Introduction
While the deep inferior epigastric artery perforator (DIEP) flap remains the gold standard in breast reconstruction, there are a number of relative contraindications, such as previous abdominoplasty or transverse and oblique abdominal scars.1 The lumbar artery perforator (LAP) flap was first reported in breast reconstruction by De Weerd and colleagues in 2003.2 The LAP flap has been gaining recognition in breast reconstruction with some surgeons suggesting it has become the second choice free flap for breast reconstruction where an abdominal-based reconstruction has failed or is otherwise contraindicated.3–5 Some benefits of a LAP flap include a decreased anterior scar burden, an accentuation of the natural concave lumbar curvature and lifting of the buttock. In the two largest series published, the LAP flap has a flap loss rate of 6.6–9 per cent, which is higher than for DIEP flaps at around 2 per cent.3,5 While this may represent a learning curve, concerns for the need for an arteriovenous interposition graft, the size of flaps available on the lumbar system, and the need for an intraoperative position change have led to hesitation regarding its use, particularly in patients undergoing large volume breast reconstruction. We present a literature review addressing these concerns and a case of a 1.1 kg LAP flap in a patient undergoing unilateral salvage breast reconstruction, demonstrating the LAP flap’s utility in these settings.
Case
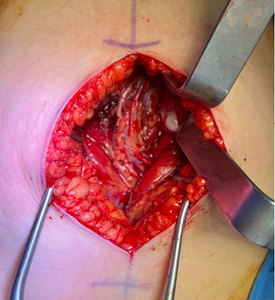
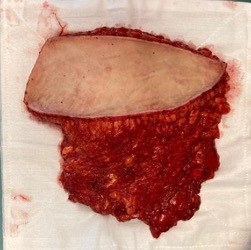
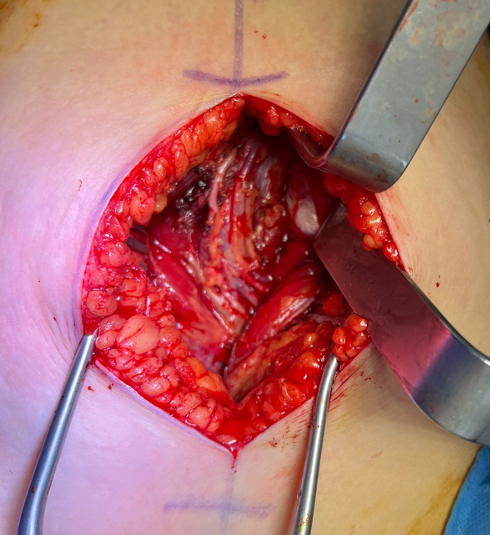
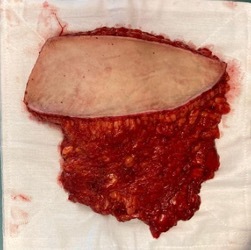
A 44-year-old woman was referred for a salvage right breast LAP flap reconstruction following a failed right transverse rectus abdominis myocutaneous (TRAM) flap two years earlier (Figure 1). A preoperative computed tomography (CT) angiogram showed a large ipsilateral fourth LAP with two septocutaneous branches. We designed our flap markings to capture this perforator, which was confirmed with handheld Doppler. After general anaesthesia, the patient’s right internal mammary vessels were prepared. Once the recipient vessels were found to be suitable, an anterolateral thigh incision was used to harvest the left descending branch of the lateral circumflex femoral artery (DBLCFA) as an interposition arteriovenous graft (Figure 2). The patient was then positioned prone and the LAP flap was harvested using a standard flap technique, with bevelling superiorly and inferiorly to include additional gluteal fat. This enabled us to harvest a flap with a weight of 1.1 kg (Figure 3). As the harvest team closed the donor site, a second team performed back table microsurgery connecting the harvested grafts to the flap. The patient was then positioned supine for the final microsurgical anastomoses to the internal mammary vessels and the flap was inset. Pedicle length was 5.5 cm with an additional 3 cm interposition graft, and ischaemic time was 64 minutes. Operative time was 369 minutes. The patient recovered well without complication. At six weeks postoperatively she had no signs of wound complications or fat necrosis (Figures 4 and 5).
