Introduction
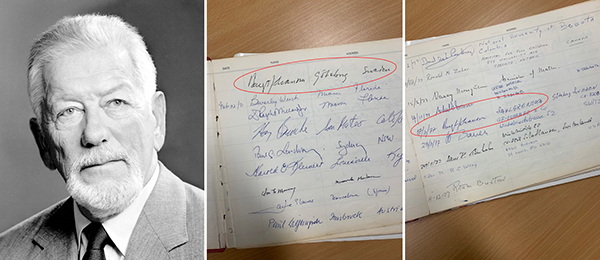
This is a joint perspective by two microsurgeons, Dr Ingemar Fogdestam of Sweden and Dr Richard Hamilton of Australia, written to mark the 40th anniversary of the first use of a free abdominoplasty flap in breast reconstruction (Figure 1). It is not widely known that Australia played a key role in the development and first performance of this free- flap technique. Although the pioneering operation was performed in Sweden, Australian resources and expertise lay behind the breakthrough.
Richard Hamilton, July 2019, Adelaide, Australia
Microsurgery revitalised surgical practice in the second half of the 20th century and Australia was at the forefront of the new field. Melbourne hosted the prestigious Fifth International Confederation of Plastic and Reconstructive Surgery (IPRS) in 1971, while the previous year Dr Bernard O’Brien had succeeded in setting up the Microsurgery Research Centre that subsequently became part of St Vincent’s Hospital (Figure 2). The centre rapidly developed an international reputation. The field was so new that the centre had to design its own operating instruments and micro sutures1 to be manufactured by its own instrument maker.2 In 1973 the world’s first successful free island flap transfers for lower limb salvage were performed in Melbourne—these were among the first free island flap transfers in a human performed anywhere in the world.3,4
O’Brien set up a generous outreach program: every year, four fellowships were granted to overseas plastic surgeons, together with a living allowance, to come to Melbourne and be trained in microsurgery with the idea that they should return to their home countries and develop the field there.5 The fellows both observed and participated in all the microsurgery operations that took place at the hospital, as well as carrying out research projects in the centre’s laboratory under the supervision of O’Brien and Wayne Morrison.
In 1977 I became a member of the centre. I had been senior registrar at Flinders Medical Centre in South Australia but I could see that microsurgery, although in its infancy at the time, was going to have a far-reaching effect on plastic surgery. I was aware of St Vincent’s pre-eminent reputation and was lucky enough to gain the post of senior registrar in plastic surgery there.
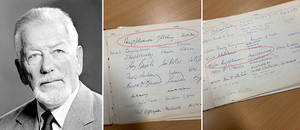
Meanwhile, at Sahlgrenska University Hospital in Gothenburg, Sweden, where a pioneering free- flap operation was to take place in two years’ time, Professor Bengt Johanson, head of the plastic surgery department, had also realised the implications of the new speciality of microsurgery. He had travelled to Australia in 1971 for the IPRS and had visited O’Brien’s microsurgery centre, sensing how important microsurgery was going to become (Figure 3). By 1976 Johanson was very conscious that there was no work at all being done in this field in Sweden. It was time to take advantage of Australia’s willingness to share its expertise. He decided to seek a fellowship to send one of his young surgeons, Dr Ingemar Fogdestam, to St Vincent’s to be trained so that when he returned to Gothenburg he could set up a microsurgery unit there.
So Ingemar and I both arrived at St Vincent’s at the same time. My work as senior registrar in plastic surgery and Fogdestam’s work as a visiting fellow meant that we came in contact with each other regularly, especially since we were both involved in the digit replant6 and free-flap program and were working on projects in the microsurgery laboratory.7 We soon became friends. Ingemar’s training involved an experimental scanning electron microscopy project on microvascular anastomoses,8 experimental and clinical lymphaticovenous microsurgery,9 and participation in the very first operation using the wrap-around principle for thumb reconstruction.10
During the year of Ingemar’s fellowship, Johanson visited the centre to see how he was getting on. Johanson had another purpose in mind too. He was well aware of the limited options for breast reconstruction available to women who had undergone a mastectomy. At the time the main reconstructive option was by means of a multistage pedicled flap from the abdomen, first attached to the wrist to enable movement up to the chest and then transferred to the breast area—a procedure that took several months to complete, was extremely taxing on the patient and had a very uncertain outcome.11 Understandably, it was not often performed.
