Introduction
The pectoralis major myocutaneous flap is a reliable workhorse flap for reconstruction of the chest, and head and neck. In female patients with macromastia, there may be indication for a simultaneous superomedial pedicle breast reduction mammoplasty. The inferior pole of the breast and the inframammary fold can be harvested as the skin paddle of this myocutaneous flap.
We describe a case where the pectoralis major flap was used to reconstruct a supraclavicular defect with a simultaneous breast reduction. The inframammary fold was preserved with the pectoralis muscle flap which was accessed through a Wise-pattern reduction. This technique is suitable in women with macromastia who require a soft tissue reconstruction of the sternum or head and neck defect.
Case report
A 45-year-old woman presented with a six-week history of a growing lump in the left supraclavicular area. An excisional biopsy showed an epithelioid haemangioendothelioma. She underwent neoadjuvant radiotherapy prior to the wide local excision of the soft tissue tumour. On consultation for the reconstruction of this defect, the patient requested a bilateral breast reduction. She had no significant past medical history. She was not on any regular medication and was a non-smoker. On examination, the patient had large and asymmetrical breasts (bra size 14F), larger on the left. Nipple to notch was 30 cm, and nipple to inframammary fold was 12 cm. In her supraclavicular fossa, the scar from the biopsy was approximately 4 cm with surrounding post- radiation changes. This would require a wider excision for tumour clearance. The patient underwent a preoperative screening ultrasound and mammogram to rule out any breast pathology.
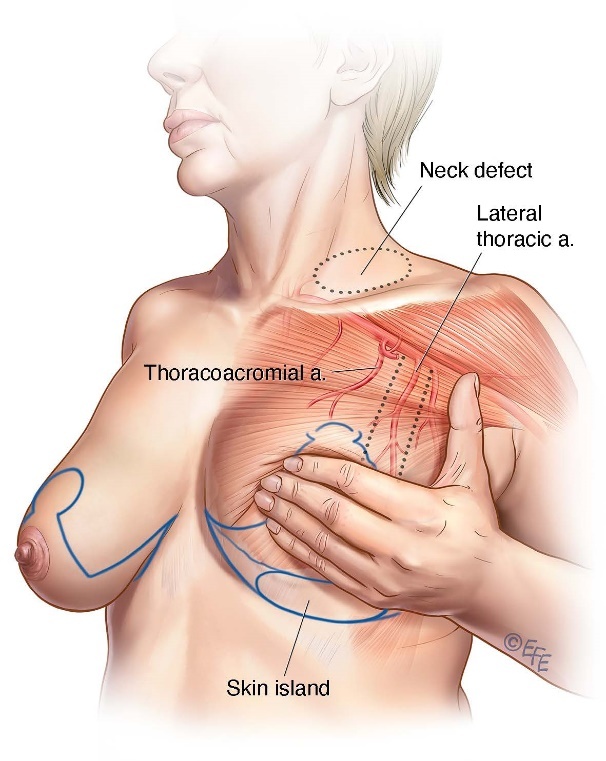
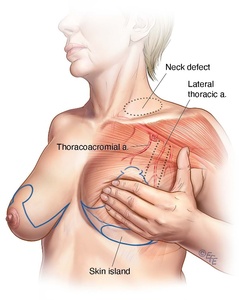
The surgery was performed in conjunction with a sarcoma surgeon who took a further resection margin from the lower neck (see Figure 1a and b). The reconstruction consisted of a pedicled pectoralis major myocutaneous flap for the supraclavicular defect and bilateral breast reduction based on a superomedial pedicle.
The operation was performed in supine position. The sarcoma surgeon resected the supraclavicular mass, creating a 8 x 5 cm defect. The Wise-pattern superomedial reduction was performed on the right side, and 710 g of breast tissue was removed on that side.
On the left side, the pectoralis major flap was raised based on the lateral thoracic artery. The skin island used was the left inframammary fold. The skin was dissected down to the pectoralis muscle. A submuscular dissection was performed using a lighted retractor, while the breast reduction offered adequate direct access to the pectoralis major. Once the pedicle was identified, a narrow strip of muscle containing the pedicle was then incised, with special care taken to spare the pedicle. An appropriate tunnel was dissected to facilitate the inset of the flap in the supraclavicular defect without compromising the vascular pedicle. After the flap was positioned, the reduction mammoplasty was completed in a standard closure (Figure 1c).
Discussion
The pectoralis major myocutaneous flap is a type V flap according to the Mathes and Nahai classification.1 The major pedicle for this flap is the thoracoacromial artery and the segmental arteries include the lateral thoracic artery and the perforators from the internal mammary artery.2
The pedicled pectoralis major flap is a reliable and robust flap used in sternal and head and neck reconstruction.3,4 It is considered to be the workhorse flap.5 Patients with osteonecrosis of the mandible, wound breakdown of the chest wall and sternotomy, local breast cancer recurrence and chest wall tumour often require soft tissue reconstruction.6 Median sternotomy wound breakdown after cardiac surgery has a reported incidence of 0.3–5.0 per cent.7 The rate is higher among patients with comorbidities such as obesity, diabetes, malnutrition and macromastia.8 The breasts produce laterally directed force on the wound edges, which leads to wound breakdown in spite of tension-free closure. Patients with macromastia may be candidates for a simultaneous reduction mammoplasty to reduce the risk of sternal wound dehiscence.9
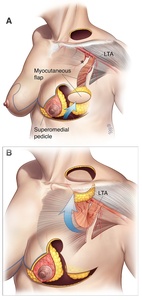
This procedure makes use of tissue present at the inframammary fold that would have otherwise been discarded in a superomedial breast reduction (Figure 2a). It is important to maintain a robust attachment of this area to the pectoralis major to avoid compromising the blood supply of the skin paddle (Figure 2b). A cutaneous skin paddle extending beyond the origin of the pectoralis major is well documented to be unreliable in reconstruction of head and neck defects.2 In order to increase the reliability of the skin paddle placed in the inframammary fold and lower pole of the breast, a robust parenchymal attachment is maintained between the mid to lower portions of the pectoralis major, breast tissue and planned skin paddle (Figure 2a and b). This may make the flap bulkier but optimises blood supply to this flap. A contralateral reduction mammoplasty can be performed at the same time with minimal added morbidity.
Conclusion
The technique described in this case uses a combination of a reliable flap with a reduction mammoplasty procedure. This combined procedure has multiple advantages including a single operation with only one general anaesthesia, comfortable patient positioning and wide flap access, and a mutually beneficial donor site without morbidity.9,10 In female patients with macromastia, and sternal or head and neck defect, this novel combination should be considered.
Acknowledgements
We would like to thank Mr Levent Efe for his illustrations. We would also like to acknowledge Dr Aimee Jenkins, FC PlastSurg (SA), who was involved with the initial concept discussions of this procedure.
Patient consent
Patients/guardians have given informed consent to the publication of images and/or data.
Conflict of interest
The authors have no conflicts of interest to disclose.
Funding declaration
The authors received no financial support for the research, authorship and/or publication of this article.
Revised: April 26, 2022
_preoperative_markings_which_include_the_wise-pattern_reduction__the_site_for_the_new_nipp.jpg)
_preoperative_markings_which_include_the_wise-pattern_reduction__the_site_for_the_new_nipp.jpg)