine-induced thrombotic thrombocytopenia.5 To date, there have been no reported cases of COVID-19 vaccine-related median artery thrombosis.
A 20-year-old right-hand dominant woman developed acute carpal tunnel syndrome two days following her first Pfizer COVID-19 vaccination. She developed acute pain and paraesthesia radiating from her right wrist to her thenar eminence, thumb, index and long fingers. There was no personal or family history of coagulopathy, she was a non- smoker and had no underlying medical conditions. She was otherwise well with no systemic reaction to the vaccine. Her medications consisted of the oral contraceptive pill. She initially presented to her general practitioner who organised an outpatient ultrasound scan identifying an occlusive thrombus in a persistent median artery. The GP commenced her on 100 mg aspirin daily and referred her to the plastic and reconstructive surgery department. On examination her hand was well perfused and had no thenar wasting. She had a positive Tinel’s and Phalen’s sign at the wrist, and Allen’s test indicated patent ulnar and radial arterial flow. She was reviewed by the haematology and vascular medicine teams who ceased her aspirin and did not recommend thrombolysis or anticoagulation. Coagulation screening and her thrombocyte count were normal.
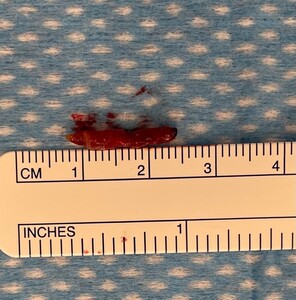
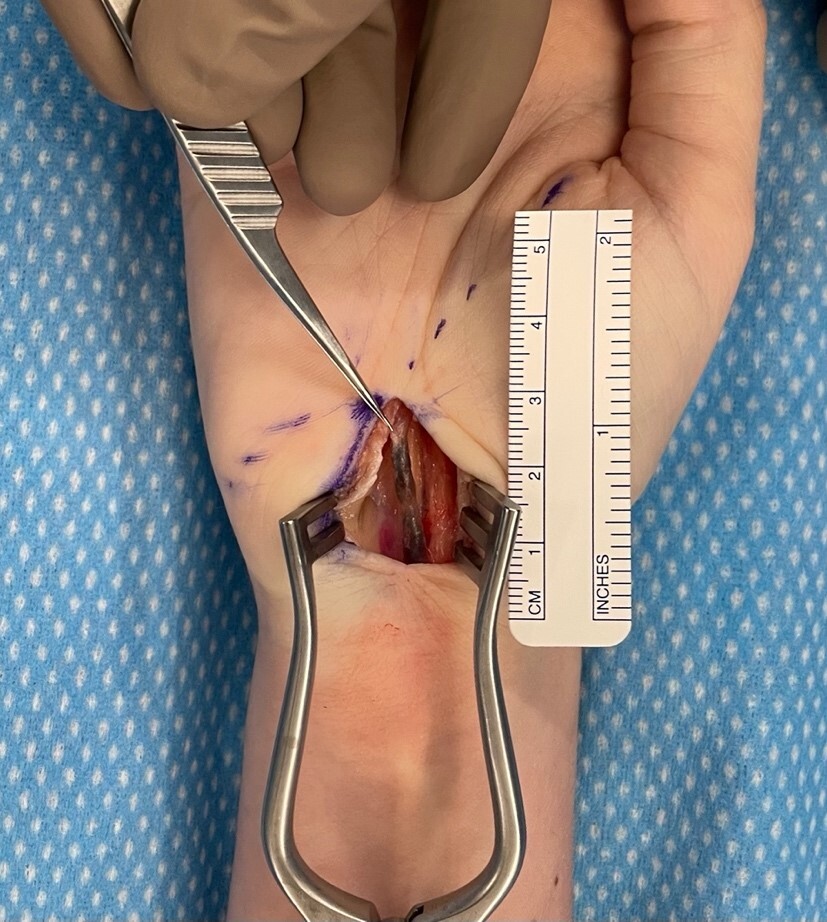
She underwent an open carpal tunnel decompression and excision of the thrombosed PMA (see figures 1 and 2). She had complete resolution of her carpal tunnel symptoms after surgery and no further thrombotic events.
Discussion
This case describes a rare complication of the uncommon anatomical variant of PMA, namely, thrombosis and acute compression of the median nerve at the level of the wrist, leading to secondary carpal tunnel syndrome. Receiving the COVID-19 vaccination may have been a contributary prothrombotic trigger for this patient.
The carpal tunnel is a fibro-osseous passageway in the wrist bounded by the carpal bones and transverse carpal ligament. The tunnel houses the median nerve and the flexor tendons to the fingers and thumb. Carpal tunnel syndrome occurs due to narrowing or swelling within the carpal tunnel, putting pressure on the median nerve and compromising its blood supply. This pressure results in paraesthesia, pain and progressive atrophy of muscles of the thenar eminence. Most commonly, the cause of the swelling is idiopathic; however, mass effect from ganglion cysts or less frequently lipoma has been reported.6 Carpal tunnel syndrome is the most common entrapment neuropathy, compressing the median nerve within the tunnel. This patient had a palmar type PMA that had segmental thrombosis within the carpal tunnel which led to median nerve compression and acute secondary carpal tunnel syndrome. This diagnosis is supported by the relief of symptoms after carpal tunnel decompression and excision of the thrombosed segment of the PMA.
Sterling Bunnell, considered by some to be the founding father of hand surgery, was the first to describe PMA as a cause of secondary carpal tunnel syndrome due to pressure from the thrombosed artery rather than ischaemia.4,7 This was also supported by the fact that the PMA and median nerve share a common sheath. Causes of median artery thrombosis have been documented to include taking the hormonal contraceptive pill, infection and repetitive placement of the wrist in unusual positions. This patient’s only known risk for thrombosis included taking the oral hormonal contraceptive pill, having a palmar type PMA and having recently had the COVID-19 vaccination.
The COVID-19 vaccination has been linked to prothrombotic events and may have been the inciting risk factor for development of a thrombosis in this patient given the close timeline from vaccination to onset and progression of symptoms. Although this patient did not meet the criteria for vaccine-induced thrombotic thrombocytopenia, thrombosis alone is a well-documented atypical adverse effect secondary to inoculation with the COVID-19 vaccine. The increased risk of thrombosis appears to be due to a soluble adenoviral protein spike variant causing endothelial inflammation and binding to endothelial cells expressing certain receptor genes (ACE2). Venous thrombosis occurs more commonly than arterial thrombosis; however, peripheral artery thrombosis leading to acute limb ischaemia has been documented. Women of child-bearing age are most at risk of developing the procoagulant side effects of the COVID-19 vaccine.5
Conclusion
This unique case demonstrates a patient who developed PMA thrombosis and acute compression on the median nerve at the wrist leading to secondary carpal tunnel syndrome. Her risk factors included palmar-type PMA, recent COVID-19 vaccination and oral contraception. The vaccination as the triggering event for this patient to develop thrombosis cannot be ruled out.
Patient consent
Patients/guardians have given informed consent to the publication of images and/or data.
Conflict of interest
The authors have no conflicts of interest to disclose.
Funding declaration
The authors received no financial support for the research, authorship and/or publication of this article.
Revised: September 13, 2022; September 20, 2022 AEST