Discussion
Most studies of the LAP flap have originated from Ghent University Hospital, including the three largest series.4–6 Prior to the present case, the largest successful reported LAP flap was a 750 g flap used in sacral reconstruction,7 and the largest LAP flap used in breast reconstruction was 730 g.8 The authors of the Ghent series reported LAP flap sizes between 77 g and 1216 g, however information was not given on the outcome of the large LAP flap and did not specify if this represented a stacked flap.4–6 The average size of a LAP flap used in breast reconstruction has been around 495 g.8 Raising our flap on two perforators, the body habitus of our patient and significantly bevelling gluteal fat during flap harvest may have enabled the larger flap weight of 1.1 kg without complications, such as fat necrosis. Anatomical studies have found that two perforators are most likely in the second and fourth lumbar arteries, however this is not present in all cases.9,10 While not used in our case, a preoperative CT scan may be useful in identifying dual perforator anatomy in patients under consideration of large volume reconstruction. In breast reconstruction, the presentation of fat necrosis can vary widely, with studies showing presentations as early as day five up to seven-and-a-half months postoperatively.11
Donor site morbidity seroma
The incidence of donor site seromas varies widely, and has been reported as high as 78 per cent.8 Other series have found rates between 13 and 43 per cent, which may reflect the differences in surgical technique.3,5 Some surgeons advocated the use of quilting sutures and a ‘vest-over-pants closure’ while others recommended a more anterior design of the flap to help preserve the lymphatic drainage over the thick fascia of the paraspinal muscle.4,8 Management varied but usually involved serial aspiration and use of compression garments. Increased donor site morbidity in the form of increased flank pain can be an issue in select patients, however results have been inconsistent in published series to date.4–6,8,12 While anterior scar burden is reduced, the donor site scar is too high to be easily covered with standard underwear or swimwear and this may be an important consideration for some patients. In our case, the lumbar donor site provided minimal pain for the patient, the drain was retained for three weeks and there were no seroma complications; however, this may reflect the early follow-up of six weeks.
Position change
A downside to the use of the LAP flap for breast reconstruction is the necessary intraoperative position change from supine to prone then back to supine. While this is an inconvenience, it does not appear to significantly impact operative or ischaemic time, with several studies finding surgical times comparable with DIEP flaps in both bilateral and unilateral reconstructions.3,5,13 Our case had an operative time of 369 minutes and an ischaemic time of 61 minutes which is similar to the average duration of a delayed unilateral DIEP breast reconstruction.13 This is important as prolonged ischaemic time greater than 99 minutes has been found to correlate with fat necrosis.14
Pedicle
One of the shortcomings of the LAP flap is its short pedicle length, usually necessitating an arteriovenous interposition graft, most often taken from the deep inferior epigastric artery (DIEA) and deep inferior epigastric vein (DIEV) system.6 The thoracodorsal vessels have also been described in patients in whom the DIEA and DIEV vessels are unavailable, either due to previous abdominal surgery or previous DIEP reconstruction.6 Given our familiarity with the anterolateral thigh flap, we used a graft harvested from the DBLCFA in our patient. Most cases report using the DIEA and DIEV as an interposition arteriovenous graft, however this was not an option for our patient who had these vessels harvested for her prior bilateral TRAM flap. The lateral circumflex femoral artery and vein provided a good vessel size match for the LAP flap, was a straightforward harvest which is familiar to most plastic surgeons, and created an acceptable donor site. The use of the DBLCFA instead of the thoracodorsal vessels has the added benefit of preserving the latter as a pedicle for the latissimus dorsi, which retains it as a salvage option. To our knowledge this is the first reported use of the DBLCFA in this manner.
Conclusion
The LAP flap is a valuable asset in the breast reconstruction toolbox. While abdominal-based reconstructions are the gold standard, in patients with contraindications or salvage procedures, the LAP flap can provide a large amount of tissue for breast reconstruction. Technical considerations such as the use of outward bevelling to include gluteal fat and incorporating a second perforator when available may lead to lower rates of complications such as fat necrosis.
Patient consent
Patients/guardians have given informed consent to the publication of images and/or data.
Conflict of interest
The authors have no conflicts of interest to disclose.
Funding declaration
The authors received no financial support for the research, authorship, and/or publication of this article.
Revised: May 26, 2023 and June 14, 2023 AEST