Introduction
Operating room fires are imminently preventable, devastating events with physical and psychological consequences that can last a lifetime for patients. They also represent a potential cause of litigation.1–3 The vast majority of surgical fires occur during surgery of the head and neck region, including plastic surgery (both reconstructive and cosmetic), ophthalmology, otolaryngology, maxillofacial surgery and neurosurgery.2,4–10 The face is the second most common surgical site injured by surgical fire accidents, with only fire during tonsillectomy being more common.11
A survey of personal experiences of surgical fires by members of the American Society of Ophthalmic Plastic and Reconstructive Surgery reported that 43.5 per cent of surgeons have had at least one operating room fire.8 In the USA, the prevalence of surgical fires has been estimated at approximately 600 events per year.12,13
A recent event in our institution was the stimulus for this review. The patient’s face caught fire during excision of a skin cancer. Interestingly, the flame was very subtle and it took some time to recognise. The presence of sedation also meant that the patient’s response was not immediate. These points underpin the importance of awareness and prevention in these situations.
The increasing numbers of day surgery procedures performed on the face under local anaesthesia with intravenous sedation increase the potential risk of fire accidents. The main reason for this is that the three components of the ‘fire triangle’ are in close proximity around the airway. The key to fire safety and prevention is an awareness of the risks.
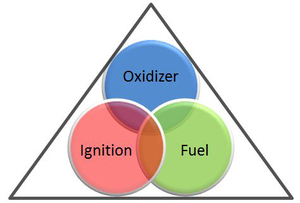
Fire triangle
A surgical fire is defined as a fire that occurs on or in a patient. An airway fire is a specific type of surgical fire that occurs in a patient’s airway.1,12 Fire requires the presence of three components: an oxidiser, an ignition source and fuel,2,8–10,14,15 (Figure 1). Together these are known as the ‘fire triangle’ or ‘fire triad’.
There are many different types of oxidisers, ignitors and fuels documented in the literature. This review seeks to highlight causative factors, detail preventive measures and raise surgical staff awareness of this hazard.
Methods
The review was conducted according to the PRISMA search criteria and checklist (Figure 2).
Sources of information
A literature review was performed using PubMed and MEDLINE® search engines. Search terms included ‘operating room fire’, ‘theatre fire’, ‘surgical fire’, ‘fire triangle’, ‘fire triad’ and ‘oxygen enriched atmosphere’, with the search covering the 25 years from 1993 to 2018. The popularity of plastic surgery procedures as day surgery under sedation during the last two decades corresponds to the increase in burn accidents; accordingly, most of the literature covering surgical fires under sedation has been published during the last 25 years.
Inclusion and exclusion criteria
No randomised controlled trials about causes and prevention of fire are available. Therefore, prospective experimental laboratory and manikin trials were included in addition to case reports and case series with precise event descriptions. Relevant articles from references in the selected studies were also included, as were non-clinical experimental studies exploring fire risks in the operating theatre environment.
The literature search identified 414 published studies. Excluded articles pertained to surgical fires under general anaesthesia, those occurring in regions other than the face, fires related to use of laser, and those occurring in surgical craft groups other than plastic surgery (Figure 2).
After applying inclusion and exclusion criteria, 30 articles remained for the purpose of this review.
Results
Our review of the literature produced an extensive list of different materials that can act as a fuel for surgical fire if an igniting source sparks in the presence of an oxidiser. For a procedure performed on the face under sedation, high-flow oxygen supplementation together with electrocautery is the most common combination of factors predisposing to surgical fire.
