Introduction
A variety of benign tumours affect the subungual region. They encompass solid tumours (glomus tumour, subungual exostosis, enchondroma, haemangioma) and cystic lesions (epidermal and mucoid cysts). Their clinical manifestations are non-specific and diagnoses most often require histopathological confirmation. A surgical approach for the excision of benign subungual tumours has not been described extensively in the current literature. The ideal approach should provide adequate exposure to prevent tumour recurrence and prevent nail deformity.1 The most commonly described approach is the transungual technique, which involves nail plate removal followed by longitudinal incision through the nail bed. It provides good exposure; however, it requires meticulous nail bed repair to prevent nail dystrophy. Alternative approaches aim to reduce the risk of nail dystrophy by placing the incision in the surrounding skin instead of in the nail bed itself. This includes the lateral subperiosteal approach, periungual approach and fish mouth approach. However, while nail preserving, these techniques offer limited exposure thus are associated with a higher risk of recurrence. A less commonly used approach, the nail bed margin, involves nail plate removal and incision along the nail bed margin to avoid iatrogenic injury to the nail bed. In this review, we present different techniques for the excision of benign subungual tumours in relation to tumour location and their outcomes as described in the literature. We also present our experience in the excision of benign subungual tumours.
Methods
Search strategy
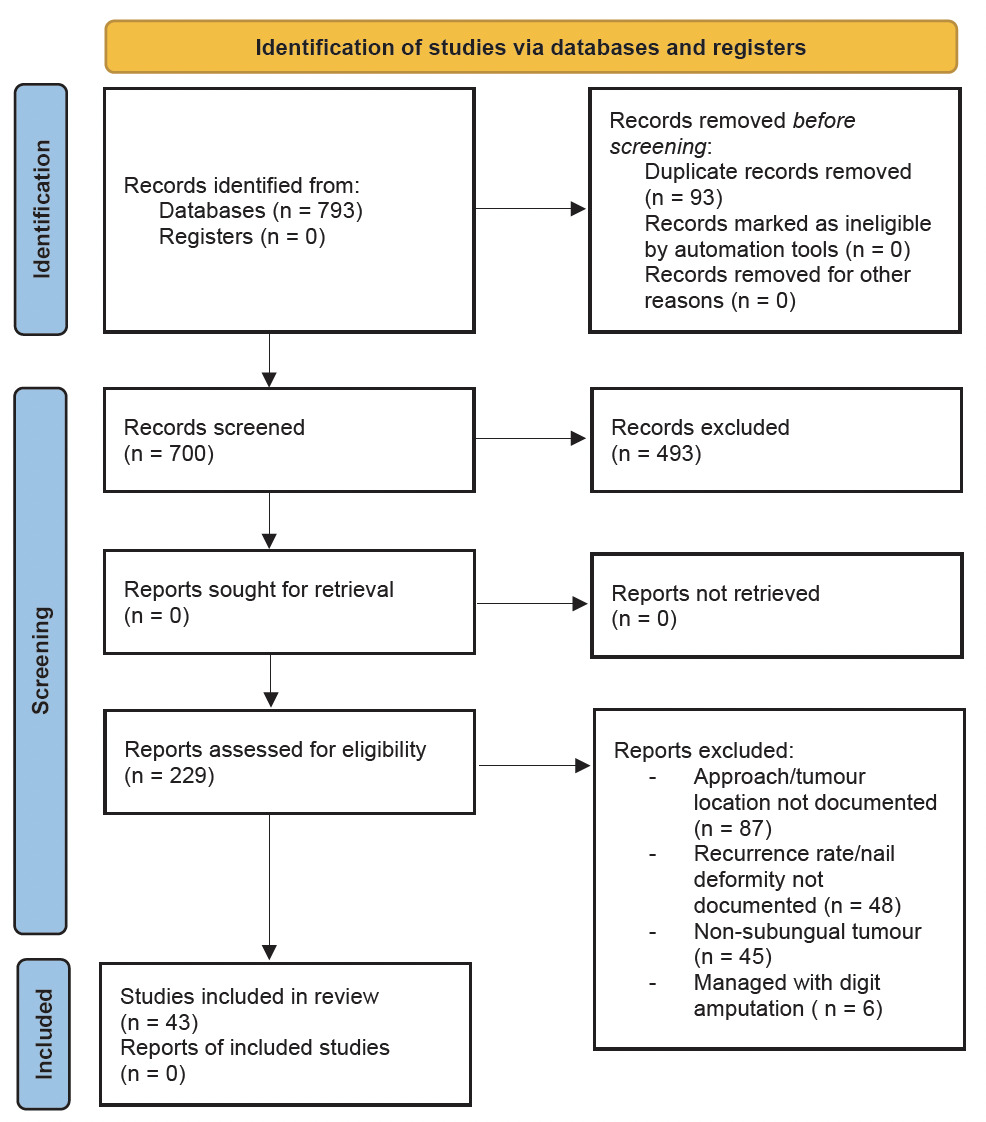
A systematic review of studies evaluating surgical management of benign subungual tumours was conducted using the PubMed database between 1 January 1962 to 31 December 2021. The search terms included ‘glomus tumour’, ‘subungual exostosis’, ‘osteoid osteoma’, ‘fibro-osseous pseudotumour of the digit’, ‘enchondroma’ and ‘implantation dermoid tumour’ of the subungual region. See Figure 1.
Eligibility criteria
The following inclusion criteria were applied: 1. Studies published in the English language that describe the surgical approach to excision of benign subungual tumours 2. Studies that document tumour location in relation to nail bed, and 3. Studies that report the rate of recurrence and nail dystrophy postoperatively. Exclusion criteria were studies that did not document the surgical approach or tumour location, cases treated with digit amputation, and cases with follow-up of less than six months.
Data extraction
