Introduction
The keystone perforator island flap (KPIF) has been applied in reconstructive techniques since 2003.1 As a result of its extensive use, mainly in head and neck reconstruction, beneficial characteristics of the island flap technique have been described.2 These are best summarised by the acronym ‘PACE’ which refers to ‘pain-free aesthetic appearance with low complications and efficiency’ both in times for operating and healing (Figure 1).
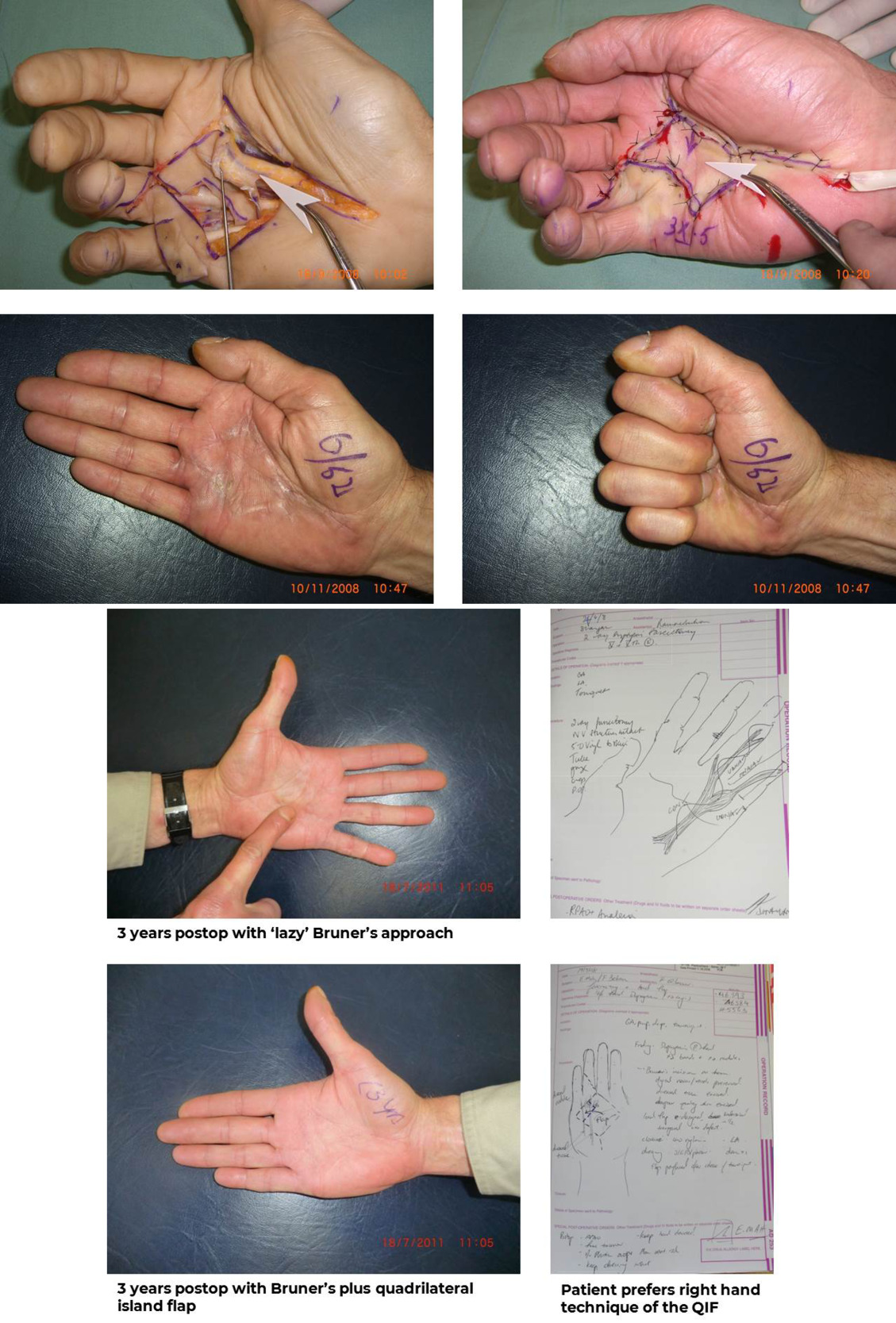
Formerly, the standard practice in Dupuytren’s disease was to use longitudinal exposure along the contractual band of the disease with Bruner’s z-flaps—though John Hueston preferred the technique of a linear incision and the secondary development of z-plasties in the manner of the McIndoe technique.3 Over the years, palmar defects caused by