Introduction
Performing perforator-based flap reconstruction requires careful selection of the perforator, flap design and donor site. A suitable perforator is ideally harvested from a donor site with minimal morbidity and is large enough to facilitate microsurgical anastomosis and adequately supply all portions of the flap.1 In recent times, an increasing number of plastic and reconstructive surgeons have begun using modern 3D imaging and printing technologies to aid preoperative planning, intraoperative guidance and medical education.2,3 However, there is a lack of comprehensive review of these techniques that provides a global understanding of this novel field in a language suitable for clinicians.
Currently, a plethora of imaging modalities is being used in plastic and reconstructive surgery, mainly computed tomography angiography (CTA) and magnetic resonance angiography (MRA).4–9 First reported for perforator-based flap planning in 2006,6,7 CTA is widely used in preoperative investigations by institutions around the world and is considered the gold standard due to its high accuracy and reliability.4,5,10–13 However, CTA poses the potential risk of additional radiation exposure, involves intravenous administration of iodinated contrast media and does not provide haemodynamic features such as flow velocity and direction.
Magnetic resonance angiography bypasses radiation exposure but is limited by only being able to detect vessels greater than 1 mm in diameter.14 It also has lower spatial resolution15 and poorer contrast differentiation from the surrounding soft tissue.16 As a result, MRA has a lower sensitivity (50%) for detecting abdominal wall perforators than CTA.9 Enhanced by recent advances in imaging techniques,17 contrast agents18 and increasing availability of higher field-strength scanners,19 more recent studies have reported improved sensitivity in identifying perforators (91.3–100%).8,20–24 As a result, MRA remains an investigation of choice for younger patients and for those with iodine allergy and impaired renal function.25
In this review, we evaluate the established 3D imaging and printing techniques based on CT and MRI.
Methods
We reviewed the published English literature from 1950 to 2017 from well-established databases such as PubMed, MEDLINE®, Web of Science and EMBASE. We included all studies that analyse 3D imaging and printing techniques used in surgery, especially plastic and reconstructive surgery. We used search terms such as ‘3D imaging’, ‘CTA’, ‘MRA’, ‘3D image software’, ‘volumetric analysis’, ‘3D printing’, ‘preoperative planning’, ‘intraoperative guidance’, ‘education’, ‘training’ and ‘customised implant’. We also retrieved secondary references found through bibliographical linkages.
3D imaging rendering software
Through our literature review, we identified the most commonly used 3D image rendering software suites in medical application. We identified their specifications, such as the software language on which they are based, cost, open-source capability and function, by accessing the manufacturer’s website or from publications.
3D perforator mapping
We identified that CTA and MRA are the most commonly used imaging modalities for 3D perforator mapping. Hence, we evaluated the software suites based on these modalities.
3D volumetric analysis
We focused our analysis of 3D volumetric analysis based on conventional 3D imaging techniques, CT and MRI. We systematically identified a list of software suites used to analyse 3D volumetric data from CT or MRI and examined their application in plastic and reconstructive surgery.
3D printing
Studies using 3D printing for preoperative planning in plastic and reconstructive surgery were assessed using Oxford Centre for Evidence-Based Medicine levels of evidence.26 Given that the most common 3D printing application in plastic and reconstructive surgery is mandibular reconstruction with free fibular flap, we performed a focused further qualitative analysis of this application.
Results and discussion
Numerous studies have explored the application of conventional imaging modalities for 3D perforator mapping, 3D volumetric analysis and 3D printing.
3D image rendering
Proprietary software provided by manufacturers of CT and MRI scanners generally offers only two-dimensional image-viewing capabilities. As a result, numerous free, open-source software platforms have been developed that are capable of 3D image rendering. They are built on robust, but limited, open-source software libraries that provide the basic architecture. In plastic and reconstructive surgery, the most commonly used free software platforms are 3D Slicer (Surgical Planning Laboratory, Boston, MA, USA) and OsiriX (Pixmeo, Geneva, Switzerland) (see Table 1).