After the removal of duplicate studies and non-English studies, we analysed abstracts of 700 articles. Subsequently, we excluded 206 studies that did not document surgical approach, tumour location, recurrence rate and postoperative nail deformity. We also excluded tumours that were managed with digit amputation and those with less than six months of follow-up. We then assessed the full text of 21 studies and identified 228 participants who are included in this review.
Results
Included studies
We initially identified a total of 793 studies on excision of benign subungual tumours. There are five techniques described in the literature that have been used for excision of benign subungual tumours: transungual,1–18 lateral subperiosteal,9,19,20 periungual,13,18 nail bed margin21 and fish mouth.22,23 In terms of tumour location, there is heterogeneity in describing subungual tumour location, which are sterile matrix, germinal matrix, matrix, nail bed, peripheral, central and distal phalanx. For the purpose of this study, the following terms are interchangeable—sterile matrix/nail bed and germinal matrix/matrix.
Tumour location
There is heterogeneity in included studies when describing subungual tumour location, which are distal phalanx, sterile matrix, germinal matrix, central and peripheral.
Types of approaches and outcomes
We identified five techniques from our systematic review, which include transungual, lateral subperiosteal, nail bed margin, periungual and fish mouth. Outcomes are measured using the rate of postoperative nail deformity and rate of tumour recurrence (summarised in Table 1).
The transungual approach is the most commonly used technique in the literature (152 patients).1–18 Fifty per cent of tumours excised with the transungual approach were located centrally, 34 per cent were located in the sterile matrix, 15 per cent were in the germinal matrix and one tumour is in the distal phalanx. Tumours located in central subungual area and sterile matrix showed good postoperative outcome for nail deformity (9.2%), recurrence for central tumours (2.6%), nail deformity (5.7%) and recurrence for sterile matrix tumours (1.9%). However, excision of tumours in the germinal matrix using the transungual approach showed a high rate of nail deformity postoperatively (47.8%; 11 of 23 participants).
Lateral subperiosteal approach was the second most popular alternative (34 patients).9,19,20 The majority of tumours were peripheral (62%), while the rest are located centrally (21%), in the germinal matrix (15%) and in the distal phalanx (2%). Postoperatively, there was no nail deformity or tumour recurrence with this approach.
The nail bed margin approach was used in 17 patients with varying tumour location,21 including peripheral (59%), central (24%) and germinal matrix (17%). There was no postoperative nail deformity or tumour recurrence observed with the nail bed margin approach.
