Introduction
Between January 2018 and December 2021, the New Zealand Accident Compensation Corporation received 28,901 new claims for maxillofacial fractures, at annual numbers of 7615 (2018), 7483 (2019), 6805 (2020) and 6998 (2021). Despite the drop in claim numbers, the costs per claim increased from NZ$6494.85 to NZ$7860.01 over this period, making maxillofacial fractures a substantial annual cost to the New Zealand health system of NZ$70–80 million.1
We have previously shown interpersonal violence (IPV) to be the most common cause (38%) of maxillofacial fractures in the Wellington Region of New Zealand, with young Māori males being disproportionately affected.2 We concluded that public health strategies similar to those previously implemented to reduce road traffic accidents (RTA) are urgently needed to reduce IPV as the main cause of maxillofacial fractures.2
This study investigated the impact of COVID-19 lockdowns on the causes (including associated alcohol and/or drug use), fracture patterns and management of maxillofacial fractures within the Wellington Region over four years. This period included the two years preceding the global COVID-19 pandemic and the first two years of the pandemic , during which New Zealand experienced multiple lockdowns, including periods with widespread restrictions on the public’s ability to interact socially.3
Methods
Patients referred to the Wellington Regional Plastic, Maxillofacial and Burns Unit at Hutt Hospital from 1 January 2018 to 31 December 2021 were identified from the maxillofacial fracture database. Ethics approval was given by the Central Health and Disability Ethics Committee (Ref 16/CEN/173), with written consent obtained from all patients. Patient demographic data including age, gender, ethnicity, alcohol/drug use, and the cause, pattern and management of maxillofacial fracture, were analysed.
Statistical analysis
Statistical analysis was performed using IBM SPSS Statistics for Windows, Version 28.0 (IBM Corp, Armonk, NY, USA) with p < 0.001 denoting statistical significance. Percentages were compared using chi-squared statistics. To test for ethnicity differences while controlling for age, chi-squared tests were used within each age group. To compare rates, the Open Epi software was used.4
Results
The study included 1281 patients, aged between eight months and 95 years (mean, 39.0 years), of whom 963 (75.2%) were male and 318 (24.8%) were female. There were 714 (55.7%) New Zealand Europeans, 282 (22.0%) Māori, 107 (8.4%) Pasifika, 60 (4.7%) Asians and 118 (9.2%) other ethnicities. Causes of maxillofacial fractures were IPV (37.6%), followed by falls (34.9%), sports (24.0%), RTA (7.7%) and other causes (5.7%).
Demographics and causes of maxillofacial fractures
Table 1 demonstrates the causes of maxillofacial fractures by age. The mean age at presentation was 30.6 years (range, 1–86) for Māori, 43.0 years (range, 2–95) for New Zealand European, 29.4 years (range, 10–66) for Pasifika, 35.1 years (range, 6–89) for Asian and 45.6 years (range, 8–93) for other ethnicities. Of the 495 patients (38.7%) aged 16–30 years, most injuries were caused by IPV (237, 49.2%), followed by sports (153, 49.7%), RTA (37, 37.4%), falls (48, 15.0%) and other causes (20, 27.4%). Those aged > 60 years were the largest group affected by falls (181, 56.7%).
Interpersonal violence was the most common cause in Māori (55.7%), Pasifika (43.0%) and Asians (38.3%), and the second most common cause for New Zealand Europeans (31.0%). Maxillofacial fractures in New Zealand Europeans (31.7%) and other ethnicities (33.1%) were most likely to be caused by falls (Table 2). However, the power of this significant relationship between ethnicity and cause was significantly reduced when age was controlled for. This suggests that the differences for the cause by ethnicity is partially explained by the different age distributions within the ethnicity groups. Over half of the New Zealand Māori, Pasifika and Asian cases were under 30 years of age, while half of the New Zealand European and other ethnicities were over 37 years old.
