Introduction
The Victorian Adult Burns Service (VABS) based at The Alfred Hospital, Melbourne, Australia serves as the major adult burns centre for the state of Victoria. A common pattern of patients presenting with burns related to the use of petrol was noted. An accelerant is a substance that aids the spread of fire or increases the intensity of a fire. Accelerants include substances such as petrol, diesel, liquefied petroleum gas (LPG), propane, kerosene, paint, glue, paint thinners, lighter fluids, turpentine and fertiliser.1–3 Burns fuelled by accelerants are a major cause of injury in Australia and New Zealand.1,4,5 Accelerants, especially petrol, are readily available and commonplace in both domestic and commercial environments. The same quality of explosive ignition that makes a flammable liquid so valuable as a fuel can cause injuries when it is handled carelessly or used for a purpose for which it is not intended, such as directly adding petrol to a fire.
This study aimed to quantify the incidence of petrol use related to burn injuries within Victoria and to define the characteristics of patients affected by these injuries in order to better direct resources and patient education towards identified groups.
Methods
The VABS maintains a database of patient details to contribute to the Burns Registry of Australia and New Zealand (BRANZ). This clinical quality register captures epidemiological, quality of care and outcome data from adult and paediatric burn patients across Australia and New Zealand burns units (16 of 17 burns centres). Ethics approval was obtained from The Alfred Hospital’s health human research ethics committee to interrogate the database.
This was a retrospective cohort study that examined demographic data, specific burn characteristics, treatment data and geographical location of burn incident for patients with petrol-related burn injuries admitted to The Alfred Hospital. Data were extracted from the VABS database on patients presenting over a seven-year period, between 1 July 2009 and 30 June 2016. Data collected were analysed using Microsoft Excel Version 16 and GraphPad Prism Version 7.
Postcodes recorded in the database as the geographical location of burn incidents were classified into local government areas (LGAs), which were used to determine the rurality of the burns incidents. Maps were created using online map-generating software from the Australian Urban Research Infrastructure Network (AURIN) (https://aurin.org.au).
To calculate the potential financial cost of petrol burns in Victoria, the formula described by Ahn and Maitz in 20126 was used (y = 10.08x 3–625.71x 2+13584.25x) where y is the total cost per patient and x is the average percentage total body surface area (TBSA) burn recorded as part of our study.
Approved by The Alfred Hospital health human research ethics committee [2017-9850-11501].
Results
During the study period, 378 out of 1927 burns admissions were related to petrol use, with a mean of 54 patients per year, accounting for 19.6 per cent of the total burns admissions. Of the patients with petrol-related burns, 331 (87.6%) were males and 47 (12.4%) were females. Males aged 20–29 years were most at risk, contributing to 25.4 per cent of all petrol-related burn injuries (Table 1).
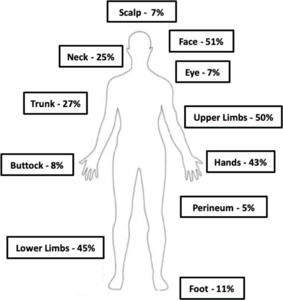
Fifty-nine per cent of patients sustained burns between 0 and 9 per cent of TBSA and 23 per cent had more significant burns between 10 and 19 per cent of TBSA. Analysis of burn depth showed that 171 patients (45.2%) had a superficial component to their injury recorded in the database. The anatomical location involved for petrol-related burn injuries is depicted in Figure 1. The most common areas affected were the face (51% of burns), the upper limbs (50% of burns) and the lower limbs (45% of petrol-related burn injuries).
The event surrounding petrol-related burn injuries was most commonly classified as a leisure activity (31.0%) followed by ‘other activities’ (11.4%) and self-harming (10.3%). Alcohol use was reported in 21.2 per cent of injuries and drugs alone were reported in only 2.4 per cent of cases (Table 2).
The average length of hospital stay for patients with petrol-related burn injuries increased as the percentage of the TBSA burn increased, peaking at 39.8 days for males and 86 days for females with a TBSA burn of 40–59 per cent. In the 80–100 per cent TBSA burn group, the average total length of hospital stay was less than one day because of the high number of fatalities in this group. Average hours in the intensive care unit (ICU) peaked at 551.6 hours in the 40–59 per cent TBSA burn group. Again, due to mortalities, this declined to 17.3 hours in the 80–100 per cent TBSA burn group. Patients admitted to ICU for ventilation comprised 31.5 per cent of the total, of whom 21.2 per cent had a confirmed airway injury, demonstrated by bronchoscopy. Operative management of burns was required in 70.4 per cent of cases.