The periungual approach has been described to excise peripheral tumours in 23 patients,13,18 while the fish mouth was used for distal phalanx tumours in two.22,23 Both of these techniques showed no postoperative nail deformity or tumour recurrence.
Cases
A total of six participants underwent excision of various benign subungual tumours at our institution with surgery performed by the senior author. Five participants underwent excision using the transungual approach and one participant using the periungual approach. Three out of five tumours excised using the transungual approach were located centrally. The periungual approach was used to excise a peripheral tumour in the germinal matrix.
All participants were followed up for more than six months postoperatively, with no recurrence and nail dystrophy at final review. See Table 2.
Discussion
A variety of benign lesions affect the subungual region. Their clinical manifestations are often non-specific and diagnosis is confirmed by histopathology following excision or biopsy.24 Several approaches have been described to provide maximum tumour exposure ensuring complete tumour removal, while balancing risk of nail deformity postoperatively.
Our systematic review found various surgical approaches for excision of benign subungual tumours which can be categorised into transungual, lateral, periungual, nail bed margin and fish mouth incisions. Some of these approaches have been developed and are only recommended for tumours in specific locations, such as proximal tumours25 and peripheral tumours.18 However, we note that there is heterogeneity between studies when describing tumour location; some report tumour location in relation to sterile and germinal matrix, others describe whether the tumours are central or peripheral on the nail bed. Several studies report tumour location as ‘distal phalanx’.
The standard or traditional approach is the transungual approach which involves removal of nail plate, followed with a longitudinal incision over the nail bed directly over the tumour. Once visualised, the tumour is excised and nail bed repaired.25 The nail plate can then be replaced over the nail bed repair depending on the surgeon’s preference. The transungual approach offers excellent exposure of tumours and assists in complete removal, thus reducing the risk of recurrence.25 The disadvantage of this technique includes damage to the nail bed, which increases the risk of postoperative nail deformity, such as longitudinal ridge or complete split nail deformity.25 The transungual approach has been most commonly used for tumours located in the sterile matrix (52 tumours) and centrally located (76 tumours). For tumours in these locations, there is minimal postoperative nail deformity and recurrence reported (5.7% nail deformity and 1.9% recurrence for sterile matrix tumours; 9.2% nail deformity and 2.6% recurrence for centrally located tumours). When used for germinal matrix tumours, the transungual approach results in 4.3 per cent of tumour recurrence and 47.8 per cent postoperative nail deformity.
Several studies have described modification of the transungual approach. The nail-preserving transungual technique involves making an incision over nail folds from bilateral proximal nail corners of the nail groove diagonally. The proximal nail plate is retracted upward, leaving the distal nail plate intact. Lee and colleagues25 use a longitudinal incision over the nail bed to expose and excise a subungual glomus tumour in 34 patients. The proposed advantage is minimising damage to the nail bed thus preventing future nail deformity. They reported 6 per cent recurrence rate with no nail deformity at the 33-month postoperative follow-up. However, this approach is recommended to be used in proximally located tumours only.
Another modified transungual technique is the no-nail extraction approach,16,17,26 which involves making an incision on the nail-nail bed complex together over the tumour to perform nail bed splitting without nail plate extraction to expose and remove the tumour. Following which, the nail bed spontaneously reapproximates and thus a nail bed repair is not required. Trans nail suture is then applied. The proposed advantage is less operative time and less postoperative pain as the nail is not extracted. The approach was used in two studies (21 participants)17,26 on glomus tumours and a case report on fibro-osseous pseudotumor of the digit (FPOD),16 which reported no nail deformity and no recurrence.
The nail plate avulsion technique11 is a variation of the transungual approach, which involves avulsion of one side of the nail plate, leaving the contralateral side intact. This approach offers the advantage of minimal postoperative nail deformity.