Oxidisers
The oxidiser component of the fire triangle is so important to fire creation that it is unusual for a surgical fire to occur in the absence of oxygen enrichment.6 Oxygen-enriched environments occur far more frequently around patients receiving supplemental high-flow oxygen (> 3–4 L/min) compared with those receiving supplemental oxygen at low flow rates (2 L/min).2,7,8,16,17
The proximity of the oxidiser to the ignition source plays an important role,7,8 as does the way the oxygen is delivered in creating an oxygen-enriched environment. Malpositioned nasal cannulae and facial masks are associated with the highest risk, followed by properly placed nasal cannulae, while the lowest levels of oxygen were recorded when nasopharyngeal tubes are used for oxygen delivery.11
Draping can create occlusive tenting and trap oxygen, raising its concentration, and many studies suggested open-drape techniques to avoid oxygen pooling.1,9,17,18
Nitrous oxide also acts as an oxidiser and both increase the likelihood and intensity of combustion in the surgical field in a concentration-related manner.1,2,6
Ignition source
Electrocautery devices are the most common source of ignition.1,6 Cases of surgical fire have been reported when cautery is used in cutting, coagulation and blend modes.19 Electrocautery was used in 90 per cent of fire-related malpractice claims from 1985 to 2009.2
Monopolar devises cause more sparking than bipolar forceps. Likewise, uncleaned diathermy tips covered with crust cause more sparking.6,20 There is a greater risk of fire if the electrocautery device is in close proximity to the oxygen source7,8,12,21 and at a setting higher than 15 Watts (W).7,20
Laser is the second most common cause of operating theatre fire ignition.12 Other ignition sources identified include fibre-optic light cables, argon beam coagulators, drills, burrs and pulse lavage power cords (Table 1).2,8–10,14,18,22
Fuel
Multiple different materials can act as fuel for surgical fires. Some of them are non-inflammable at normal oxygen concentration levels but become a fuel source when placed in an oxygen-enriched environment.5,16 Common materials include surgical drapes, towels, sponges, gauze, dressing materials and gowns with variable levels of flammability.1,5,16 Oxygen masks, nasal cannulae, suction catheters, anaesthetic airway tubing, scavenger tubes and drains are also common fuels.1,9,10,18
Antiseptic skin preparations (especially alcohol-based) are well recognised fuels, particularly with pooling in skin creases and drapes and if not given sufficient time to dry before commencing surgery.1,14,25 Other fuel sources include ointments, benzoin tinctures, phenol, petroleum-based lubricants and degreasers.2,5,9,10,18 Desiccated tissue and hair (including lanugo hair) can be combustible (especially if the hair contains hairspray or hair gel).8–10,23
Catgut and sometimes nylon sutures are stored in solutions containing isopropyl alcohol, which can be a potential fire risk.18 Monopolar diathermy needle insulators made of polytetrafluoroethylene have also been reported as a fuel source in a case report (Table 2).19
Discussion
Day surgery procedures under assisted local anaesthesia facilitate faster turnover of a theatre list. This has been associated with reduced costs of healthcare provision, hospital stay and possible complications related to general anaesthesia. The use of intravenous sedation is common during these procedures and may require supplemental oxygen therapy to prevent desaturation. The presence of oxygen (oxidiser) and an electrocautery device (ignition) in the area around the airways is the primary risk factor for surgical fires in facial surgery.4,8
Skin preparation
The presence of alcohol in skin preparations is a main cause of surgical fire, especially if it is not left to dry before commencing surgery. A study by Jones and colleagues on porcine dermis using different types of skin preparations showed that alcohol-based preparations (chlorhexidine-isopropyl alcohol and iodine-isopropyl alcohol) created fires if ignited immediately after application and to a lesser extent after three minutes’ delay in room air (21% oxygen concentration).14 On the other hand, non-alcohol-based preparations (povidone iodine 1% and chlorhexidine gluconate 4%) did not lead to fire under similar conditions. The study showed that pooling of the alcohol-based preparations in skin folds or drapes increases the risk of fire.14 Other studies have confirmed the safety of non-alcohol-based preparations.25
Draping
Drapes have a dual role in initiating burns. They can both act as a fuel source and trap oxygen, creating an oxygen-enriched environment if applied in an occlusive manner over the oxygen source.
Flammability differs from one material to another, with polypropylene drapes being less flammable than cellulose drapes. In all cases the time to ignite shortens with higher oxygen concentrations.12 Culp, Kimbrough and Luna tested the flammability of surgical drapes and other fuel sources in room air and in oxygen-enriched environments.16 They found that utility drapes and surgical gowns (95% polypropylene) did not burn in room air (21% oxygen concentration), compared with surgical drapes (80% polypropylene and 8% polyethylene) and both laparotomy sponges and blue towels (100% cotton), which ignited and burnt. At 100 per cent oxygen all tested materials ignited and burnt.16,18 In another study all four types of drapes studied ignited at 21 per cent, 35 per cent and 100 per cent oxygen but the time to ignition was longer when lower concentrations of oxygen were used.5 Studies also showed that drapes labelled ‘fire resistant’ or ‘non-flammable’ can ignite in an oxygen-enriched atmosphere.5,12
Oxygen-enriched environment
The term ‘oxygen-enriched environment’ is used for any atmospheric concentration of oxygen greater than room air (namely 21–23.5%)1,17,24 or a partial pressure greater than 21.3 KPa.22