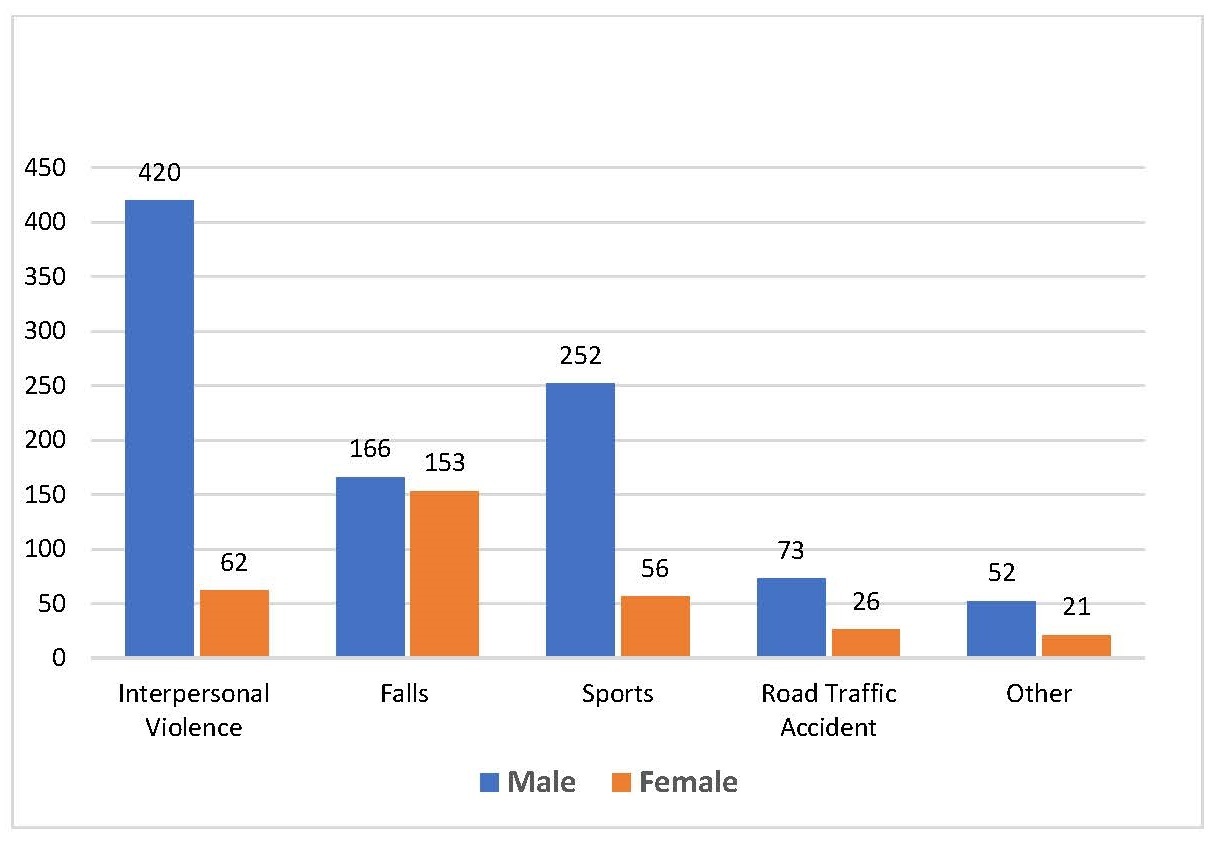
Males of all ethnicities were most likely to present due to IPV (420, 43.6%), sports (252, 26.2%) or falls (166, 17.2%), whereas females were most likely to present due to falls (153, 48.1%), IPV (62, 19.5%) or sports (56, 17.6%) (Figure 1). Males were significantly more likely to present due to IPV while females were significantly more likely to present due to falls (p < 0.001, χ2 = 136.5).