The second most commonly used approach is the lateral subperiosteal technique. This approach involves making a dorsal incision to the mid-lateral line. Dissection is performed down to the distal phalanx and the dorsal flap is raised (comprising nail bed, matrix and nail plate). The flap is then replaced at the end of the procedure. The technique is nail preserving; however, it offers limited access, thus there is a higher rate of recurrence (15.7%).27 Garg and colleagues20 describe a modified lateral subperiosteal approach, which involves a high mid-lateral incision extended distally and curved around the pulp. In comparison to the traditional lateral subperiosteal, this modified approach offers better exposure as well as nail preservation.
Next, the periungual approach involves an incision over periungual skin and dissection to distal phalanx. The dorsal flap is then raised, containing the nail bed, matrix and nail plate. The periungual technique is comparable to the lateral approach in terms of risks and benefits—preservation of the nail with limited access. Two case series conducted on glomus tumours showed no recurrence and no nail dystrophy at follow-up.13,18 They recommended the periungual technique for excision of peripheral subungual tumours.
Another approach described in the literature is the nail bed margin approach, which involves removal of the nail plate, followed by a curved incision near the side of the tumour along the nail bed margin. Dissection is carried down to the distal phalanx and a dorsal flap is raised (containing nail bed and matrix). Proximal and one lateral attachment is maintained. After tumour excision, the flap is then replaced. Advantages include good tumour exposure, prevention of nail bed splitting and retraction of interosseous ligament of distal phalanx and minimal scar due to the hidden incision. Disadvantages include removal of the nail plate, which results in longer recovery time and pain during dressing change.21
Lastly, a fish mouth incision has been described in two case reports,22,23 which involves a bilateral mid-lateral incision over the fingertip. The dorsal and volar flap are raised and the epithelial bed is dissected from the bone. Advantages include a reduced risk of postoperative nail deformity as the nail bed is left intact. Disadvantages include limited exposure, thus a higher risk of incomplete excision.
We used the transungual approach in five of our patients with a variety of benign subungual tumours of various locations (three involving germinal matrix and two involving sterile matrix). None of the five patients had a recurrence or nail deformity at the final follow-up. One patient has a peripherally located germinal matrix tumour which we excised using the periungual approach. At the 18-month follow-up, she had no nail dystrophy or recurrence.
Our experience suggests that the transungual approach provides appropriate exposure for both central and peripherally located tumours in germinal and sterile matrix. Postoperative nail dystrophy could be avoided by meticulous repair of the nail bed.
Limitations
Limitations of the study include heterogeneity in describing tumour location as well as small population for techniques other than the transungual approach.
Conclusion
Several approaches have been described in the literature for excision of benign subungual tumours, namely transungual, lateral subperiosteal, periungual, nail bed margin and fish mouth. The transungual approach is the most widely used technique. It offers maximum tumour exposure; however, it is associated with a risk of postoperative nail dystrophy. This risk can be minimised by meticulous repair of the nail bed.
Acknowledgement
Dr Andrew Ryan for providing histology reports.
Patient consent
Patients/guardians have given informed consent to the publication of images and/or data.
Conflict of interest
The authors have no conflicts of interest to disclose.
Funding declaration
The authors received no financial support for the research, authorship and/or publication of this article.
Revised: December 3, 2022 AEST

_(a)_preoperative_appearance_of_subungual_glomus_tumour_with_pinpo.jpg)
_(a)_preoperative_appearance_of_a_tender_fibro-osseous_pseudotumor.jpg)
_(a)_preoperative_appearance_of_tender_implantation_dermoid_tumour.jpg)
_(a)_preoperative_appearance_of_asymptomatic_linear_dark_mark_on_f.jpg)
_(a)_preoperative_appearance_of_tender_lump_just_medial_to_fingern.jpg)
_(a)_preoperative_appearance_of_subungual_glomus_tumour_with_pinpo.jpg)
_(a)_preoperative_appearance_of_a_tender_fibro-osseous_pseudotumor.jpg)
_(a)_preoperative_appearance_of_tender_implantation_dermoid_tumour.jpg)
_(a)_preoperative_appearance_of_asymptomatic_linear_dark_mark_on_f.jpg)
_(a)_preoperative_appearance_of_tender_lump_just_medial_to_fingern.jpg)