Studies assessing different variables associated with the oxidiser contribution to surgical fires confirm that oxygen flow rate, duration of oxygen supplementation, pooling of oxygen under drapes and the distance between the oxidiser and the ignition source are all interacting contributing variables. Reyes and his colleagues determined the minimum conditions for combustion while supplemental oxygen was administered during facial surgery.7 In their experiments, they demonstrated that a nasal cannula ignited at a minimum coagulation level of 30 W, an oxygen flow of 2 L/min and a linear distance of 5 cm from the oxygen source.7 In general, oxygen concentration increases when oxygen flow is increased,17 and a minimum flow of 2 L/min has been shown to be enough for ignition in experimental models,7,21 especially if the nasal cannula is placed under the drapes.17,18
Experiments on the effects of draping technique have shown that oxygen concentration beneath the drapes was found to be consistently elevated when compared with the estimated delivered oxygen concentration.13,17,26 Supplemental oxygen leads to pure oxygen accumulating in the more basal regions covered by the surgical drapes. Oxygen is of a higher specific gravity than room air and this results in oxygen pooling in a dependent location.12,26 Experiments by Tao and colleagues showed that higher oxygen levels are detected at the corners of the mouth compared with the centre of the face when open face draping is used with a nasal cannula.26 It took 30 seconds after cessation of supplementation to reach lower levels in open draping compared with 60 seconds for closed draping techniques (at a rate less than 3 L/min). As mentioned above, the pooling effect increases the combustibility of materials near the surgical field.13,17
A study of the concentration of oxygen at different facial landmarks recommended keeping the ignition source at least 10 cm from the nasal cannula if the flow rate is 4 L or more.21
Malpositioned nasal cannulae are associated with higher fire risk in open draping experiments.7,8 The use of face masks is less favourable than nasal cannulae as they create a pocket of oxygen over the mouth and nose which might leak through gaps between skin folds and the edge of the mask to areas within less than 5 cm of the cautery and fuel sources.8
Use of closed face draping increases the risk of burn by creating a local oxygen-enriched environment.2 Open face draping is recommended in many studies1,2,8,9,18 and use of suction decreases the level of oxygen in the surgical field.13,15 Tao and colleagues achieved lower oxygen levels using a midfacial seal drape for an oculofacial surgical field compared with an open face drape.26 They used a drape with an adhesive seal across the nasal bridge and midface covering the nasal cannula and along the malar eminence to the angle of the mandible.26 Although the experiment showed lower oxygen levels (21–22%) outside the drape area (around the orbit), oxygen levels under the drape were high (59– 73%), producing an oxygen-enriched environment with potential risk if any leak happened during surgery if the drape seal was breached at the skin or drape folding points.26
Meneghetti, Engel and colleagues achieved a reduction in oxygen concentration in the operative field when the cut ends of the nasal cannula were passed down a rubber nasopharyngeal tube into the posterior pharynx compared with using a nasal cannula in the standard manner. The study showed that this oxygen delivery method reduced the oxygen concentration in the operative field to a level consistent with ambient air.11,27 The nasopharyngeal tube was used only in deeply sedated patients to avoid pharyngeal irritation being felt by the patient.27 Contrary to these findings, another study showed no advantage to the use of nasopharyngeal tubes compared with nasal cannulae, and patients experienced discomfort when using nasopharyngeal tubes.17
Ignition (heat) source
Diathermy is the most common type of therapeutic equipment involved in burn incidents.12,26,28 An experimental study comparing the power of electrocoagulation required to ignite a fire at different distances from a malplaced nasal cannula has shown that at an oxygen flow rate of 2 L/min, 30 W of coagulation level created a burn 5 cm from the malplaced nasal cannula.7 Other experiments showed that electrocautery at 15 W did not ignite any fire when the oxygen concentration was below 50 per cent.20
Buildup of a crust on the tip of an electrosurgical device can contribute to increased heat and in turn to increased fire risk.20
Monopolar and thermal hand-held cautery were the most common devices associated with fire accidents compared with bipolar cautery and carbon dioxide laser.8,10 Case reports have suggested the ‘spray’ modality of electrocautery to be a contributing factor,29 however, no definitive evidence in the literature supports this assertion.
Fire accidents during general anaesthesia
Although outside the scope of this literature review, plastic and reconstructive surgeons may face a similar situation when a patient is under general anaesthesia and an uncuffed endotracheal tube is used or a leak occurs around a leaking or inadequately cuffed tube during airway surgery, as in intraoral, maxillofacial and cleft surgeries.2,19 The same principles of surgical fire prevention should be followed in such situations.
Tracheostomy during head and neck reconstructive procedures is another example of a high-risk situation under general anaesthesia, as an oxygen leak into the surgical field is always present during tracheostomy once the trachea has been incised. Cauterising a bleeding vessel or performing further dissection using electrocautery increases the risk of fire at this stage of the procedure.2,24 It is safer not to enter the trachea with an ignition source; if an electrocautery device must be used, the surgeon should provide adequate warning to the anaesthesiologist to enable the oxygen concentration to be minimised before the trachea is entered.1
Recommendations
The accumulated experience of surgical fires and the conditions that predispose to them have led to many sets of recommendations in the literature. We present a consensus summary of these findings to guide the practice of plastic surgeons.
