Introduction
Cleft lip repair is a technically challenging operation that requires an appreciation of the complex anatomy of the lip and nose. Its mastery lies at the end of a steep learning curve and demands a cultivated eye for the nuances that set each case apart from the next.1,2 Establishing operative experience for surgical trainees is imperative in cultivating surgical skills. The diminished opportunities for trainees to perform cleft lip and palate repairs may be partly attributed to limited accessibility to paediatric units, the relatively low caseload volume and the steep learning curve associated with the procedure. This unmet need has been recognised, but has not yet been addressed in Australia.
Simulation training, either digital, virtual or 3D, has been shown to be effective in improving the transfer of skills.3–6 The appeal and utility of a simulator-based module are further realised in the context of a procedure that presents itself only to trainees undertaking their paediatric term. Given the intricacies of the surgery and the importance of patient safety and satisfactory long-term outcomes, opportunities to carry out the technical aspects of a cleft lip repair tend to be restricted.1,2,4,5
In the context of the ongoing COVID-19 pandemic, barriers to surgical training are further exacerbated by the cancellation of elective procedures, reassignment of surgical staff to higher acuity departments and limitations on the number of personnel in theatre. A potential by-product of this unique surgical climate is the development of innovative educational techniques. One such tool recently incorporated into our surgical practice is a microvideoscope system that projects magnified 3D images of the operating field onto dedicated screens in the theatre or elsewhere in the hospital for observers. This facilitates demonstrations of surgical technique and avenues of teaching that were previously limited given the confines of the operative field.7 Embracing these novel learning tools ensures the ongoing cultivation of skills and maintenance of high surgical training standards.
There is evidence for the role of simulations to bolster ongoing skill acquisition across various surgical specialities.5,6 The ability to incorporate knowledge, complex cognitive steps and technical skills in a risk-free environment via simulations may increase competency and confidence among participants. There is growing recognition among the plastic surgery community that simulations should be considered not merely as an adjunct to training, but as a vital medium to facilitate further learning and surgical excellence.2,4–6