dermofasciectomy of contracted tissue have been treated with variations ranging from the McCash technique4 of open granulation tissue healing to John Hueston’s full-thickness grafting technique5 to various flap techniques such as the z-plasty (Table 1).6
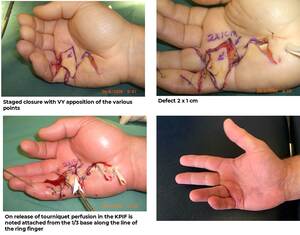
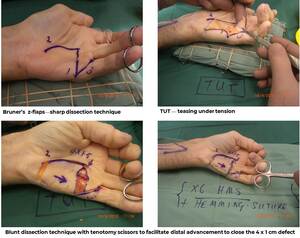
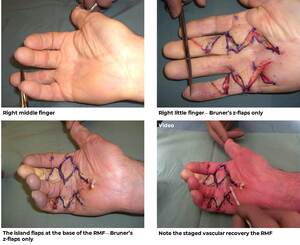
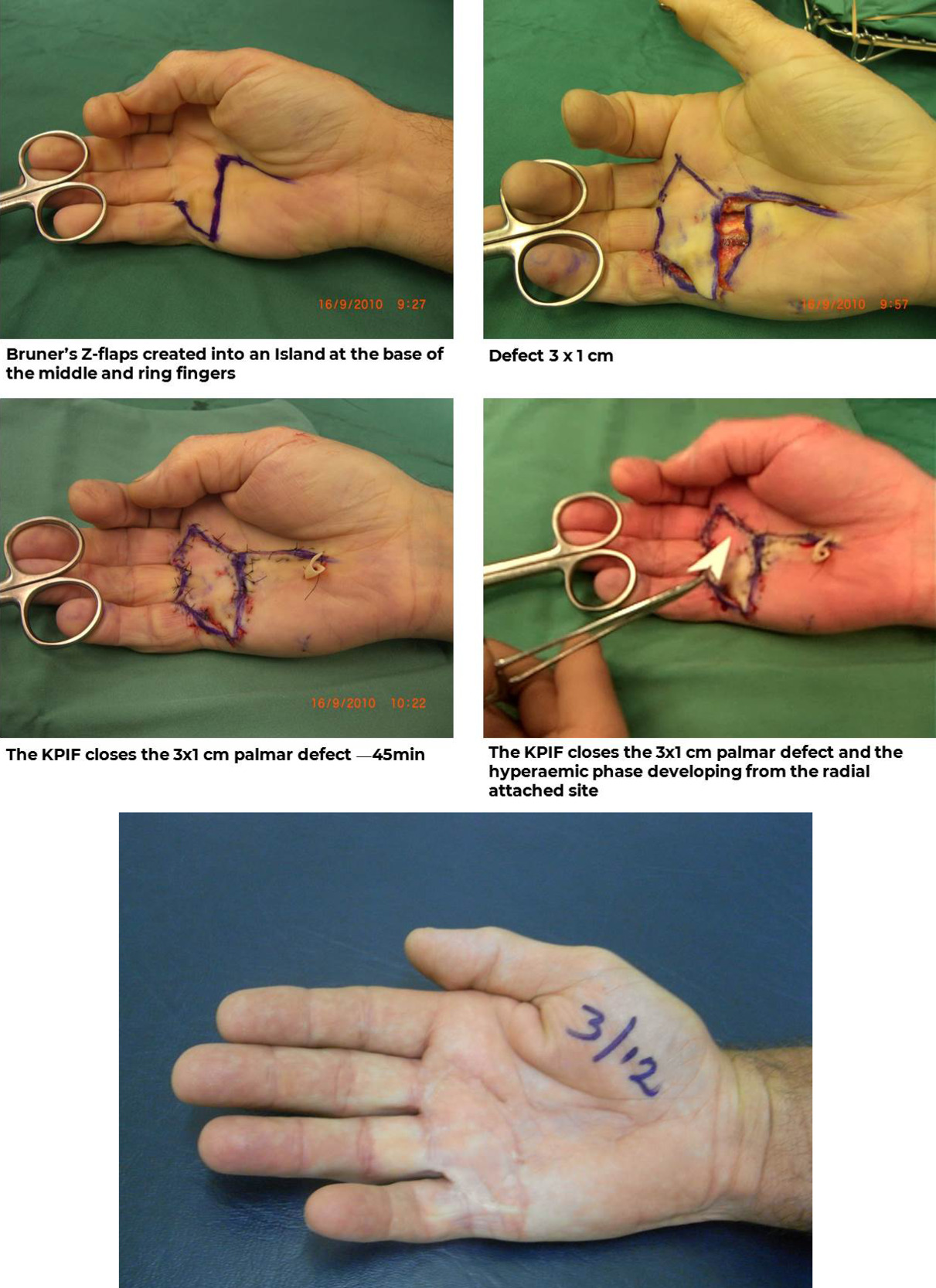
In the keystone technique, Bruner’s z-flaps are ‘islanded’ leaving one-third of the triangular base design attached as the source of vascular supply for non-specific perforators from the proximal and distal palmar arches. These randomly located perforators are not individually detailed or dissected. Island flaps can then be used to reconstruct tissue defects particularly over the region of the 4th and 5th metacarpals.