Ethnicity stratification versus 2018 New Zealand Census
The 2018 New Zealand Census shows that Māori make up approximately 16.5 per cent of the general population,5 but they made up 22.0 per cent of all patients presenting with maxillofacial fractures from all causes and 32.6 per cent of those caused by IPV. Asians, who constitute 15.1 per cent of the general population, made up 4.7 per cent of all maxillofacial fracture presentations and 4.8 per cent of those caused by IPV. New Zealand Europeans, who constitute 70.2 per cent of the general population, made up 55.7 per cent of all maxillofacial fractures and 45.9 per cent of those caused by IPV. This indicates that Māori were over-represented within our study and were disproportionately affected by maxillofacial fractures from any cause and especially those involving IPV. Conversely, those identifying as New Zealand Europeans and Asians were under-represented.5
Alcohol and drug use as risk factors
Alcohol and/or drug use was associated with 273 (21.3%) presentations, including those caused by IPV (39.8%), falls (15.0%), RTA (21.2%) and sports (2.6%) (p < 0.001, χ2 = 181.3). Māori (29.8%) and Pasifika (27.1%) were more likely to have alcohol/drug use associated with their presentation compared to New Zealand Europeans (18.8%), while Asians (13.3%) were the least likely to have associated alcohol/drug use (p < 0.001, χ2 = 21.8). Females were statistically less likely to have associated alcohol (11.3%) or drug (< 1%) use compared to males (22.2% and 1.8%, respectively) whose injuries involved alcohol and drugs (p < 0.001). Those aged between 16–30, 31–45 and 46–60 were most likely to be involved with these risk factors (29.3%, 23.4% and 24.1%, respectively).
Causes, maxillofacial fracture patterns and management
Of the 1281 patients with maxillofacial fractures included in the study, 874 (68.0%) had an isolated single-pattern (orbital, midface, mandibular, nasal or skull/skull base) fracture and 407 (32.0%) had mixed-pattern fractures with one patient sustaining panfacial fractures. Orbital (604, 47.4%) and midface (441, 34.4%) fractures were the two most common fracture patterns, 24.0 per cent and 29.3 per cent of these were managed operatively, respectively; the remainder were managed conservatively.
The most common cause of orbital, midface, mandibular and nasal fractures was IPV (37.4%, 33.3%, 58.3% and 31.77%, respectively), whereas skull/skull base fractures were most likely to result from RTA (28.2%). Statistically significant relationships were found between the mechanism of injury and the fracture (midface p < 0.001; mandibular p < 0.001; skull/skull base p < 0.001; nasal p = 0.004) patterns.
Impact of COVID-19 lockdowns on maxillofacial fractures
There were 73 days of COVID-19 Alert Levels 3 and 4 lockdowns in the Wellington Regional Plastic, Maxillofacial and Burns Unit catchment area from 23 March 2020 to 13 May 2020 and 17 August 2021 to 7 September 2021. During these lockdowns, our unit received 33 maxillofacial fracture referrals.3 These were compared to the 1248 referrals received outside the restriction periods, taking into account the number of days in lockdown (or not).3 Significantly fewer maxillofacial fracture referrals were received during the lockdown periods compared to the periods outside lockdown—only 4.5 per 10 person-days compared to 9.0 per 10 person-days (p < 0.001).
Interpersonal violence was less frequent, with a rate of 1.2 per 10 person-days during lockdown periods compared to 3.4 per 10 person-days outside lockdown (p < 0.001). Sports referrals were less common, at a rate of 0.41 per 10 person-days in lockdown versus 2.19 per 10 person-days (p < 0.001) outside lockdown. Falls, RTA and other causes had a similar rate of referral in and out of lockdown. Women were more likely to be referred during lockdown periods, with a referral rate of 1.78 per 10 person-days versus 0.014 per 10 person-days (p < 0.001) out of lockdown. Those older than 60 years of age had a referral rate of 4.2 per 10 person-days in lockdown compared to 1.8 per 10 person-days out of lockdown (p < 0.001). Referral rates were not different in and out of lockdown in any other age group. Referrals with associated alcohol and/or drug use were less frequent in than out of lockdown (0.4 versus 1.9 per 10 person-days, p = 0.003).