Identification of risk
A high-risk procedure is one in which an ignition source is in close proximity to an oxygen-enriched atmosphere, thereby increasing the risk of surgical fire.1 The three arms of the fire triangle are under the control of different members of the surgical team: the anaesthetist controls the oxidiser, nursing staff control the potential fuel sources and the surgeon controls the ignition source.22 Team communication regarding fire risk and prevention is an important component of the pre-surgical checklist or ‘time out’, as well as intraoperatively.2,6,8,9
Oxidiser
Indications for supplemental oxygen
Oxygen supplementation should not be considered as routine for all cases.8,18 Oxygen saturation levels should be continuously monitored to determine the lowest possible oxygen concentration that can be administered to achieve near-preoperative oxygen saturation levels.1,8,18 The indications for oxygen may include preoperative comorbidities such as cardiopulmonary, vascular or haematological disease or desaturation induced by deep sedation.17
Use of compressed air
If the patient is not oxygen dependent and can maintain a safe saturation level then compressed air can safely replace oxygen use.1 If deep sedation is required, or if the patient is oxygen dependent, the anaesthesiologist should consider a sealed gas delivery device (cuffed endotracheal tube or laryngeal mask, which includes general anaesthesia).1,2
Use of supplemental oxygen
When indicated, oxygen supplementation should be administered intermittently when an electrosurgical unit is not in use.12 Keep the oxygen flow rate low (2–3 L/min) and cease supplementation 60 seconds before starting electrocautery.2,8,12,17 The FiO2 should be kept as low as possible (less than 30%) well in advance of electrosurgical unit use.6,9,16,19,20
Supplemental oxygen delivery
Avoid using face masks to deliver supplemental oxygen. Nasal cannulae are safer8,12 but they should be properly placed7,18 and never covered by drapes.1,2,8,9,18 Use of a scavenger system reduces the risk.2,8,13
Nasopharyngeal tubes may show a reduction in oxygen concentration in the operative field in comparison with nasal cannulae,11,27 but avoid their use in a lightly sedated patient due to discomfort.27
Ignition
Electrocautery/heat source
Use bipolar cautery rather than monopolar8,10 and an electrocautery level less than 15 W.7,20 Keep the diathermy tip as clean of crust as possible.6,20 Hold the cautery device a minimum distance of 5 cm from the oxygen source,7,8 or 10 cm if the flow is 4 L/min or more,12,21 and at all times leave the electrosurgical device in a holster when not in use.12,24 Never leave an endoscopic or fibre-optic cable lying on top of surgical drapes, towels or gauze when the light source is turned on.8
Fuel
Skin preparation
Avoid using alcohol-based skin antiseptics when operating on the face,1,25 instead opt for aqueous-based skin preparations.6,10 If using an alcohol-based preparation, allow it to dry completely before draping.9,10,14,25
Hair
The patient should not use hair spray, gel or perfume preoperatively, and in the operative site hair should be coated with a water-soluble lubricating jelly.10,23,25
Draping
Use flame-resistant surgical drapes,9 polypropylene surgical drapes are recommended,8 and avoid the use of cotton products as drapes or gowns.16 The majority of publications favour open face draping rather than closed face draping.1,2,8,9,18 Fenestrated drapes can act as closed face draping and should not cover the oxygen source. Moist towels can be used to drape out the eyes if needed.18
Sponges
Moisten all swabs and sponges before use1,6,15 and keep all flammable products away from the surgical site at time of electrosurgery.
Extinguisher
Keep a carbon dioxide fire extinguisher in the operating theatre (with all staff regularly trained in its use)6,10,24 and a bowl of normal saline on the surgical instruments trolley at all times.10,12,30
Awareness and education
Operating theatre fire drills, involving a formal rehearsal with the entire theatre team and including simulation and training on surgical fire, should be conducted regularly.21 Maintain awareness using posters in the operative room.6
Conclusion
An integral causative factor in all surgical fires is human error. The risk of such a catastrophic complication can be mitigated by separating the elements of the fire triangle from each other. The use of supplemental oxygen at a high flow rate and electrocautery are the main instigators in most surgical fires. Risk identification and awareness of the different roles played by surgical, anaesthetic and nursing staff are crucial in surgical fire prevention. We recommend a checklist of 10 points to be considered during the preoperative time out process whenever surgery is planned to be conducted under sedation with the use of supplemental oxygen and electrocautery (Figure 3).
Conflict of interest
The authors have no conflicts of interest to disclose.
Funding declaration
The authors received no financial support for the research, authorship and/or publication of this article.
Revised: April 13, 2019 AEST