Introduction
Postoperative complications are detrimental to patient outcome and an essential target for improving surgical quality. Growing demand, limited resources and increasing healthcare costs with variation across units are additional arguments for stringent audit of complications. Initially, universal comparison of these adverse events was hampered by the lack of an objective and agreed definition of a postoperative complication. Clavien and colleagues,1 Veen and colleagues,2 and Sokol and Wilson3 have described a standardised definition for surgical complications, put simply as ‘any deviation from the normal postoperative course’. This, however, fails to capture why these events are significant. A refined definition is ‘any deviation from the typical postoperative course, with a corresponding effect on outcome’. Similarly, ‘classification’ is a better descriptor than ‘grading’ as different levels do not necessarily equate with a graduated increase in severity.4
Clavien and colleagues first coined the term ‘T92 system’, given its origin in Toronto in 1992.1 The system was revised by Dindo and later renamed the Clavien-Dindo Classification (CDC). The CDC was first evaluated in 6336 patients undergoing elective general surgery at a single institution5 and then again over the ensuing five years across various centres.6 The basis of the CDC is that a complication is classified per the intervention required to treat it. Briefly, a simple deviation from the typical postoperative course treated non-pharmacologically, such as symptomatic anaemia requiring blood transfusion, would be a grade I. In contrast, a complication resulting in mortality is a grade IV, the most severe complication. Return to operating theatre (RTT) is described as grade III. The Accordion Severity Grading System (ASGS) styled by Strasberg and colleagues7 is similar to CDC, the main difference being the former ignores intensive care unit (ICU) admission and focuses on the presence of any level of organ failure as a single grade IV.8
One criticism of the CDC is that it focuses on the single most severe complication and ignores lesser events, hence it is unrepresentative of true overall morbidity.8 Slankamenac and colleagues developed the Comprehensive Complication Index (CCI), an extension of CDC that quantifies the cumulative burden of all complications as an aggregate score of 100. As such, CCI demonstrates a superior predictor in terms of hospital stay, survival and healthcare cost.9–16
An important consideration is RTT in plastic and reconstructive surgery (PRS) can present a moderate range in outcome, which is of limited description in these current systems. As examples, haematoma evacuation, prosthesis revision, and flap failure salvage each bear significant heterogeneity in morbidity. Furthermore, many PRS procedures are relatively minor, and complications resulting in ICU admission or mortality are less common in our cohort, particularly in the elective setting. Similarly, patients may frequently RTT, which does not necessarily presage a significant downstream effect on outcome, such as scar correction, wound dehiscence or even moderate haematoma evacuation.
It is hypothesised that an emphasis on RTT would be a considerable avenue for developing a classification of postoperative complications unique for PRS. This review aims to ascertain the use of current systems in PRS, identify any systems already designed for PRS and ultimately develop a classification of postoperative complication unique to PRS.
Methods
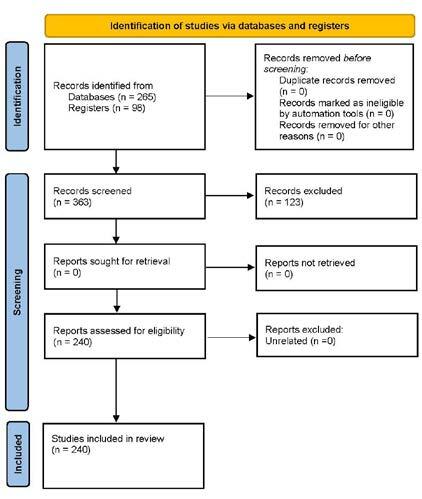
An initial literature review using PubMed, targeting PRS research only was found to be limited, hence the review was expanded to include all types of surgery. The search was performed using a combination of medical subject headings (MeSH) terms: ‘classification’, ‘grading’, ‘adverse events’, and ‘postoperative complications’. There was no date range applied to the search, hence our review captured all articles in the PubMed database published prior to 2023. These were then limited to level-one evidence, that is, systematic reviews, meta-analyses, and randomised control trials, with the exclusion of book chapters, case reports, commentaries, and anecdotal evidence.
From this search 265 papers were derived. Further additions through bibliographic linkage accumulated 363 articles for title and abstract review. Of these, 24 were related to current systems in PRS, and 107 articles to the use of these systems in other specialties. The remaining articles were kept for discussion on methods of external validation (35), important outcome measures (12) and preoperative factors that confound universal comparison (29). Figure 1 demonstrates this stratification.
Results
Twelve papers used CDC to describe postoperative complications in PRS, primarily in free flap surgery. The AGCS was used in four papers and had a much larger scope of patients from breast, aesthetic and carpal tunnel procedures.17–20 In the broader surgical literature, CDC was used in 88 papers, and ASGS in 19 papers. Hence, evaluating current systems in PRS forms a minority (16/107, 15.0%).
