Introduction
Successful facial reconstruction requires accurate restoration of the concealed three-dimensional facial skeleton. The key rationale for intraoperative computed tomography (iCT) is that it facilitates the most comprehensive assessment of fracture reduction. Real-time visual feedback is now considered an essential component in hand, spine and general orthopaedic surgery. Frequently proposed as the new gold standard of care, iCT has been widely adopted in maxillofacial surgery, especially internationally. In contrast, our Australian experience is that access to iCT and therefore uptake is relatively lacking. The craniofacial skeleton is a complex structure owing to its various convexities and concavities, sinonasal elements, biomechanical buttresses, visceral and occlusal components and neurovascular structures. Classic approaches to open reduction internal fixation aim to reduce incisions to prevent complications such as ectropion, salivary leak or nerve damage. However, intraoperative assessment of fractures in minimally-invasive techniques are hindered by the limited extent of exposure, especially in the setting of complex fracture patterns or those that involve dynamic or functional endpoints. With iCT, surgeons may visualise, adjust and revise fixation without wide exposure while the patient is on the operating table. This obviates an additional operation that may be required due to an unsatisfactory fixation. Other benefits are that iCT is cost-effective and reduces radiation exposure. Challenges in integrating iCT include competing for availability with other specialties, training staff and lack of awareness about the benefits this technology offers. This narrative review discusses the role of iCT in the modern Australian operating theatre.
Discussion
The key rationale for iCT is that it facilitates the best possible intraoperative assessment of fracture reduction and fixation. Pre- and postoperative computed tomography (CT) with fine-slice and three-dimensional image reconstitution is established as the gold standard for assessing both the presence and degree of bony displacement, as well as the accuracy of operative reduction.1 Intraoperative assessment using iCT , however, is not routine in many centres in Australia, despite its established use in other surgical specialties,2 descriptions of its use in craniofacial trauma since the 1990s3 and calls for it as a standard-of-care.1,4
The craniofacial skeleton is a complex structure owing to its various convexities and concavities, sinonasal elements, biomechanical buttresses, visceral and occlusal components, and neurovascular structures. Traditional approaches to fixation of the craniofacial skeleton are via limited exposures, such as the temporal (Gillies) approach for zygomatic arch reduction and the retromandibular approach to a subcondylar mandible fracture. Therefore, it is unsurprising that intraoperative assessment of fractures in these minimally-invasive approaches is hindered by the limited extent of exposure, especially in the setting of complex fracture patterns or those that involve dynamic or functional endpoints. Intraoperative CT emerged in the late 1990s as a rapid method to accurately evaluate hardware position, fracture reduction and dynamic skeletal positions. Indeed, real-time visual feedback is considered an essential component in hand, spine and general orthopaedic surgery.2 Resultantly, surgeons may visualise, adjust and revise fixation while the patient is on the operating table, obviating an additional operation that may be required as a result of an unsatisfactory reduction and or fixation. Marrying minimal-access approaches with iCT conveys the benefits of wide exposure without consequences such as scarring, aesthetic deformity, risk of facial nerve injury and ectropion.5 For example, in mandibular ramus fractures, less-invasive access is preferred to prevent scarring and salivary fistulae, however it can cause excess retraction leading to temporary or permanent nerve injury. Intraoperative CT can augment minimally-invasive options that preclude panoramic fracture views such as temporal, retromandibular and endoscopic-assisted techniques to mandibular rami. With iCT, restoration of ramal height and dynamic effects of mandibular movement on fixation can be assessed and revised during the index operation.
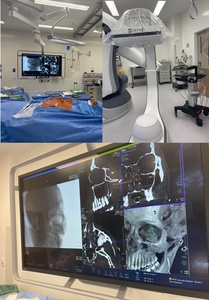
Orbital floor reconstructions provide yet another avenue for iCT usage. The undulating nature of the orbital floor and classic, anterior approach permit only a narrow surgical field which can make depth perception challenging and risky. Although individualised anatomy and complex fracture patterns are more accurately addressed by the expanding presence of computer-assisted technology and in-house three-dimensional printing, precise intraoperation navigation remains the highest standard of care.1 Figure 1 demonstrates the utility of iCT for an orbital floor reconstruction. Intraoperative CT is excellent at ensuring precise implant location and relationship to soft tissue and bony structures, such as the posterior ledge in an orbital floor fracture. Visual impairment is a devastating complication of periocular surgery that arises more frequently in trauma than elective cases (6.45% vs 0.84%).6 Prevention of malpositioned hardware by insertion under iCT may mitigate this risk.
