Introduction
Free flap salvage classically consists of anastomotic revision, local thrombectomy or systemic thrombolysis.1 These established interventions are not without risk: a return to theatre, bleeding and reopening of wounds with the potential for further damage to the pedicle and surrounding tissue. Delayed vascular compromise can result in poor outcomes, and surgical salvage is often unsuccessful while disrupting neovascularisation.
Catheter-directed thrombolysis has an excellent evidence base in cardiological and vascular procedures; however, it is only recently emerging in the microsurgical field for free flap salvage. Parry and colleagues first used this technique to concurrently salvage an acutely ischaemic lower limb and a rectus abdominis free flap.2 Recently, an increasing number of reports in the literature demonstrate the utility of this intervention for which an otherwise conventional surgical approach may be precluded.
We present a single case of delayed compromise in a free latissimus dorsi flap successfully treated with catheter-directed thrombolysis.
Case
The patient is a 75-year-old female non-smoker with a history of preoperative radiotherapy and wide local excision of a posterior thigh sarcoma followed by immediate reconstruction using a local perforator flap in 2016. Three years later she presented with a recurrent sarcoma surrounding the sciatic nerve, necessitating re-excision of the previous flap with segmental resection of the sciatic nerve and the entire extensor compartment. A free latissimus dorsi flap was used for functional muscle transfer, while sural nerve grafts facilitated sciatic nerve reconstruction.
During this latest procedure, the patient suffered intraoperative cardiac ischaemia, resulting in early termination of the operation. The free flap was partially raised but then re-inset. The proximal profunda femoris artery and vein were dissected as recipient vessels and showed good flow with normal intima. After the patient stabilised four days later, she returned to theatre for completion of reconstruction. Widespread clot was found throughout the profunda femoris artery and vein. A thrombectomy of each was performed with a Fogarty catheter, re-establishing flow. Fibrinous exudate on the intima was unable to be removed hence both vessels were shortened back to the medial femur, noting that there were no other suitable recipient vessels. After microvascular anastomosis, the flap became venously congested despite good flow across the anastomosis. Five thousand units of heparin was injected into the profunda vein with good resolution of congestion, and 25,000 units of urokinase was injected into the artery to thrombolyse any residual clot.
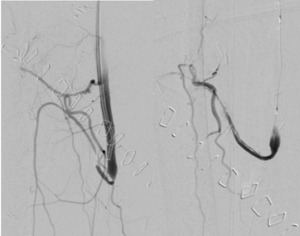
The patient started therapeutic enoxaparin and vascular surgical opinion was sought regarding options for flap salvage if it were to become necessary. Seven days postoperatively, the flap developed signs of arterial insufficiency (Figure 1).
Therapeutic enoxaparin was given, and radiologically guided catheter-directed thrombolysis commenced. Angiography via a retrograde left common femoral approach demonstrated extensive thrombus in the profunda artery proximal to the anastomosis over a length of 4 cm. The wire was passed beyond and a PROGREAT micro catheter run showed patent vessels in part of the flap. Attempts were made to clear the thrombus using 50,000 units of pulse spray urokinase through a small balloon catheter. Angioplasty using a 2 mm balloon was also performed proximally within the flap artery. Despite this, there was minimal restoration of angiographic flow yet significant clinical improvement of the flap was noted with re-establishment of an arterial Doppler signal.
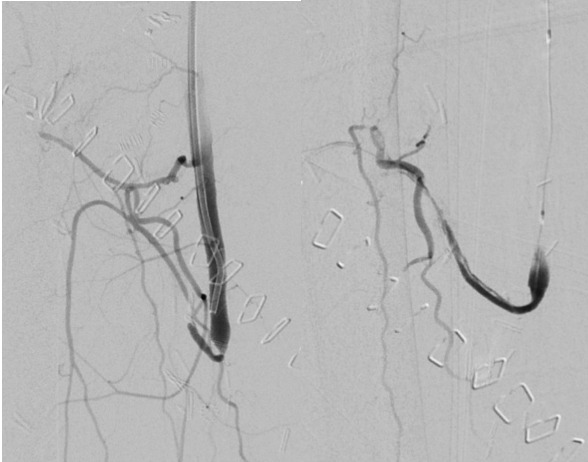
On day 11 Doppler signals were again lost, with visible hypo-perfusion. Angiography was repeated with an identical approach, demonstrating a patent anastomosis with thrombosis at the same site artery. Catheter-directed thrombolysis was repeated using 100,000 units of urokinase. Angioplasty with balloon dilatation was performed, though stent placement was not possible due to the tortuosity of the vessel. There was improvement in angiographic flow (Figure 2) and the flap regained good colour and capillary refill with the return of an arterial Doppler signal.
Post-procedure, the patient recovered well, and there were no further issues with vascular compromise to the flap. She was discharged on a three-month course of aspirin, and at the time of writing (two years later), has had an uncomplicated recovery with good motor function of the affected limb (Figure 3).
Discussion
Catheter-directed thrombolysis should be considered as an intervention for late flap failure. Acland and colleagues describe two separate zones of endothelial injury: the anastomotic site (zone I) and downstream (zone II).3 Due to the anastomosis healing within the first week, delayed presentations are more likely to consist of zone II injuries. In this case, prolonged vascular stasis increased suspicion for a zone II injury. These injuries often result in multiple downstream microvascular thrombi with diffuse endothelial injury, which can be challenging to treat with a surgical thrombectomy. Targeted thrombolysis should be considered in this situation.4
Timing of vascular compromise is another pertinent factor. Delayed flap loss often responds poorly to surgical salvage, and can disrupt neovascularisation around the inset of the flap. The minimally invasive approach of catheter-directed thrombolysis is invaluable in retaining the integrity of both the pedicle and healed surgical wounds, while also allowing high doses of targeted thrombolytic therapy to be delivered. In addition, it has been used as a successful salvage therapy in ultra-delayed arterial thrombosis more than 10 years post-procedure.5
The anatomy of the anastomosis may also raise challenges when attempting flap salvage. Our patient had short recipient vessels, and any further resection would have been challenging and necessitated a vein graft, increasing thrombosis risk. The morbidity of an operation should also be considered, and high-risk patients, including burn victims,6 may benefit from a minimally invasive procedure.
Lastly, any interventions should occur immediately, and early involvement of the multidisciplinary team is critical for successful catheter-directed thrombolysis. Discussions should begin when the surgeon considers the flap’s high risk for vascular compromise, to facilitate availability of a vascular interventionalist.
Conclusion
In summary, catheter-directed thrombolysis is a novel technique that may be a valuable tool for flap salvage late in the postoperative period. It is a relatively low risk procedure that can be undertaken in multi-morbid patients, while additional benefits include its utility in delayed flap compromise, flaps with anatomy precluding vascular resection, and downstream zone II injuries.
Patient consent
Patients/guardians have given informed consent to the publication of images and/or data.
Conflict of interest
The authors have no conflicts of interest to disclose.
Funding declaration
The authors received no financial support for the research, authorship and/or publication of this article.
Revised: October 4, 2022; January 26, 2023 AEST