Introduction
Lipodystrophy syndromes, a clinically diverse group of conditions with selective deficiency of adipose tissue as a central feature, are classified as inherited or acquired, with further sub-classification based on aetiology and clinical features.1 The acquired lipodystrophy subtypes include localised, partial, generalised and HIV-associated.1 Acquired partial lipodystrophy, also known as Barraquer-Simons syndrome, is a rare condition first described in 1885 by Mitchell.2 It is characterised by progressive accumulation of surplus subcutaneous fat in the hips and lower limbs, contrasted with a deficiency of fat in the upper body, as well as metabolic complications of hypertriglyceridaemia and insulin resistance.3 Precise pathogenesis is unclear; however, it is commonly preceded by infection, and reports have implicated tetanus antitoxin, surgery, psychological stress and sunburn.4 Management options are limited1 and scarce literature regarding liposuction in acquired partial lipodystrophy exists, though it has been used effectively in other lipodystrophy syndromes, albeit rarely.5,6 Medical management and large-volume liposuction are effective in improving the metabolic profile of patients without lipodystrophy, as well as cosmesis and quality of life.5,7,8 The removal of large volumes of fat via liposuction is not without potential complications, and postoperative medical management is complex.9,10 We report a case of acquired partial lipodystrophy treated with large-volume liposuction of the lower limbs with subsequent metabolic improvements.
Case
A 29-year-old female with acquired partial lipodystrophy was referred to the plastic surgery team by her endocrinologist for consideration of liposuction. She developed lipodystrophy at age four years following varicella infection.
Her medical history included hypothyroidism, tonsillectomy, adenoidectomy and excision of cervical intraepithelial neoplasia II. Her medications were daily metformin XR 500 mg, thyroxine 50 mcg and the cyproterone acetate/ethinylestradiol oral contraceptive.
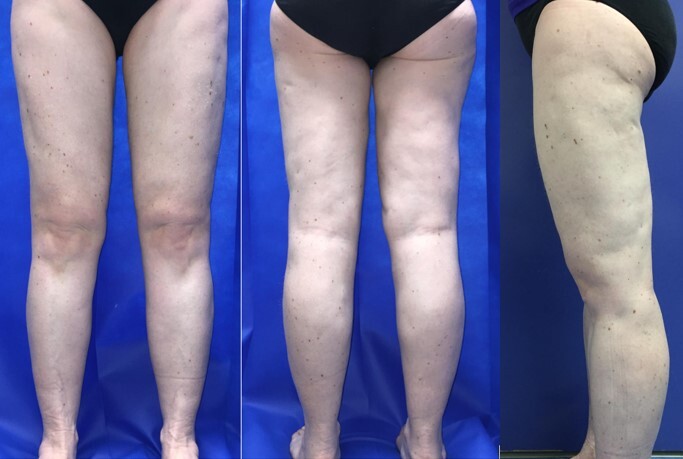
On examination, she weighed 67.5 kg, with significant deficiency of subcutaneous fat in her face, upper limbs and torso. There was excess subcutaneous fat in her lower limbs, with predominance in the upper thighs and sparing of the buttocks (Figure 1). Circumferences were 74 cm at the waist, 60 cm bilaterally at a point 40.0 cm below the iliac crest and 33 cm bilaterally at a point 30 cm above the lateral malleolus.
Biochemical markers showed total cholesterol 6.9mmol/L, low-density lipoprotein (LDL) cholesterol 4.1mmol/L, high-density lipoprotein (HDL) cholesterol 1.5mmol/L and triglycerides 2.8mmol/L. She exhibited hyperinsulinaemia (24.5mU/L), while her leptin level was 25.6ng/mL (reference range 3.7–11.1ng/mL). Liver ultrasound was suggestive of mild fatty infiltration. Following consultation between the plastic surgery and endocrinology teams, consensus for surgery was reached.
The operation involved tumescent infiltration of 10 L normal saline, with a total of 200 mg ropivacaine and 10 mg of 1:1,000,000 adrenaline (epinephrine). Large-volume liposuction of the calves and thighs was conducted via multiple stab incisions with total aspirate of 18,950 mL. The postoperative course had minimal complications, though was prolonged when compared with routine liposuction. She had tender calves but was able to mobilise on postoperative day one. Haemoglobin levels decreased from 116g/L (reference range 110–160) preoperatively to 92g/L postoperatively, though did not require treatment. Myoglobinuria and a transiently elevated creatine kinase (6590U/L) were documented, with renal function remaining normal throughout and recorded abnormal values trending towards baseline prior to discharge on postoperative day five.
There was significant metabolic improvement three months postoperatively (Table 1). She remained on 500 mg metformin XR and 50 mcg thyroxine daily. She weighed 58 kg and her leg circumferences had reduced considerably (Table 1). There was also significant cosmetic improvement (Figure 2).
Three years later revision liposuction was undertaken for a minimal increase in subcutaneous fat, cosmesis and gradually worsening biochemical markers, with total cholesterol 4.7mmol/L, LDL cholesterol 2.5mmol/L, HDL cholesterol 1.1mmol/L, triglycerides 2.5mmol/L and insulin 15.2mU/L. Despite this, her weight remained stable at 57 kg. Her metformin XR dose was increased to 1000 mg daily and she commenced on rosuvastatin 10 mg daily. At surgery, 1700 mL was aspirated, and she progressed to discharge uneventfully.
Discussion
As few as 250 cases of acquired partial lipodystrophy have been reported,1 limiting the literature to individual case reports and small series. However, other lipodystrophy syndromes with similar clinical manifestations have been more thoroughly investigated due to higher prevalence.5,7 In these studies and others, liposuction has improved the metabolic profile of patients, as well as making aesthetic enhancements that improve quality of life.5,7,8
Large-volume liposuction has been defined as aspiration of ≥ 5000 mL, and recommendations of safe maximum aspirate volume vary significantly.9 Postoperative care can be complicated by significant blood loss, venous thromboembolism, fluid shifts and electrolyte abnormalities.9 The key is adequate fluid resuscitation and electrolyte replacement. A series of 631 cases found large-volume liposuction could be safely undertaken if patient selection is judicious, the operation is conducted by an experienced surgeon and postoperative care is meticulous.10 In our case, 18,950 mL was aspirated from a patient with acquired partial lipodystrophy, with biochemical improvements and no major postoperative complications. To our knowledge this is the largest volume liposuction reported in this rare syndrome. The value of the procedure was highlighted by the improvement in physical appearance, biochemical markers and patient satisfaction. Although we were concerned that removal of significant fat mass might worsen the metabolic profile (due to the lack of a ‘sink’ for storing fatty acids), this did not eventuate.
Conclusion
We report the successful treatment of acquired partial lipodystrophy with large-volume liposuction. This resulted in significant biochemical and aesthetic improvements for the patient.
Patient consent
Patients/guardians have given informed consent to the publication of images and/or data.
Disclosures
The authors have no conflicts of interest to disclose.
Funding
The authors received no financial support for the research, authorship and/or publication of this article.