External validation through correlation with postoperative length of stay (PLOS) and interobserver reliability was proven in two papers assessing CDC in a head and neck series.21,22 One study used CDC to benchmark complications with and without radiotherapy in similar cases.23 Another study used CDC to benchmark the safety of free jejunum transfer in preventing anastomotic leak.24 The remaining studies also supported CDC; however, analysis supported its interobserver reliability rather than its correlation with outcome.25–30 One study doubted the use of the CDC in craniofacial surgery.31
Eight papers used a unique system or no system at all. Aljerian and colleagues, in their systematic review of brachioplasty patients, collated a scope of complications that may warrant RTT.32 These were scarring, recurrence, dehiscence, seroma, infection, nerve-related complications, delayed healing, lymphoedema and haematoma. Wound dehiscence is a broad complication in PRS as management can range from dressing support to vacuum-assisted closure (VAC) or formal operative intervention.33 Dehiscence is a particularly morbid complication in cranioplasty after decompressive craniectomy.34 Steele and colleagues looked at the incidence of wound breakdown as a complication after simple, intermediate and complex closure of defects after hidradenitis suppurativa.35 Similarly, Zheng and colleagues classified sternal wound complications according to the reconstructive method used for closure, that is, wounds of type I closed with local flap transplantation versus wounds of type IV repaired with a pedicled omental flap.36 Qassemyar and colleagues proposed a unique classification similar to CDC that described complications in accordance with the method to treat them, yet this was validated in only a small case series of 16 patients undergoing elective body lifts.37
It is apparent that RTT is a source of wide heterogeneity and morbidity in PRS. Therefore, demarcating reasons for RTT and establishing their respective correlation with outcomes would be the key to designing a specialty-specific classification of postoperative complications. In this process, a variety of complications unique and important to PRS were identified:
-
transient discomfort, pain, nausea or vomiting
-
bruising or minor haematoma
-
symptomatic or severe postoperative anaemia requiring blood transfusion
-
minor wound dehiscence, managed conservatively with dressing support
-
suture-related issues (stitch abscess, retained suture)
-
prolonged swelling or oedema
-
seroma
-
minor infection, managed with oral antibiotics
-
moderate haematoma attaining evacuation without general anaesthesia
-
aesthetic dissatisfaction (asymmetry, contour, over or under correction)
-
unfavourable scarring (hypertrophic, keloid, contracture)
-
major wound dehiscence, requiring surgical intervention
-
major haematoma, requiring formal evacuation under general anaesthesia
-
moderate infection, requiring intravenous antibiotics or debridement
-
partial skin necrosis or flap compromise
-
complete skin necrosis or flap compromise
-
implant-related complications (malposition, rupture, contracture)
-
functional impairment (restricted range of movement, motor or sensory damage)
-
major infection meeting sepsis criteria warranting ICU admission
-
deep vein thrombosis (DVT) or pulmonary embolism (PE)
-
anaesthetic complications warranting ICU (allergy, cardiorespiratory arrest).
There is strength in the current systems in that subjective bias is limited. As complications are classified by the treatment required, the current systems have demonstrated interobserver agreement over time, proving them to be simple and reproducible. Therefore, rather than reinventing the current systems, it may be better to modify CDC incorporating the above syllabus of complications. In this fashion, Jan and colleagues proposed a modification of CDC for PRS to include grade IIIc, representing partial or total free flap loss.38 Return to theatre for free flap perfusion complications may be described in itself concerning partial versus complete flap loss or due to arterial versus venous insufficiency.39 In head and neck reconstruction RTT for flap loss is a morbid complication.40
The following is a further modification of CDC incorporating the above syllabus of complications. The graded severity of each complication in this system is currently anecdotal, and will need to be validated in a follow up study.
Grade I: Complications not requiring medical management or RTT
Ia: Transient bruising, discomfort, pain, nausea or vomiting
Ib: Minor wound dehiscence managed conservatively
Ic: Seroma managed with bedside aspiration
Grade II: Complications treated medically or requiring RTT for a minor procedure
IIa: Minor infection treated with oral antibiotics
IIb: Hematoma evacuation under local anaesthesia
IIc: Revision for aesthetic dissatisfaction not involving implant exchange or major reconstruction
IId: Scar revision or minor contour correction
Grade III: Complications requiring RTT for a major procedure
IIIa: Hematoma evacuation under general anaesthesia
IIIb: Moderate infection requiring intravenous antibiotics or debridement
IIIc: Skin necrosis or flap compromise requiring debridement or reconstruction
IIId: Implant-related complications necessitating implant exchange or removal
IIIe: Surgical intervention for functional impairment or nerve damage
Grade IV: Life-threatening complications requiring ICU or major surgery
IVa: Major infection or sepsis requiring ICU and aggressive surgery
IVb: DVT or PE requiring anticoagulation therapy or intervention
IVc: Major anaesthetic complications (allergy, cardiorespiratory arrest) requiring ICU
Grade V: Death due to surgery or its complications
Discussion
Limitations of current systems
Although CDC, ASGS and CCI are widely accepted across various specialties including PRS, there are currently no well-established grading systems tailored to our specialty. The primary limitation is that these current systems lack procedure-specific criteria, and are therefore not tailored to specific surgical disciplines. Although this universal nature has merit, the general nature of these systems restricts their applicability. The ideal system is simple, reliable and reproducible.