3D Slicer
3D Slicer27 is a well-supported, open-source platform built on Insight ToolKit (ITK) and Visualisation ToolKit (VTK) using C++ and Python.2 Developed to segment brain tumours from MRI scans,29 3D Slicer is used in a variety of medical applications ranging from lung cancer diagnosis30 to cancer imaging.31 This software is adept at generating volumetric images for 3D printing through thresholding and segmentation techniques.
OsiriX
The OsiriX28 image-viewing software platform is built on ITK and VTK, for Macintosh computers only. It has an intuitive graphical user interface and fast processing speed make it popular with clinicians worldwide.28 OsiriX enables viewing of multidimensional data such as positron emission tomography (PET)-CT32 and cardiac-CT as well as standard tomographic scans (CT and MRI).33 It is suitable for viewing 3D and 4D datasets but limited to 3D anatomical models of large organs such as long bones and the heart.
3D perforator mapping
In perforator based, free flap reconstruction, plastic surgeons commonly rely on CTA- or MRA-based 3D reconstructed images of the relevant perforators for preoperative planning (see Figure 1).
CTA
Computed tomography angiography is the most commonly used imaging modality for 3D perforator mapping, using maximum intensity projection (MIP) and volume-rendered technique (VRT) 3D software reconstruction techniques. Compared with Siemens Syngo InSpace 4D (Siemens, Erlangen, Germany) and VoNaviX (IVS Technology, Chemnitz, Germany), which are expensive, and virSSPA (University Hospitals Virgen del Rocio, Sevilla, Spain), which is not available outside the original institution, OsiriX software platform is free and has been demonstrated to be as accurate.
MRA
Modern magnetic resonance technology can provide superior 3D reconstructed images. However, they are expensive, time-consuming and relatively difficult to perform. Similar to CTA, free OsiriX software can be used for 3D perforator mapping from MRA. Recently, investigators have developed a semi-automated plugin tool for analysing MRA images using OsiriX, However, it remains to be validated in a large cohort.
3D volumetric analysis
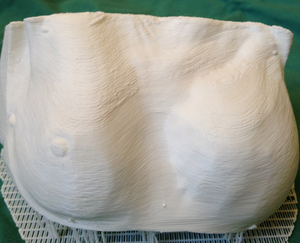
Accurate assessment of tissue volume is an important aspect of preoperative planning in plastic surgery.34–38 Particularly in breast reconstructive surgery, volumetric analysis is paramount for achieving symmetrisation and a satisfactory outcome.39–44 However, an accurate, reliable and convenient method of objective breast volumetric analysis has remained elusive (see Figure 2 and Table 2).45
CTA
Calculating the flap volume from CTA and comparing it with the intraoperative flap weight, Eder and colleagues reported high correlation between the two measurements (r = 0.998, p < 0.001) demonstrating the high prediction accuracy of CTA (0.29%; –8.77 to 5.67%).39
In order to further improve its accuracy, Rosson and colleagues placed fiducial markers on the surgical incision line before the CTA and achieved accuracy of up to 99.7 per cent (91–109%).43
Lee and colleagues calculated a ratio using the volume of the breast and the potential deep inferior epigastric artery perforator (DIEP) flap from CTA and created a treatment algorithm.46 If more than 50 per cent of the harvested flap is required for reconstruction, surgeons can make modifications to the flap design by increasing its height, capturing more adipose tissue by bevelling superiorly from the flap’s upper margin, like Ramakrishnan’s extended DIEP technique,51 and incorporating multiple perforators if available. If more than 75 per cent of the flap is required, venous augmentation is performed with contralateral superficial inferior epigastric vein. Using this algorithm in 109 consecutive patients, the authors noted a significant reduction in perfusion-related complications (5.6 vs 22.9%, p = 0.006) and fat necrosis (5.6 vs 19.1%, p = 0.03).