Petrol-related burn injuries were associated with a 7.4 per cent mortality rate. In total there were 28 deaths (22 males and six females). Of the individuals who died from their petrol-related burn injuries, 18 (64.2%) sustained their injuries as a result of self-harming.
Reported postcodes for burn incidents are recorded for all patients admitted to the VABS. Plotting the postcodes of burns cases involving petrol in LGAs showed patients presenting from a large geographical area, across the whole state of Victoria (Figure 2). Only 16 petrol-related burn injuries occurred within the Melbourne metropolitan area during the study period.
The mean TBSA burn for our study was 19.3 per cent which, according to the cost formulation by Ahn and Maitz,6 gives a total average cost of AU$101,571 per patient or AU$5,484,834 annually, based on the mean of 54 patients per year.
Discussion
This study aimed to identify the epidemiological factors contributing to patients with petrol-related burn injuries presenting to the VABS based in The Alfred Hospital. Previous studies in Australia, the USA and the UK have shown that the incidence of accelerant-related burn injuries ranges between 18 and 23 per cent, and this is in accordance with the current study where 19.6 per cent of burns involved petrol alone.1,4,5,7,8 However, there is a significant male predominance in this study compared with the current literature, 87.6% vs 67%).1,4,5,7,8
The anatomical areas affected by petrol burns showed a predominance for the exposed skin on the face and limbs, suggesting that the majority of injuries were sustained while facing the fire and were the result of an explosive or flash burn pattern. Anecdotally, patients often described the injury occurring as they were adding petrol to an already established fire. Burns to the face and hands are of increased significance due to the potential for eye injury (7%) and airway injury (21.2%) and the difficulties in reconstructing the specific aesthetic and functional components of these areas.
‘Leisure activity’ was the most common precipitating event for petrol-related burns.5,9 Nearly one-quarter of patients in this study reported being under the influence of drugs and/ or alcohol, which is higher than the 16 per cent reported for all burns in BRANZ.10 A large number of petrol-related burn injuries are attributed to human error1,4 associated with the misuse and unsafe handling of petrol. It is vital to identify and address unsafe practices with petrol as a means of reducing these devastating injuries.1,2,4,5
Environment is an important factor that shapes the epidemiology of burn injuries.1–3 This study highlights that the majority of petrol-related burns occurred in rural and remote areas. It appears that open domestic fires are more commonplace in regional settings, and bonfires, campfires and burning-off occur there more often.1–3
Approximately one-third of patients in our study required admission to ICU for ventilation, with over one-fifth having confirmed evidence of airway injury, demonstrating the severity of petrol-related burn injuries. More than two-thirds of patients required surgical management of their burns. Petrol-related burn injuries were associated with a 7.4 per cent mortality rate, which is significantly higher than the 1 per cent rate for all burns during the same period.10 The majority of these deaths were due to non-accidental injury.
Our study estimates that the cost of petrol burns to Victoria could amount to almost AU$5.5 million annually, not including the cost of patient transfer to The Alfred Hospital. This is a considerable expense in Victoria due to the rural location of the majority of burns cases and the need for air transport in many instances. Our estimate does not include the cost to the individual and to the community in terms of loss of earnings due to inability to work or the irreplaceable deficit due to permanent disability or death.
In Australia, petrol and other accelerants are readily accessible and are often stored in households ready for use in motor vehicles, boats and gardening equipment. The authors advocate and encourage public education campaigns to raise awareness of their potential hazards and the life-changing consequences of their misuse. Another preventive measure is to ensure that accelerant packaging includes obvious labels about the risks of misuse as well as safety features to minimise the risk of spillage.
Limitations
This study does not represent the entire cohort of petrol-related burn injuries in Victoria. It only includes patients with severe enough burns to require treatment in specialised burns units and does not include patients managed in non-specialist centres and the ambulatory setting.
Conclusion
Misuse of petrol around naked flames contributes to a substantial injury burden in Victoria, Australia. Young males from rural areas are the group most likely to be affected by these injuries. Petrol is one of the most common and readily available accelerants being misused around fires. Raising community awareness through preventive strategies targeted at high-risk groups and highlighting hazardous behaviours is warranted to reduce the incidence of petrol-related burn injuries. The authors intend to work with the Country Fire Authority to engage with the media and politicians to develop education campaigns and legislation to target the patient groups identified in this study.
Acknowledgements
The authors would like to acknowledge Samara Rosenblum for her invaluable help in extracting the data.
Disclosures
The authors have no conflicts of interest to disclose.
Funding
The authors received no financial support for the research, authorship and/or publication of this article.
Revised: July 13, 2019 AEST