Postoperative period
One aspect not immediately clear in the literature, is precisely when the postoperative period begins. Theoretically, this can begin anywhere from commencement of closure, instrument count, dressing application, cessation of anaesthesia, formal extubation, post-anaesthetic recovery, or arrival on the postoperative ward. Formal extubation does not sufficiently indicate the postoperative period. Some patients may have a prolonged wake from anaesthesia, failure to wean off a ventilator, or be kept sedated and intubated for airway and central nervous system (CNS) support. Formal discharge from the operating theatre is similarly inaccurate; an example would be a patient in recovery returning to theatre for evacuation of haematoma, which would be represented as a postoperative complication in a surgical audit.
Cessation of anaesthesia and when the patient is undraped is the best indicator. Intuitively, the index procedure would continue if there were an on-table complication while the patient is still under general anaesthesia and, furthermore, reinducing a patient to address a complication would be a significant undertaking. This delineation is significant as it separates postoperative complications from intraoperative complications, which is a separate area of study. Postoperative complications are also less subject to interpretation bias, given that they are defined by the treatment, whereas intraoperative events are subject to operator detection. One could argue that some postoperative complications are due to undetected intraoperative issues. Current systems do not include intraoperative issues, and there are separate grading systems for these events, such as ClassINTRA.41
Duration of observation
In a similar fashion, an adequate observation period postoperatively is required to capture all, if not most postoperative complications. Schwarz and colleagues determined 90 days as a modest benchmark to allow adequate detection of postoperative complications.42 In their study of pancreatectomy patients, complications increased by 10 per cent between 30 and 90 days, and 35 per cent of readmissions occurred during the period beyond 30 days. Additionally, 30-day mortality only captured 40 per cent of postoperative deaths, whereas 90 days captured 85 per cent of surgically-related deaths. It should also be mentioned that complications beyond this period may be related to other factors. Excusing complications beyond this period also mitigates attrition bias.
Construct validity—outcome measures
The purpose of having a graded classification of postoperative complications is that it ideally correlates with the severity of outcome. Hence, we must first understand what outcome measures are most important. Every specialty will have a particular set of unique outcome measures. For example, recurrent stroke after carotid endarterectomy,43 functional deficit after elective aneurysm clipping,44 and survival after oncological resection.45 Lerut and colleagues interestingly demonstrated a correlation between the severity of complication and oncological recurrence.46 Out of 17 articles demonstrating adequate construct validity, PLOS was the chosen outcome measure in 14 studies (82.4%). Surgical complications during the index admission are the main reasons for prolonged PLOS.47 Similarly, unplanned readmission is disappointing for patients; an extra two or three days in the hospital is less of a burden than being discharged and returning to the hospital for the same time.48 Short PLOS and infrequent readmissions are, therefore, the desired outcomes, can be measured objectively and should be the primary indicators for grading postoperative complications.
PLOS and unplanned readmission can be interrelated. Takchi and colleagues noted that shortened PLOS was associated with increased readmission after pancreaticoduodenal resections.48 Thus, if the effect on readmission is considered, longer PLOS could be beneficial, and shorter PLOS confounding. Composite length of stay (CLOS), a summation of PLOS and readmission LOS, may be used as an accurate single quality measure addressing this.47 ‘Hospital free days’ over a specific observation period is an alternate way of describing this.49 Again, the goal is to reduce CLOS with a concurrent reduction in readmission, as demonstrated by Holoyda and colleagues in their study of reconstructive breast patients.50
Of course, PLOS may be unreliable in comparing multicentre outcomes due to individual medical policies regarding discharge. Socioeconomic status, discharge against medical advice and absconding are further confounders. In the same way, readmission can be criticised. Rodriguez and colleagues found racial disparity may play a role in increased readmission after less severe postoperative complications from pancreatic surgery.51
Discharge destination can also be a useful outcome measure. Longer recovery and the need for inpatient rehabilitation pose significant patient, carer and hospital burdens, which can also influence timely discharge. Sanford and colleagues demonstrated discharge home with health care to be an independent predictor of frequent readmission, particularly non-severe readmission.52 This may be due to the inability to manage minor complications as an outpatient.51 Intensive care unit stay during admission is also a considered and objective outcome measure.
