Introduction
Secondary breast cancer-related lymphoedema is a common condition that afflicts 15–25 per cent of patients who undergo lymph node dissection during axillary clearance (ALND) or 5–7 per cent of patients with sentinel node biopsy (SNB).1,2 Lymphatic fluid stasis in the interstitial space results in the obliteration of the lymphatic vessel lumen, extracellular fibrosis, and eventual adipose tissue differentiation.1,3
Vascularised lymph node transfer (VLNT) involves the free tissue transfer of lymph nodes (LN) from one location to the affected extremity with micro-anastomosis of the vasculature to the recipient bed. There is no consensus on the optimal donor site of the harvested LN, the timing of transfer or whether VLNT is optimised by simultaneous breast reconstruction.4,5 Similarly, previous studies have only reported limited follow-up periods ranging from three to 64 months.5
Here, we present the seven-year follow-up data for the first use of a delayed breast reconstruction using a free transverse rectus abdominis muscle (TRAM) flap with simultaneous VLNT in Australia, performed following initial conservative therapy.
Case
A 59-year-old right-hand-dominant female teacher was referred to the Australian Lymphoedema Education, Research and Treatment (ALERT) program at the Macquarie University Hospital (MUH, NSW, Australia) with a history of mammographically-detected invasive lobular carcinoma (ER +ve, PR +ve, HER2 -ve) of the right breast. Mastectomy and SNB were performed in March 2012, and histopathology of two sentinel nodes revealed residual disease. The patient subsequently underwent ALND with 30 LN removed. Histopathological analysis demonstrated no residual disease, and postoperative radiotherapy and chemotherapy with doxorubicin, cyclophosphamide and paclitaxel were given. Following the second dose of paclitaxel in August 2013, the patient developed right periorbital cellulitis requiring hospitalisation. Simultaneously, the patient developed right arm lymphoedema, with an increase in the L-Dex score from a baseline of +2.9 to +10 (n = -10 to +6.5). The patient was managed conservatively with a compression sleeve and massage, which resolved the swelling to a L-Dex score of 3.9. Followinga return to work, arm and hand swelling returned with a L-Dex score of 39.0, causing significant functional impairment despite conservative therapies.
The patient was selected for a delayed right breast reconstruction using a right TRAM flap with a contiguous VLNT from the left inguinal LN as it allowed for a single incision from the donor site. Due to the patient’s history of periorbital cellulitis, the supraclavicular LN basin was deemed inferior.
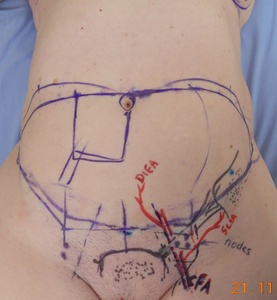
Preoperative indocyanine green (ICG) lymphoscintigraphy demonstrated dermal backflow of dyes in the right forearm with no dye accumulation in the right axillary LN basin. Preoperatively, the patient underwent an ultrasound of the left inguinal region, which identified harvestable LN (Figure 1). Unfortunately, no LN was identified superior to the inguinal ligament, which is considered favourable due to the lower risk of lower limb lymphoedema in the event of lower limb surgery or cellulitis.4
The patient underwent a simultaneous double-pedicled free-flap breast reconstruction in November 2013. The recipient site was prepared with resection of previous scar tissues in the axilla and the right fourth costal cartilage to allow for the preparation of the right internal mammary artery and vein. The right TRAM flap was raised with the right deep inferior epigastric artery (DIEA) and veins. The left inguinal VLNT flap was raised as a contiguous extension of the TRAM flap with the left superficial circumflex iliac artery (SCIA) and veins. The combined flap weighed 1087 g. Microvascular anastomosis was performed between the right DIEA and veins to the right internal mammary vessels, and the left SCIA and veins to the right thoracodorsal vessels proximal to the serratus branch. The total ischaemia time was 53 minutes. The rectus defect was repaired with synthetic mesh before abdominoplasty closure.
The patient’s recovery was uneventful, and she was discharged after one week. She attended regular ambulatory follow-up with measurements of L-Dex and volumetric measurements of both arms (figures 2 and 3).
Postoperatively, the patient developed a seroma of the left groin donor site, which required repeated weekly aspirations for four weeks, and a single episode of bacillus cellulitis, treated with a short oral course of clindamycin.
Results
Ultrasound of the axilla with Doppler was routinely used to assess blood flow dynamics in the flap, in addition to ICG lymphography, to demonstrate the development of lymphatic channels. An ultrasound exaxmination one year postoperatively demonstrated a single morphologically normal LN deep in the right axilla. There was unilateral pitting oedema in the left upper thigh, but there was no discernible size difference in the lower limbs.
At the three-year postoperative follow-up, swelling was well controlled with regular daytime compression and nightly alternating regimen of pneumatic pump compression or compression garments. Indocyanine green lymphography identified dye transit between the mid upper arm and axilla, both anteriorly and medially, suggesting the development of deep lymphatic connections to the transferred LN. There was no clinically detectable lower limb lympheodema and upper limb oedema was controlled.
Unfortunately, in 2018, the patient developed an early melanoma in the right arm that required surgical resection, resulting in an acute exacerbation of lymphoedema with an L-Dex score of 70. Intensive lymphoedema physiotherapy post-resection allowed the patient’s swelling to return to baseline.
Indocyanine green lymphography performed seven years postoperatively demonstrated further lymphatic drainage to the axilla. Lymphatic vessels were identified in the anterior forearm with connections to the deep lymphatics above the elbow. In the posterior aspect of the arm, dermal ICG dye backflow was evident, but moved relatively quickly. The reconstructed breast remained soft and adequately symmetrical with natural ptosis. Compared to the initial presentation, lymphedema of the upper limb had greatly reduced, was soft, and the patient was satisfied with the outcomes.
Discussion
Advances in microsurgical techniques and high rates of lymphoedema following mastectomy and ALND have generated great interest in lymphoedema surgery, with a particular interest in VLNT. Inconsistent results, the lack of significant evidence-based trials and data on the long-term feasibility of this technique have limited uptake by the general surgical community.4,5 Of the few studies that report on the use of a contiguous TRAM/VLNT flap, only three studies had quantitative, volumetric measurements of lymphoedema.5–8 The longest follow-up period reported in the literature is 64 months9 with the longest follow-up ICG lymphography study performed 12 months postopertatively.6
This case highlights the merit of long-term follow-up and studies of patients who have received VLNT or other lymphoedema therapies. VLNT allows for thecontinued efficatious use of conservative therapies long term.
Conclusion
This case demonstrates the application and long-term feasibility of an effective treatment, which allows for a functional and aesthetic flap to treat those with disrupted lymphatic drainage. While this personalised, surgical approach within a comprehensive multidisciplinary service was effective in this setting, further research is necessary to prove the long-term effectiveness of this lymphoedema treatment.
Patient consent
The patient has given informed consent to the publication of images and/or data.
Conflict of interest
The authors have no conflicts of interest to disclose.
Funding declaration
The authors received no financial support for the research, authorship, and/or publication of this article.
Revised: 28 January 2023; 6 July 2023
_patient_photographs_showing_the_preoperative_defect_of_the_right_breast_(b)_and_the_recon.jpeg)
__and_the_percentage_difference_in_arm_v.tiff)

_patient_photographs_showing_the_preoperative_defect_of_the_right_breast_(b)_and_the_recon.jpeg)
__and_the_percentage_difference_in_arm_v.tiff)