In the cases illustrated with this article, I describe the vascular dynamics of KPIF reconstruction used in Dupuytren’s disease in conjunction with Bruner’s z-flaps.6
Background
Dupuytren’s fibromatosis is a genetically determined, fibroproliferative disorder that causes contracture of the digits mainly in the ulnar half of the hand in the vicinity of the power grip region and the ulnar nerve neurodermatome alignment. The resultant digital contracture of the ring and little fingers compromises the functional dexterity of the hand causing social and industrial inconvenience. In the Dupuytren’s diathesis, the disease progresses towards the median half of the hand. In longstanding cases, dermofasciectomy procedures eliminate contractures and help to improve functional recovery.
As a result of surgical correction, palmar defects occur in the vicinity of the metacarpophalangeal (MCP) crease lines. In order to extend the digits into functional alignment, a secondary defect occurs that can be surgically corrected using skin grafts. This was the basis of John Hueston’s firebreak principle,5 popularised in the mid-1980s. In 2003, I introduced the principle of a fenestrated, full-thickness graft to optimise graft-take and expedite healing, offering an alternative for the management of palmar defects created by surgical release.1 Since then, techniques of KPIF reconstruction have been used extensively throughout the body, including to close major melanoma and head and neck defects after excisional surgery.2
The clinical design of the keystone shape can be modified to suit variations in palmar defects following surgical fasciectomy—not forgetting that the keystone arc is really a conjoined double vy-flap based on random perforators, in this case of the distal palmar arch. Creating islands of tissue produces hypervascularity and what is, hypothetically, a sympathectomy effect. This clinical finding is regularly observed in palmar reconstruction using KPIF where Bruner’s z-flaps are islanded leaving one-third basal attachment as the source of vascular supply as a guarantee of rapid healing.
This hypervascularity (illustrated in detail in the linked audiovisual files) is in strong contrast with the slower vascular perfusion changes observed in the standard design of Bruner’s flaps, which are not islanded. The combination of reliable hypervascularity with a pain-free postoperative phase, characteristic of KPIF, ensures an easy recovery with early commencement of hand therapy. With minimal vascular complications (apart from clinical cases such as diabetics) the overall surgical outcome gives an aesthetic appearance matching surrounding tissues. This follows the Gillies principles of replacing ‘like-for-like’ and ‘the next best tissue is the next best tissue’.7
Techniques for the closure of defects of the palm date back to the McCash technique, where MCP contractures, mainly over the fifth digital ray, create an area of tissue loss that can be 2–3 cm in length depending on the age of the patient and the state of the Dupuytren’s contracture (type IV). John Hueston’s graft technique5 replaces tissue loss with like tissue (in the Gillies manner), overcoming limitations of the McCash4 technique (such as healing by secondary granulation).
When Bruner’s z-plasty exposures are done as part of the Dupuytren’s fasciectomy technique, these z-flaps are part of the initial design mark-out. The traditional creation of z-plasties following longitudinal exposure has been replaced by the technique of islanding Bruner’s flaps using KPIF principles. Z-flaps may lead to vascular impedance and slower healing in certain patients (particularly the elderly), and so hypervascularising the z-flaps by making an island assists in the successful repair of closures of Dupuytren’s wounds.
The four observed clinical advantages of the KPIF technique when applied with a smaller triangulate design become evident when one considers it is a VY-flap,8 which is really a keystone flap in hemi-section. Besides hypervascularity, the other major advantage of KPIF is the temporary state of anaesthesia created by the island flap which recovers at the somatic level and results in pain-free healing (observed to last up to three months and a feature often seen in any surgical wound where temporary denervation recovers somatic input). Using the KPIF for Dupuytren’s, the appearance of the palm no longer needs amplification as the island flap reconstruction uses the same tissue as that adjacent to the defect. Given that complications are rare with KPIF (excepting patients with diabetes or who smoke), the therapeutic, economic and aesthetic benefits of this technique are clear.
A series of ten cases, viewable on YouTube, illustrate these established principles.
Discussion
The fibroproliferative disorder of the palm, characteristic of Dupuytren’s disease, is sometimes referred to as the ‘Viking’s disease’, recalling the rowing technique used by Vikings to cross the North Sea in flat-bottomed boats. The source of the expression comes from the Viking ‘power grip’ where the oar is held in the ulnar half of the hand, resulting in limitations in function. As the Vikings invaded Europe and the British Isles this became a genetic characteristic for generations world-wide and is strongly linked to family history, with a predominance of 75/25 between males/females.9
The aetiology of Dupuytren’s disease is not fully understood but it is strongly evident in family histories.10 The Dupuytren’s diathesis5 is also not well understood, though diabetes mellitus and smoking are strongly associated with the disease. (It is noteworthy that in the two KPIF cases illustrated with this article that experienced complications, diabetes and smoking featured in the clinical stories.)