The overall revision rates documented in the literature with reference to the outcome of surgical reduction of facial fractures in combination with the application of iCT range from 24 per cent (zygomaticomaxillary fractures) to 31 per cent (orbital fractures).7 These high intraoperative revision rates while using iCT suggest operative reductions that clinically appear acceptable frequently have scope for improvement, suggesting that the threshold for revision is lower with iCT owing to the opportunity to improve fixation before the conclusion of the procedure.8 This is further supported by studies using iCT reporting relatively high intraoperative revision rates accompanied by absent or reduced return to theatre revisions.8 The far-reaching implications of reduced return to theatre revision rates include avoidance of a second operative procedure (and morbidity related to anaesthesia and surgery), reduced costs associated with readmission, uninterrupted wound healing and faster patient recovery. It is therefore unsurprising that the globally-recognised AO Foundation recommends iCT for all mid-face and orbital reconstructions.1
Australian centres performing facial fracture fixation will already have the existing infrastructure to support iCT (scanner, compatible operating suite, software, radiographers and draping equipment). This is a unique advantage of implementing iCT as a novel technique for maxillofacial trauma surgery services.
Intraoperative CT decreases radiation exposure to patients as the dose patients are exposed to with iCT is less than standard postoperative CT.9 Even with multiple iCTs performed, a cumulative dose remains lower than standard because the radiation dose of iCT (single cone-beam) is 13–82 microsieverts whereas traditional CT (fan beam) is 474–1160 microsieverts.9 Additionally, iCT is anatomically focused to the region of interest thereby reducing radiation to the entire facial skeleton.
Finally, in Australia, trauma centres are typically the same centres in which surgical training occurs. Real-time review of fracture reduction allows trainees to combat the learning curve of maxillofacial trauma more efficiently.10 While not the primary aim of the intervention, real-time feedback of imaging and anatomy is an invaluable opportunity for training surgeons.10
In our unit the learning curve for the surgical team performing the set-up sequence initially increased operative time. While operating time may be extended due to iCT set-up, actual scanning time is under one minute.8 Alasraj and colleagues reported iCT required an additional 18.9 +/− 4.6 minutes.11 We also faced issues with resource allocation of the CT machine or hybrid operating suite. As iCT is well established in other surgical specialties, it is possible iCT may be requested by multiple surgical teams simultaneously so prior planning is critical. This is feasible in facial trauma, and we have found this essential to prevent cases from being deferred or delayed. Financial concerns are important when integrating changes in technology into practice. Intraoperative CT is cost-effective though costs will be significantly reduced if hospitals already own the technology,4 as all Australian trauma hospitals should.
Our unit selectively performed iCT during 2021 and 2022 in 10 cases: six orbital floor, one medial orbital wall, one panfacial, one mandible (subcondyle/body) and one frontal sinus/orbital roof reconstruction. The ARTIS pheno C-arm imaging system (Siemens AG, Erlangen, Germany) in a hybrid suite was used (see Figure 1). Theatre radiographers did not require additional training or changes to routine iCT protocols used by our vascular, orthopaedic and neurosurgical colleagues. A single case of orbital floor reconstruction required revision of hardware placement due to impingement of orbital soft tissues. In our institution there was no additional cost of using the iCT scanner in orbital floor reconstruction: in fact, a single episode of using iCT is cheaper than standard pre and postoperative CT (AU$65 versus AU$230) (see Table 1). A further cost disparity occurs when comparing iCT cost (AU$4687) with that of performing revision procedures (AU$8419 –AU$9574). It is beyond the scope of this article to further elucidate cost-effectiveness though it is clear preventing only a few revisions would justify changing to iCT use as standard of care.4,7
Conclusion
The now widespread uptake of iCT in numerous international maxillofacial units has allowed patients to experience lower diagnostic radiation exposure, more accurate reduction (and fixation placement), less requirement for revision surgeries, and overall improved outcomes. The Australian healthcare system already boasts the infrastructure to switch to routine iCT for complex cases of facial fracture fixation so local institutions should strive to deliver the highest global standards of care.
Patient consent
Patients/guardians have given informed consent to the publication of images and/or data.
Conflict of interest
The authors have no conflicts of interest to disclose.
Funding declaration
The authors received no financial support for the research, authorship, and/or publication of this article.
Revised: August 20, 2023 AEST