The Australian plastic and reconstructive surgery curriculum guidelines highlight the expectation that trainees carry out elements of a cleft lip repair under ‘direct guidance’ during the early (surgical education and training (SET) 1–2) to mid-training years (SET 3–4). Senior trainees (SET 5) are expected to perform the procedure under ‘monitoring and supervision’. An evaluation of 11 Western Australian trainees who attended the inaugural cleft lip simulation workshop at the Perth Children’s Hospital demonstrated that of the early (n = 6) to mid (n = 4) level trainees, only one mid-level trainee had performed cleft lip repairs under supervision as the primary operator. The single senior trainee who attended the workshop had also completed the procedure under supervision.
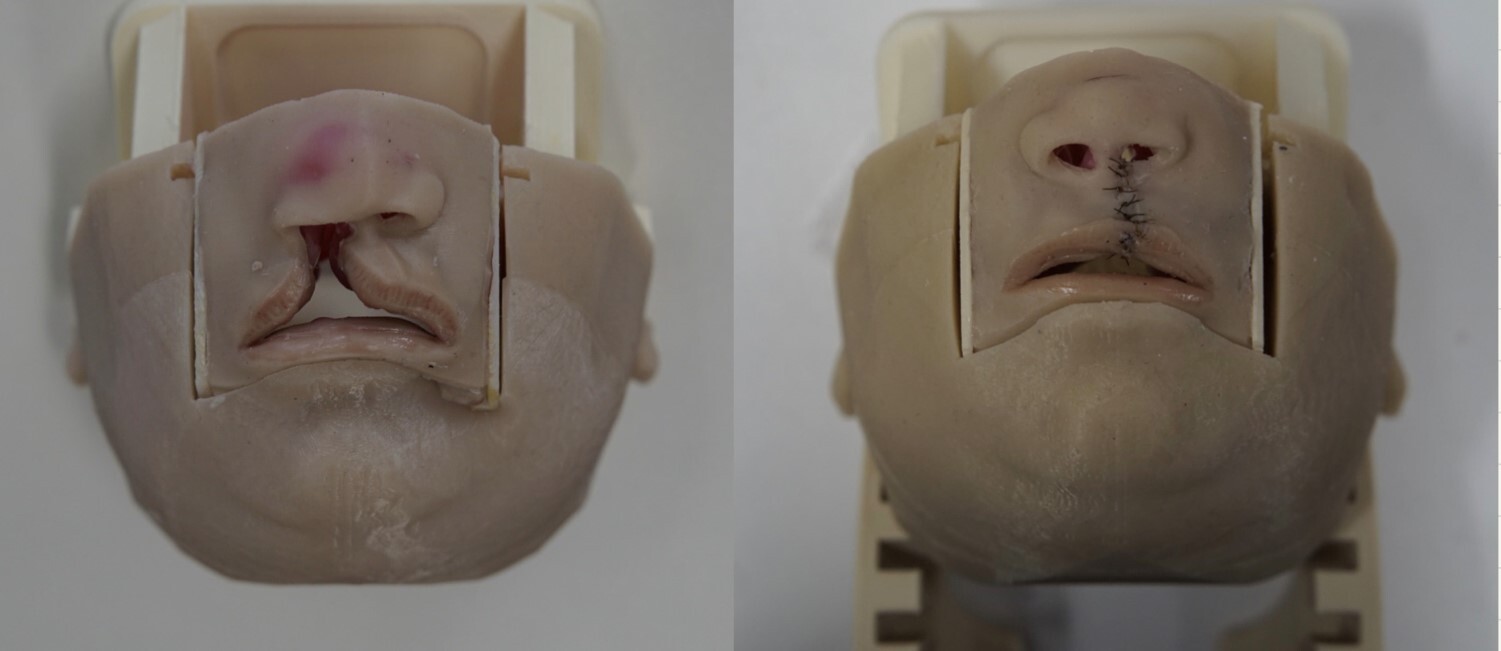
At present, a variety of digital and 3D cleft lip simulators are available for educational purposes.1,2,5,8 The Simulare Medical (Smile Train Inc, New York, New York, USA) unilateral cleft lip simulator is a 3D high-fidelity model that comprises multilayered, anatomically accurate bony and soft tissue structures. The pliability and material properties of the model were designed to match those of their respective anatomical components, allowing for realistic tactile feedback and tissue feel while carrying out the repair. (Figure 1).
Aim
This study assesses the perceived confidence levels of plastic surgical trainees to carry out a cleft lip repair before and after didactic teaching and a practical session with the Simulare models.
Material and methods
The workshop was hosted in November 2019 at the Perth Children’s Hospital. Eleven out of 12 of the state’s plastic surgery trainees participated in the session. Three-dimensional high-fidelity Simulare simulation models were purchased for the workshop. The kits contained surgical instruments, training videos and standardised questionnaires. Participants watched a video depicting the markings, incisions and repair of a unilateral cleft lip. Two senior cleft surgeons provided additional commentary and teaching points throughout the workshop. (Figure 2).
Before the workshop, the participants completed an online survey to assess their level of training, prior surgical experience and confidence levels with regards to performing a cleft lip repair. The confidence-rating scale, provided by Simulare, was comprised of eight questions on a Likert scale of 1–5 (total score = 40) that provided a self-assessment of confidence, surgical skill, knowledge and level of ‘anxiety’ in carrying out a cleft lip repair (Table 1). The validated procedural confidence assessment scale was created by Geoffrion and colleagues and adapted by Simulare.9,10
Questions about the level of training and prior experience (no experience, observer, assistant, primary operator) were added to the survey. Participants completed the survey before and after the simulation workshop. Responses were analysed for changes in confidence levels and perceived improvements in technical skills/knowledge.