Discussion
Our analysis of 1281 patients presenting with maxillofacial fractures to the Wellington Regional Plastic, Maxillofacial and Burns Unit from 1 January 2018 to 31 December 2021 shows that IPV (37.6%) and falls (24.9%) were the most common causes of maxillofacial fractures within our patient population. Māori, who constitute 16.5 per cent of the general population,5 were disproportionately affected, making up 22.0 per cent of the referrals. New Zealand Europeans, who made up 55.7 per cent of the referrals, were more likely to be older than 60 years (25.7%) and presenting due to falls (31.7%). Māori were more likely to be of a younger age with more than 50 per cent under the age of 30 years (59.5%). Interpersonal violence was the leading cause of maxillofacial fractures in Māori (55.7%) and the second most common cause for New Zealand Europeans (31.0%). These findings are consistent with previously published data showing that Māori are disproportionally at risk of adverse health events, including maxillofacial fractures, as the victims of violence. Māori are 2.5 times more likely to die from assault/homicide and Māori females are six times more likely to be hospitalised due to assault/homicide than their non-Māori counterparts,2,6 underscoring that Māori are a vulnerable population at high risk of IPV.
Globally, falls are the most common cause of maxillofacial fractures with Oceania being an exception where IPV is the main cause.7 Our findings of IPV being the most common cause of maxillofacial fractures, accounting for over one-third (37.6%) of all referrals followed closely by falls (24.9%) and sports (24.0%), are consistent with our previous study of the same population showing IPV, falls and sports accounting for 39.0 per cent, 23.8 per cent and 22.8 per cent of maxillofacial fractures, respectively.2
Consistent with our previous study,2 our current study shows an ongoing decrease of RTA as a cause of maxillofacial fractures, accounting for 6 per cent of cases referred to our unit. Sustained national efforts by both the New Zealand Government and the National Transport Agency to reduce road tolls have had a positive impact in reducing serious RTA with Ministry of Transport data (2017–2020) showing deaths and injuries per 100,000 population have remained stable with a slight downward trend.5,8
Alcohol and drugs were implicated in 21.3 per cent of maxillofacial fractures from all causes, with males (24.4%) and those aged 16–30, 31–45 and 46–60 (29.3%, 23.4% and 24.1%, respectively) most likely to be associated with these risk factors. The New Zealand Ministry of Transport reports that between 2019 and 2021, risk factors such as drugs and alcohol contributed to 11 per cent of serious RTA.9 Our study shows a significantly higher rate of these risk factors associated with maxillofacial fractures, likely contributing to our high IPV rates. As these risk factors are self-reported, these rates are likely to be underestimated.
The two lockdown periods affecting our patient population during 2020 and 2021 showed an increase in both the rates of females and older patients being referred with maxillofacial fractures. Both IPV and sports showed significantly reduced referral rates during lockdown, while falls, RTA and other were referred at a similar rate as out of lockdown. Referrals associated with alcohol/drug use were less frequent during the lockdowns. Females were more likely to be referred during lockdown, with a referral rate of 1.78 versus 0.014 per 10 person-days (p < 0.001). This increase in proportion is likely related to the reduction in cases caused by IPV, with males accounting for 84.8 per cent of all presentations caused by IPV. It may result from the fact that females make up a much larger proportion of the > 60 years of age population, with the 2018 Census indicating that for every 100 females > 65 years of age there are only 87 males, compared to those aged 15–29 years being 104 males to 100 females.10
Conclusion
Despite our previous recommendation of a targeted national health intervention to address maxillofacial fractures caused by IPV,2 this study has demonstrated that IPV remains the most common cause of maxillofacial fracture that poses a significant burden on the national health system.
Patient consent
Patients/guardians have given informed consent to the publication of images and/or data.
Conflicts of interest
The authors have no conflicts of interest to disclose.
Financial support and sponsorship
The authors received no financial support for the research, authorship, and/or publication of this article.
Disclosures
This paper was presented, in part, at the National Trauma Symposium, 27 September 2022; and the Joint Scientific Meeting of the New Zealand Association of Plastic Surgeons and the New Zealand Society for Surgery of the Hand, 1–3 December 2022, Wellington, New Zealand.
Revised: September 12, 2023 AEST