MRI
In comparison to CT, MRI has superior soft-tissue resolution and is thus more accurate at measuring breast volumes (r = 0.928 vs 0.782, p = 0.001)52 and has a mean measurement deviation of only 4.3 per cent.53 Furthermore, Rha and colleagues show that MRI- derived breast volume is more accurate than the traditional volumetric method using a plaster cast (r2 = 0.945 vs 0.625).41
Using the manufacturer’s specifications as gold standard, Herold and colleagues measured the volume of breast implants using MRI in patients with bilateral augmentation mammaplasty.44 Furthermore, they compared the accuracy of three commonly available 3D image processing software platforms: OsiriX, BrainLAB (BrainLAB AG, Feldkirchen, Germany) and Medis Suite MR (Medis Medical Imaging Systems BV, Leiden, The Netherlands). BrainLAB had the lowest mean deviation of 2.2 ± 1.7 per cent, followed by OsiriX at 2.8 ± 3.0 per cent and Medis Suite MR at 3.1 ± 3.0 per cent. However, all software platforms correlated highly accurately with the reference overall (r = 0.99). Interestingly, software analysis is fastest using OsiriX at 30 seconds per implant, followed by BrainLAB and Medis Suite MR at 5 minutes.
To date, most software techniques remain manual, that is labour-intensive and reliant on operator experience, while validated evidence of commercially available automatic segmentation tool is scarce.47,54 Interestingly, Rha and colleagues used ImageJ, a free NIH-developed image processing program, to successfully perform volumetric analysis of the orbit and breast from CT and MRI, respectively.48 However, ImageJ has yet to be investigated in clinical application.
3D printing
In contrast to medical imaging modalities that are limited by being displayed on a 2D surface, such as a computer screen, a 3D-printed biomodel can additionally provide haptic feedback.2,55–58 Three-dimensional printing, also known as rapid prototyping or additive manufacturing, describes a process by which a product derived from computer-aided design (CAD) is built in a layer- by-layer manner.59–61 The main advantages of 3D printing are the ability to customise, cost-efficiency and convenience.62,63 Since its introduction, the use of 3D printing in surgery has been extensively investigated.
In clinical application, two types of software platforms are required for 3D printing: 3D modelling software that can convert standard Digital Imaging and Communications in Medicine (DICOM) files from CTA/MRA into a CAD file; and 3D slicing software that divides the CAD file into thin data slices suitable for printing.64 A range of modelling software is available but only the following are user-friendly and commonly reported: 3D Slicer,47,65 OsiriX66 and Mimics (Materialise NV, Leuven, Belgium).67 Three-dimensional slicing software usually accompanies 3D printers at no additional cost and has a simple user interface such as Cube software (3D Systems, Rock Hill, SC, USA), MakerBot Desktop (MakerBot Industries, New York, NY, USA) or Cura (Ultimaker BV, Geldermalsen, The Netherlands).
In clinical application, a host of 3D printer types have been used including fused filament fabrication (FFF), selective laser sintering (SLS), stereolithography (SLA), binder jetting and multijet modelling (MJM).2 Fused filament fabrication is the most common and most affordable 3D desktop printing technology available.68–70 In an FFF 3D printer, a melted filament of thermoplastic material is extruded from a nozzle moving in the x–y plane and solidifies upon deposition on a build plate.71 More recently, 3D metal printing using SLS has gained popularity in creating sterilisable surgical guides72,73 and customised dental implants.74
Encouraged by its potential, surgeons from a wide range of specialities have applied 3D printing to their practice such as neurosurgery,75–82 cranio-maxillofacialsurgery,83–90 cardiothoracicsurgery,91,92 orthopaedic surgery,93,94 transplantation,95–97 ear, nose and throat surgery98,99 and breast cancer surgery.100 Similarly, in reconstructive plastic surgery, 3D printing appears most useful for preoperative planning, intraoperative guidance, medical education and creating custom implants. 3D-printed bespoke implants overlap significantly with 3D bioprinting101–103 and are beyond the scope of this article.
Preoperative planning
Three-dimensional printing has been most commonly used in plastic and reconstructive surgery for preoperative planning (see Table 3).