Results
The participants’ levels of training and prior experience in cleft lip surgery are summarised in Table 2. Eleven (n = 11) plastic surgery trainees participated in the simulation workshop. This group was comprised of six early, four mid-level and one senior trainee. Two mid-level trainees had no prior cleft lip surgical experience; only two trainees (1 mid-level and 1 senior) had been primary operators under supervision.
The participants’ scores were tabulated following the completion of the workshop. The total scores out of 40 on the procedural confidence assessments included a subsection highlighting perceived technical ability (marking and executing the repair; questions 6 and 7). Statistical analysis was performed with the Wilcoxon signed rank test to assess changes from pre- to post-simulation—the use of this non-parametric test best suited assessment in the context of a small sample size.
Nine out of eleven (81.8%; p = 0.008) of the participants saw improvements in their procedural confidence scores at the end of the session. Comparison of pre- and post-simulation surveys depicted an average increase of 53.5 per cent in total scores. With the exception of one early-level trainee with no prior experience, improvements were present on an individual basis regardless of level of training/prior experience. A single mid-level trainee had unchanged scores across all questions pre- and post-simulation.
Improvement in confidence scores pertaining to technical skills averaged 84.5 per cent. Further statistical analysis within the early (n = 6) and mid-to-late (n = 5) level trainee sub-groups was conducted in relation to marking (Q6) and executing (Q7) a cleft lip repair. Statistical significance was reached within the early trainee subgroup with regards to confidence in marking out a cleft repair (p = 0.046). Sixty-six per cent of these trainees showed improvements in confidence surrounding executing the repair (p = 0.051).
Overall, participants with prior primary operating experience had the highest pre-simulation scores and the lowest percentage improvements noted post-simulation. The simulation benefited early-level trainees with an overall improvement in confidence assessments in five out of six (83.3%; p = 0.046). Similar figures were seen for mid-to-late level trainees (80%; p = 0.057) although this did not reach statistical significance (Table 3).
It is important to note that the scoring system is not an objective assessment of a participant’s surgical performance or ability, but rather a gauge of their confidence to conduct the procedure.
Discussion
Simulation training in surgery dates back to antiquity, with evidence of clay models being used in 600 BC to conceptualise nasal reconstruction with a forehead flap.11 Innovations over the last few decades have led to significant transformations to modern simulations, spanning across various modalities, from cadaveric to high-fidelity 3D models, to virtual reality and mechanised simulators. The aviation industry in particular has its training heavily rooted in simulation training. Primary objectives of flight safety and mission successes are achieved through familiarisation of its pilots with complex systems, and their ability to prepare for emergency situations.12,13
Surgical simulators may serve as a valuable adjunct in contributing to the acquisition of skills within a risk-free environment. This is especially relevant for a procedure that requires a high level of technical ability and geometric precision and where technical errors may result in lifelong problems for the child. Several high-fidelity cleft lip simulators have been identified in the literature.1,2,8,14–17 A review by Kantar and colleagues examining presently available cleft simulators, from digitally based to low and high-fidelity models, depicted that overall, favourable outcomes were present.4
The high-fidelity cleft lip simulator can provide a realistic representation of cleft anatomy. The construction of the simulators is based on computer tomography, modelling and 3D printing. The replication of mechanical properties akin to their real-life anatomical sub-units results in a level of haptic feedback that lends to a realistic simulation.1,8,14 Consequentially, users can simulate the cleft lip repair from start to finish, rather than carrying out technical markings alone. Multiple studies have shown evidence of positive feedback expressed by specialist cleft lip surgeons regarding the realism and applicability of high-fidelity simulators in surgical training.1,2,14 (Figure 3).
High-fidelity simulations have the potential to facilitate both the progression and refinement of technical skills through repetition, experimentation and a learned understanding of the nuances associated with cleft lip and palate surgery.2 Cleft specialist surgeons can supervise these exercises in a non-clinical setting—performed without any risk to patients and the associated stress. The assessment of skill and standardisation of procedural performance can thus be established before permitting a trainee to conduct cleft surgery on an actual patient.