Johanson had been thinking of another approach to the problem and he felt that microsurgery might hold the key. After the breakthroughs in 1973, free flaps were beginning to be used to reconstruct a variety of defects.12 With this approach, donor tissue is completely detached on a vascular axis and transferred to the recipient site where circulation is re-established by anastomosis of the arteries and veins. Johanson had experience of the multistage tube pedicled abdominoplasty flap in breast reconstruction and was well aware of its drawbacks. The question occurred to him: Why not apply the free-flap approach to breast reconstruction? And why not source the flap from the same site as used in the tube pedicled flap procedure—the abdomen? For breast reconstruction after radical surgery a large supply of tissue is required and the abdomen, unlike most other possible sites, is amply suited to supply this.
Johanson met with O’Brien and was impressed with what he saw at St Vincent’s. While he was there, he took Ingemar aside and instructed him to investigate the practicality of transferring a free flap from the abdomen to the breast and to design a procedure to accomplish this. As the microvascular work involved would be a two-person job, Ingemar approached me to ask if I would assist him. Of course, I agreed.
Although abdominoplasty had been practised for some time, the difference here was that the flap had to be preserved on its blood supply before removal. It was necessary to investigate the vascular anatomy to see whether it was possible to raise it together with a blood supply sufficient to keep it viable once it was removed from its site and transferred elsewhere in the body.
In dissection work carried out in the cadaver laboratory at St Vincent’s, Ingemar and I examined the blood supply of the abdominal tissue (Figure 4). We found two vascular systems—the superficial epigastric arteries and the deep inferior epigastric arteries. The superficial arteries were small, around 1 mm in diameter. Although they were much more conveniently located in the tissue, it was clear that they would not be able to do the job. We then investigated the deep inferior epigastric artery which runs upwards under the rectus abdominis muscle and contains perforators that go through the muscle and supply the overlying skin. This artery was 2–3 mm in diameter, much more suitable to our purpose, but posed a challenge because the ramifications of the vessels, now termed perforators, passed through the muscle. We could have taken the abdominal tissue together with the underlying muscle and blood supply but that would have meant sacrificing the rectus muscle and we did not want to do that. Our solution was to come in under the muscle to locate the inferior artery and then to raise the flap together with a section of the artery plus the perforators with just a cuff of muscle around them. This worked in the lab and the results satisfied us that we had come up with a practical approach.
Ingemar Fogdestam, July 2019, Gothenburg, Sweden
When I returned to Sweden after my year’s fellowship in Australia, I set up the country’s first microsurgical service at Sahlgrenska University Hospital as planned. For such a service you need to have a minimum of two surgeons comprehensively trained in the field, so to give microsurgery a flying start I asked Dr Richard Hamilton if he would join me in Sweden.
In Gothenburg we continued our research into the new breast reconstruction technique using in vitro angiography to ascertain that the blood supply provided by the inferior epigastric artery would be adequate to keep the island flap viable. We raised an abdominoplasty flap in the cadaver laboratory, cannulated the deep inferior epigastric artery and injected barium sulfate. Under x-ray it was clear that the barium sulfate was evenly distributed throughout the tissue. This confirmed the feasibility of our approach—all that remained was to put it to the test in the theatre (Figure 5).
In late 1978 Associate Professor Hans Holmström, second in charge of our unit under Johanson, instructed us to perform the procedure on two patients who had recently undergone radical mastectomy for breast cancer. So in December, with Holmström present, we attempted the first breast reconstruction using a free abdominoplasty flap. Naturally we used instruments we had brought with us from Australia: the O’Brien clamp (which I had modified so that it was double-ended), the O’Brien needle holder and jeweller’s forceps no 2 and no 5 (specified by O’Brien).12
Unfortunately, the patients were not ideal for such a pioneering operation, being irradiated Halsted radical mastectomy patients. The first procedure was a failure because of venous thrombosis in one of the patient’s anastomosed veins. However, the second operation in 1979 was a complete success. The work we had done in Australia—the clinical microsurgery at St Vincent’s and the anatomical research in the hospital laboratory—had led to a breakthrough operation in Sweden (Figure 6). The new procedure would change breast reconstruction from an operation that was so taxing and uncertain as to be rarely carried out, to one that was so straightforward that it would soon be performed routinely all over the world. It should be noted that it preceded the pedicled TRAM flap by some two years.13
Until now, there has been little understanding of the Australian contribution to this pioneering operation and the work done by Hamilton and myself.14 Hopefully in the 40th anniversary year of this historic operation, this perspective—in a new Australasian journal—will go some way towards providing the hidden story behind the procedure and Australia’s important contribution will finally be understood.
Disclosures
The authors have no conflicts of interest to disclose.
Funding
The authors received no financial support for the research, authorship and/or publication of this article.
Revised: November 26, 2019 AEST
Updated: June 17, 2021 AEST (new formatting and pagination)
_performs_the_pioneering_operation_in_decem.jpg)




_performs_the_pioneering_operation_in_decem.jpg)