A review by Rodrigues and colleagues10 provides a summary of cases from the Nuffield Department of Orthopaedics and other rheumatological units around the world. The authors review various studies and clinical trials, with the number of cases totalling 944 hands. Outcomes for the return of hand function are reviewed using the DASH (disabilities of the arm, shoulder and hand) scoring system. The authors provide an overview of various techniques, including a simple needle fasciotomy and injection of the enzyme digestive factor collagenase.
Significantly, the only reference to a plastic surgeon is from the Oxford University Hospital, even though the plastic and reconstructive techniques used for repair following fasciectomy date back to the surgery of Sir Archibald Hector McIndoe at East Grinstead.3 John Hueston, McIndoe’s Australian protégé, came to world prominence for his refinement of hand surgery techniques. The application of KPIF in the closure of palmar defects following radical fasciectomies is based on these published plastic and reconstructive principles.2–7
In the cases and clinical trials reviewed by Rodrigues and colleagues10 it is interesting to note that needle fasciotomy received better patient satisfaction outcomes after six weeks. While patient satisfaction with these techniques at six weeks is evident, the recurrence rate is high—as both these techniques leave the ruptured ends of the fibromatous bands in place to reconnect during healing.
At the five-year mark, satisfaction was higher in the fasciectomy group, while fasciotomy had a higher recurrence rate. Hueston’s skin grafting technique did not produce a better outcome than fasciectomy alone. By comparison, however, the keystone island flap, being a loco-regional reconstruction, produces better outcomes than Hueston’s technique in terms of pain-free movements, rarer complications and an efficient operative time-frame—PACE.
Hueston’s Wolfe graft technique is reported to lower the recurrence rate but this depends on the surgical technique and the size of the graft. The essence of the KPIF technique is to provide another variation of reconstructive closure in palmar defects following the fasciectomy to reduce recurrence.
Rodrigues and colleagues also found that wearing night splints after surgery does not straighten the fingers to improve hand function. With the KPIF technique, however, the 4th and 5th digits are held into extension with Kirschner wire (K-wire) stabilisation for 10 days while the KPIF tissue heals and then, with hand therapy following the removal of the K-wire, mobilisation commences.
Further, the authors found that finger straightening is preferable to that of a needle fasciotomy when long-term recurrence is an issue.10 The complications arising from ‘blind’ surgery and digital nerve dysfunction are self-evident.
For the more afflicted type III and IV Dupuytren’s cases, dermofasciectomy (the removal of such tissue) leaves the flexor tendons and neurovascular bundles intact. The KPIF reconstruction can be used anywhere in the palm and particularly over the MCP joints to achieve reconstructive continuity. KPIF can be applied to all age groups, and particularly patients with a Dupuytren’s diathesis and hence a likelihood of recurrence later in life. The KPIF technique eliminates limitations of other techniques in terms of time, healing and delay with mobilisation—which is implicit in any skin graft technique as any graft loss delays overall recovery (again, note that the only complications among the KPIF cases illustrated with this study related to a patient with diabetes and another a heavy smoker—see Tables 2 and 3 and Figure 2).
The relative economic efficiency of skin grafts and flap closures comes down to the fact that grafting procedures take longer to perform. The KPIF technique addresses this by allowing expeditious flap closure as long as the island flap—leaving a one-third attachment—is teased into position. Importantly, an island flap with one-third attached can be stretched into various palmar defects by manoeuvre and by blood dissection around the periphery, followed by VY-closure of the advancing points of the KPIF triangle.
Conclusion
This article describes the applications of keystone principles in repairing palmar defects created by surgical excision arising from Dupuytren’s disease as an alternative to John Hueston’s firebreak graft.5 As Rodrigues and colleagues state, the primary goal of treatment is to ‘excise, divide, break or dissolve’ the fibro-proliferative disorder of Dupuytren’s disease. From a plastic surgery point of view, excision and reconstruction is the optimum technique to produce satisfactory functionally improvement of hand movement with minimal recurrence. Island flaps based on the keystone principle improve vascularity resulting in minimal complications with healing. Recurrence of Dupuytren’s disease following this technique has not been observed to date.
Videos
Supplementary material
Supplementary audiovisual material accompanies this text: LINK
Acknowledgements
Audiovisual presentation complements this paper. Produced for the author by Woodrow Wilson Clinical Imaging.
Consent to publish
Patients/guardians have given informed consent to the publication of images and/or data.
Disclosures
The authors have no conflicts of interest to disclose.
Funding
The authors received no financial support for the research, authorship and/or publication of this article.