The recent shift of the Australian and New Zealand plastic and reconstructive surgery curriculum from a syllabus to a competency-based approach enables registrars and supervisors to identify progression through training. Within this, milestones surrounding critical surgical procedures and skills in various sub-specialty areas are outlined, with the expected levels of supervision required at each level of training. Current training guidelines stipulate that early and mid-level trainees should ‘complete parts of the cleft lip/palate repairs under direct guidance’. Furthermore, senior trainees in their final year should expect to perform the repair in its entirety with a supervising surgeon present.
The snapshot of trainee experience at the inaugural cleft workshop depicted a discrepancy between expected competency levels, as dictated by the curriculum, and trainee exposure. A growing consensus exists that challenges faced by trainees regarding cleft surgery education can be addressed by simulation-based training.4–6,18 Evidence has shown that transferability of skills from the lab to the operating room exists, potentially addressing a significant portion of the learning curve via simulation exercises.4,18,19
Simulations have been widely embraced in microsurgery.6,20 Its role in skills development and retention has been well documented. Moreover, the repeatability, accessibility and ability to perform objective assessments of skill outside the operative setting lends leverage to the argument for using simulators to complement current learning opportunities and assess surgical competency.5,6,18,20
Presently, a single study in the literature details the high-fidelity cleft lip simulator experience at the registrar level. Riedle and colleagues designed, manufactured and subsequently reviewed the utility of 3D printed unilateral cleft lip and palate models on 20 residents at the University of Chicago and the University of California. All trainees within the study stated that the use of the model aided in improvements to surgical technique.8
The use of Simulare Medical high-fidelity cleft palate simulators as a training tool in the registrar cohort has been further evaluated in three separate studies, with favourable outcomes demonstrated.9,18,21 Podolsky and colleagues, developers of the Simulare Medical cleft lip and palate models, were involved in the above studies. Of 15 senior surgeons and fellows, all participants agreed that the simulator was a valuable training tool in increasing trainee competency, with 85 per cent agreeing on the anatomical accuracy and realism of the simulator.18 Ten participants (9 trainees, 1 fellow) completed pre- and post-simulation comprising a cleft palate procedural confidence scale and palatoplasty knowledge test.9 Following the session, all participants reported higher perceived procedural confidence (p < 0.05), while nine scored higher grades on the palatoplasty knowledge test. Overall, the studies concluded that the simulators were effective in increasing procedural confidence and determined to be valuable tools with the potential to increase procedural competency.9,18,21
Potential limitations associated with the use of high-fidelity models revolve around cost and accessibility. To our knowledge, Simulare Medical remains the only commercially available source for cleft lip models—the price of a single disposable cartridge amounting to US$175. The benchtop baseplate is included within a combination kit (US$2100) comprised of two lip and two palate cartridges, the necessary surgical instruments to complete either repair, headlights and a mountable USB camera for the assessment of palate repairs. A similar prototype model developed by Boston Children’s Hospital placed the estimated costs per device at US$220.2
Conclusion
Simulation training is a valid tool that aids in acquiring new skills and knowledge, indicating that there is scope for establishing and integrating simulation workshops into plastic surgery training curricula. As shown in this study, use of this platform may help bridge some of the current barriers trainees face in developing their skills by acquiring ‘hands-on’ experience in cleft surgery. Among the group of trainees who participated in the simulation workshop, favourable outcomes were noted, and an overall improvement in the procedural confidence was seen across the study group. We plan to repeat these sessions annually to facilitate cleft lip and palate surgery training and add to the growing data on simulation training.
Conflict of interest
The authors have no conflicts of interest to disclose.
Funding declaration
The authors received no financial support for the research, authorship and/or publication of this article.