Autologous breast reconstruction
In 2014, Gillis and Morris reported the first case of a 3D-printed internal mammary artery (IMA) and its perforators, a common recipient site in free flap breast reconstruction.104 Similarly, Mehta and colleagues 3D-printed a multi-colour, multi-material model of a deep inferior epigastric artery (DIEA) and its perforators.105 Despite the benefits, both studies revealed the high cost of 3D printing (US$400–US$1200 per model), mainly due to having to outsource the manufacturing. In addition, outsourcing introduces delays of up to six to eight weeks that may not be appropriate in some clinical settings. As a result, Suarez-Mejias and colleagues developed their own 3D modelling software called AYRA (Virgen del Rocio University Hospital, Sevilla, Spain).106 More recently, Chae and colleagues described an affordable and convenient technique of 3D printing using free software platforms and desktop 3D printers (see Figure 3).47
Soft-tissue modelling
In a case of lower limb reconstruction, Chae and colleagues 3D-printed a model of the soft-tissue defect that aided in flap design.65 Similarly, Garcia-Tutor and colleagues used 3D-printed models of large sacral defects to perform qualitative and quantitative volumetric assessment.66 Cabalag and colleagues fabricated a model of a giant squamous cell carcinoma that was useful for planning hemi-mandibulectomy and determining the length of the free fibular flap required.107
Bony modelling
Taylor and Lorio 3D-printed, in-house, a negative mould of a scaphoid/lunate defect from avascular necrosis from which a silicone model was created, sterilised and used intraoperatively for flap planning.108 In an interesting application, Chae and colleagues described their technique of four-dimensional (4D) printing whereby multiple models of the thumb and wrist bones were 3D printed from 4D CT scans to demonstrate their dynamic relationship.
Cartilage modelling
Three-dimensional assessment of nasal cartilaginous defect can be useful for planning reconstruction. Visscher and colleagues demonstrated that 3D printing alar cartilages using MRI showed a mean error of 2.5 mm.109 Interestingly, most of the difference was found in 3D printing the medial crus but the lateral crus remained highly accurate, probably due to its more linear shape. Recently, Choi and colleagues 3D-printed a patient-specific negative mould from CT to create silicone nasal implants for augmentative rhinoplasty using in-house software110 and demonstrated a mean accuracy of 0.07 mm (0.17%) with no complications.
Intraoperative guidance
Use of 3D-printed fibular osteotomy guides for mandibular reconstruction has been studied extensively (see Table 4).68,112–126 Investigators have demonstrated their accuracy of up to 0.1–0.4 mm.68,113–115,120 Moreover, they can significantly reduce flap ischaemia time (120 minutes vs 170 minutes, p = 0.004)117 and total operating time (8.8 hours vs 10.5 hours, p = 0.0006).120
Medical education
Educating junior surgical trainees and medical students about 3D pathological defects such as cleft lip and palate without hands-on interaction and demonstration is notoriously difficult. As the supply of cadavers for medical education continues to dwindle due to rising maintenance costs127 and concerns regarding occupational health and safety,128 the use of 3D-printed biomodels has become popular.129,130 Zheng and colleagues have used 3D-printed negative moulds to fabricate soft silicone models of cleft lip and palate on which students directly perform cheiloplasty.131 Subsequently, in a randomised clinical trial of 67 medical students, AlAli and colleagues demonstrated that the knowledge gained using 3D-printed models of cleft lip and palate was significantly higher than when using standard slide presentations (44.65% vs 32.16%, p = 0.038).132 Similarly, clinicians have 3D printed negative moulds of paediatric microtia for practical demonstration.133
Conclusion
Many studies have explored the application of 3D-rendered conventional imaging modalities for 3D perforator mapping, 3D volumetric analysis and 3D printing.
There are numerous free, open-source software platforms that are capable of 3D image rendering, such as 3D Slicer and OsiriX. For perforator mapping, most plastic surgeons rely on CTA- or MRA-based 3D reconstructed images. Current 3D volumetric analysis technologies remain labour-intensive and are yet to be automatised.
Three-dimensional printing has been most commonly used in plastic and reconstructive surgery for preoperative planning in mandibular reconstruction with a free fibular flap. The majority of these studies have a lower level of evidence, consisting of case series and reports. Furthermore, there is a lack of comprehensive review of all established 3D imaging and printing techniques in a language suitable for clinicians.
Disclosures
The authors have no conflicts of interest to disclose.
Funding
The authors received no financial support for the research, authorship and/or publication of this article.
-based_three-dimensional_(3d)_perforator_mapping_in_dee.jpg)

-based_three-dimensional_(3d)_perforator_mapping_in_dee.jpg)