Other remaining outcome measures are challenging to ascertain. Cost analysis and patient-centred outcomes are examples; however, such in-depth analysis is subject to multiple confounders, is non-standardised, and not necessarily all-encompassing. The economic status of the patients and the type of reimbursement in different hospitals may significantly affect the medical cost. Patient-centred outcomes are similarly criticised.53 One study highlighted no correlation between CDC grade and patient-reported severity for an adverse postoperative outcome.54 Although, one study did establish a correlation between CDC grade and quality of life at six weeks.55
Lastly, from the point of view of the clinician, ease of use of a developed system can be tested by ascertaining interobserver reliability.56 Again, one of the strengths of the CDC is that its classification method makes it inherently objective. One study assessed interobserver reliability between low-income and high-income countries.57 Even the ability to cross language has been trialled.58 Wingerden demonstrated reliability between reconstructive surgeons and caregivers,59 which has implications for detecting complications after leaving hospital. On the contrary, despite proving moderate validation of the CDC, one study proved low interobserver reliability for minor complications.60 In the future, having a standardised definition would potentially allow the detection of complications by screening an electronic medical record61 or through natural language processing.62
Limitation of proposed model—preoperative issues
Multiple preoperative factors may presage or even predict postoperative complications in any cohort. The American Society of Anesthesiologists (ASA) physical status classification system has proven clinical efficiency in predicting perioperative risk,63 for both inpatient and outpatient procedures.64 Specific to PRS, a higher ASA class is associated with increased surgical site infection, bleeding, hospital stay and failure to wean ventilation following facial fracture repair.65 Premorbid illness also complicates the interpretation of postoperative adverse events.66 One study proved the presence of three or more comorbidities to be an independent predictor of postoperative complications.67 The Charlson Comorbidity Index (ChCI) is a preoperative index of comorbidities to predict postoperative risk.68 When expressed as the ChCI, comorbidities may be predictive of vascular compromise and impending flap loss.30 As measured by timed stair climbing, sarcopenia has been proven to be an independent predictor of postoperative outcome and the best marker of frailty.69,70 A five-item frailty index has been developed for patients undergoing free flap breast reconstruction with a moderate association with complications.71
Additionally, surgical complexity and operating time in PRS is directly associated with wound complications, PLOS and unplanned readmission.72–74 Koras and colleagues established operating time to be positively correlated with complications.73 In addition to improved outcomes, having a second surgeon in breast reconstruction has a corresponding improvement in hospital cost.75 Elective versus emergency surgery is also a crucial preoperative factor in rationalising complications. Indeed, when procedures are performed on a life-saving or compassionate basis, death in this setting constitutes a grade IV complication.
These preoperative aspects are to gauge complications from different cases across institutions. A major difficulty of any classification system is standardising postoperative complications against preoperative issues. Having some form of risk adjustment to standardise the comparison of complications between different institutions makes the model even more complex. The current revolution in machine learning may work out a big data method to help with this.76
Limitations intrinsic to PRS
Finally, in the CDC, some complications are not represented such as those that do not require immediate treatment yet herald long-term morbidity. For example, facial nerve palsy is graded mildly by CDC as it does not frequently result in RTT, ICU admission or mortality.77 However, the same complication in a different settings may have a proportionate outcome. For example, facial nerve palsy after parotidectomy for a benign lesion is more significant than if the same complication occurred in a patient undergoing a malignant head and neck resection, where such a complication is considered to be sequelae of the procedure.
PRS presents a unique cohort in that scar quality, wound healing and patient satisfaction garner a more significant impact on our population. Aesthetic satisfaction after breast reconstruction deteriorated with CDC grade in one study.78 However, as with cost analysis, such outcomes are difficult to measure owing to the multidimensional nature of postoperative recovery.79 Notably, particularly in aesthetic surgery, preoperative body image and patient perception may correlate with complications after breast reconstruction.80 It should be noted that incomplete margins after skin excision is not included in our modified CDC. Usually, these patients await recovery, are seen as an outpatient, discussed with consensus and can be managed conservatively, medically or surgically.
Conclusion
There is moderate application of current classification systems for postoperative complications in PRS. However, current systems are all encompassing and limited in various intrinsic factors unique to PRS, primarily return to theatre garnering a heterogeneous range of outcomes. A modified version of the Clavien-Dindo Classification is presented, emphasising reasons for return to theatre to make the Clavien-Dindo Classification unique to PRS.
Conflict of interest
The authors have no conflicts of interest to disclose.
Funding declaration
The authors received no financial support for the research, authorship, and/or publication of this article.
Revised: April 26, 2023 AEST